Abstract
Background:
Sleep disturbance is associated with broadband measurements of emotion regulation (ER). The linkage between ER, a multidimensional process, and suicidal ideation and suicide attempt is also documented in theoretical and empirical work. Recent research indicates that distinct profiles of ER are associated with psychiatric outcomes, including adolescent suicidal ideation and attempt. The present study examined whether specific domains of ER would explain the association between sleep disturbance, and ideation and attempt among psychiatrically hospitalized adolescents.
Method:
The sample included 284 adolescents who completed self-report measures on sleep disturbance, ER, suicidal ideation, suicide attempt, and psychiatric symptoms upon inpatient hospitalization.
Results:
Findings indicated that sleep disturbance was associated with suicidal ideation. Further, a single ER domain (perceived limited access to ER strategies) fully accounted for the significant association between sleep disturbance and suicidal ideation. A reported suicide attempt in the past week was correlated with the nonacceptance of emotional responses, perceived limited access to ER strategies, and emotional clarity, but was not associated with sleep disturbance.
Discussion:
The current findings highlight the importance of examining narrowband ER and indicate the presence of differential associations between sleep disturbance, ER, and suicide-related outcomes. Findings further elucidate the possible role of impaired cognitive responses to emotional experiences in the co-occurrence of sleep disturbance and youth psychiatric outcomes.
Keywords: child and adolescent mental health, emotion regulation, suicide
1 |. INTRODUCTION
Sleep disturbance, defined as self-reported sleep quality deficits, is one sleep health parameter associated with impaired socioemotional functioning (Simon et al., 2020). For instance, sleep restriction and reported sleep disturbance were associated with negative mood states and reduced positive affectivity across the lifespan (Difrancesco et al., 2021; Parsons et al., 2022; Tamm et al., 2019). Converging evidence indicates that reported sleep disturbance is a risk factor for a broad range of psychiatric outcomes including anxiety disorders, depression (Freeman et al., 2020), and suicidality (Goldstein & Franzen, 2020; Kearns et al., 2020; Liu et al., 2020; Pigeon et al., 2012), particularly evidenced in adolescent populations (Lovato & Gradisar, 2014; Rapee et al., 2019; Scott et al., 2021). A common factor involved in the association between sleep disturbance and psychiatric outcomes is emotion regulation (ER; O’Leary et al., 2017). Given the bioregulatory risk window of adolescence (Carskadon, 2011), further research is needed on the possible explanatory role of ER in the association between sleep disturbance and youth psychiatric outcomes, particularly in acute clinical populations (Palmer & Alfano, 2017). Given the rise in suicide among adolescents in recent years (Garnett et al., 2022), understanding how ER may impact the link between sleep disturbance and suicide-related outcomes may be critically important for youth suicide prevention efforts.
1.2 |. Sleep disturbance and ER
ER is described as a transdiagnostic, multidimensional process involving the ability to monitor, evaluate, and respond to emotional experiences (Gratz & Roemer, 2004; Gross, 1998). Sleep disturbance can adversely impact the cognitive processing and functioning that are required for effective ER. In youth specifically, self-reported sleep disturbance is associated with key factors aligned with impaired ER, including mood disturbances, poor behavioral control, and decreased neurocognitive functioning (Dahl, 1996; Kheirandish & Gozal, 2006; Sadeh, 2007). Research has focused on the association between sleep and broadband measures of ER (Kirschbaum-Lesch et al., 2021; O’Leary et al., 2017; Wall et al., 2020; Weis et al., 2015), including ER measures used to yield an aggregate, unitary ER scale or measures with limited delineation (i.e., positive vs. negative ER strategies). Research examining the association between sleep disturbance and specific ER domains is limited. Of note, there is a need to examine more nuanced, specific associations involving ER in clinically acute populations (e.g., psychiatrically hospitalized youth) given that such populations experience pronounced sleep disturbances (Boafo et al., 2019; Thompson et al., 2020) and emotion dysregulation (Perez et al., 2012).
1.3 |. ER, suicidal ideation, and suicide attempt
A taxonomy involving six domains of ER difficulties has been described and examined in empirical research (Gratz & Roemer, 2004) and namely identifies the domains as (1) nonacceptance of emotional responses, (2) difficulty engaging in goal-directed behavior during emotional distress, (3) impulse control difficulties during emotional distress, (4) emotional awareness, (5) perceived limited access to ER strategies, and (6) lack of emotional clarity. Examination of these six domains (not simply broadband ER) reveals differential associations with sociodemographic and clinical variables, such as substance use, eating behaviors, and parental risk factors (e.g., Brockmeyer et al., 2014; Faulkner et al., 2020; Miragoli et al., 2020). This highlights the need to explore specific ER domains in relation to clinically relevant symptoms and markers of psychopathological development.
ER is closely aligned with suicide-related outcomes (Colmenero-Navarrete et al., 2021) and their treatment (Miller et al., 2007). Using the dimensional framework of ER (Gratz & Roemer, 2004), research on adolescents who were followed after psychiatric hospitalization indicated that two ER domains predicted chronic suicidal ideation: perceived limited access to ER strategies and nonacceptance of emotional responses (Wolff et al., 2018). Similarly, previous studies involving psychiatrically hospitalized adolescents found that after controlling for sociodemographic factors and psychiatric symptoms, there was a concurrent association between limited access to ER strategies and suicidal ideations (Hatkevich et al., 2019). Similarly, perceived access to ER strategies was the strongest correlate of suicidal ideation among community adolescents (Brausch et al., 2022). Research involving adults with depression also supports differential associations, such that suicide attempt status was associated only with the dimensions of impulse control difficulties during distress and emotional clarity (Neacsiu et al., 2018). This suggests there are distinct ER profiles for suicidal ideation and attempts. Whether distinct ER domains explain the association between sleep disturbance and suicide-related outcomes has not yet been explored and represents a gap in the literature.
