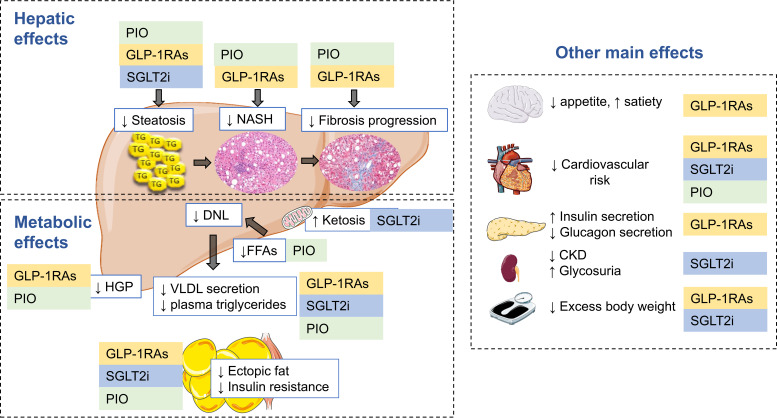
Figure 1.
Hepatic and metabolic effects of pioglitazone, GLP-1 receptor agonist, and SGLT2 inhibitor therapy in NAFLD. People with type 2 diabetes and NAFLD share common pathophysiological mechanisms, among which insulin resistance plays a central role. Excess energy intake and sedentarism promote weight gain that exacerbates potential genetic traits for insulin resistance. Dysfunctional, insulin-resistant adipose tissue promotes excess lipolysis and flow of FFA flux to the liver, increasing de novo lipogenesis (DNL) and intrahepatic triglyceride accumulation (simple steatosis), which, by a number of mechanisms, may progress over time to NASH, fibrosis, and eventually cirrhosis. Hepatic insulin resistance leads to excess hepatic glucose production (HGP), which, with dysfunctional pancreatic β-cell function, will lead to hyperlgycemia. Pioglitazone (PIO), GLP-1 receptor agonists (GLP-1RAs) and SGLT2 inhibitors (SGLT2i) are effective in treating hyperglycemia, reducing cardiovascular risk, and conferring multiple hepatic benefits in NAFLD. Pioglitazone is also a potent insulin sensitizer that restores the normal biology of adipose tissue and its response to insulin, which translates into increases in plasma adiponectin and reduction in FFA flux to the liver. GLP-1 receptor agonists reduce appetite, promote glucose-dependent insulin secretion, restore normal glucagon secretion, and have many pleiotropic metabolic and vascular effects. Both pioglitazone and GLP-1 receptor agonists decrease hepatic glucose production and improve plasma lipid metabolism. SGLT2 inhibitors promote glycosuria and a state of ketosis that induces moderate weight loss with metabolic improvement and cardiorenal protection. CKD, chronic kidney disease; TG, triglycerides; VLDL, very-low-density lipoprotein cholesterol. This figure includes pictures from Servier Medical Art used under a Creative Commons Attribution 3.0 Unported License (https://creativecommons.org/licenses/by/3.0).