1.4 |. Current study
The present study examined whether self-reported sleep disturbance, suicidal ideation, and suicide attempts were associated among psychiatrically hospitalized adolescents and whether ER domains differentially explained the association between sleep disturbance, and suicidal ideation and suicide attempt (see conceptual model, Figure 1).
FIGURE 1.
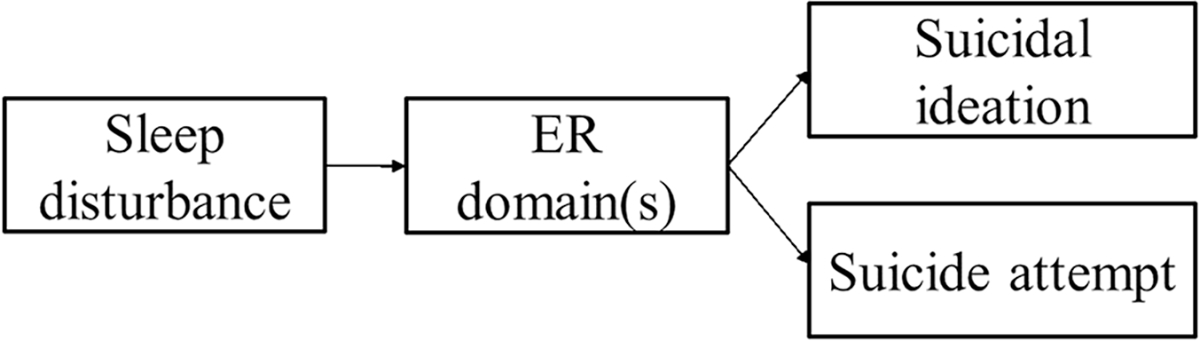
Conceptual model. ER, emotion regulation.
Hypothesis 1.
Higher levels of sleep disturbance and deficits in ER domains will be associated with higher levels of suicidal ideation in bivariate analyses.
Hypothesis 2.
Higher levels of sleep disturbance and deficits in ER domains will be associated with the endorsement of a recent suicide attempt in bivariate analyses.
Hypothesis 3.
Sleep disturbance will be indirectly associated with suicidal ideation via ER. Given prior literature, it was expected that the “perceived access to ER strategies” domain would be the primary explanatory variable.
Hypothesis 4.
The association between sleep disturbance and suicide attempts will be explained in part by ER. In accord with prior research, it was expected that ER aligned with behavioral control (i.e., impulse control during distress) would be the primary explanatory domain.
2 |. METHOD
2.1 |. Participants and procedures
This chart review study was approved by the hospital’s institutional review board. The study sample consisted of adolescent patients admitted to an inpatient unit at a children’s psychiatric hospital in a northeastern US metropolitan area.
Adolescents were administered an assessment battery of self-report measures as a part of clinical intake upon admission to the psychiatric unit. The current data was compiled from chart review of clinical intakes, which occurred between November 5, 2020 and September 15, 2021. Records were selected for adolescents who completed any portion of the intake battery during the time frame. There were 284 adolescents (68% assigned females at birth) who ranged in age from 11 to 18 years (M = 15.17, SD = 1.71) and identified themselves as White (54%), Black (14%), Asian (3%), or multiracial (17%). In terms of ethnicity, 25% identified as Hispanic. The number of previous inpatient hospitalizations for mental health reasons ranged from 0 to 9 (M = 0.92, SD = 1.63).
2.2 |. Measures
2.2.1 |. Sleep disturbance
The PROMIS Sleep Disturbance 8-item self-report questionnaire (Yu et al., 2012) assesses perceived sleep quality and satisfaction, sleep restoration, and difficulty falling asleep and staying asleep. Prior research supports scale convergent validity with well-established sleep self-report measures (Yu et al., 2012) and is moderately correlated with objective measurement in youth (Hanish et al., 2017). To determine the proportion of adolescents with elevated sleep disturbance in the current sample, the percentage of those with a T-score of 60 or above (1 SD about the general population mean; Yu et al., 2012) was calculated. Internal reliability in the current study was McDonald’s ω = 0.92.
2.2.2 |. Suicidal ideation
The Suicidal Ideation Questionnaire-Junior (SIQ-JR; Reynolds & Mazza, 1999) is a 15-item assessment of suicidal ideation. The SIQ-JR utilizes Likert-type items with responses ranging from 0 (I’ve never had this thought) to 7 (Almost every day). Responses were summed to create a total score. Internal reliability in the current sample was ω = 0.97.
2.2.3 |. Recent suicide attempt
Youth were asked, “Have you made any suicide attempts in the 7 days before you came to the hospital?” Responses were coded as a binary variable (yes [1], no [0]).
2.2.4 |. ER
The Difficulties in Emotion Regulation Scale (DERS-SF) (Gratz & Roemer, 2004) assessed six domains of ER via 18 Likert-type items with responses ranging from 1 (Almost never) to 5 (Almost always). Items in the six domains in the DERS include the following: perceived limited access to ER strategies (three items; e.g., “When I’m upset, I believe there is nothing I can do to make myself feel better”; ω = 0.87); nonacceptance of emotional responses (three items; e.g., “When I’m upset, I become irritated at myself for feeling that way”; ω = 0.88); impulse control difficulties during distress (three items; e.g., “When I’m upset, I lose control over my behavior”; ω = 0.93); difficulties engaging in goal-directed behavior during distress (three items; e.g., “When I’m upset, I have difficulty getting work done”; ω = 0.94); emotional awareness (three items; e.g., “I pay attention to how I feel”; ω = 0.87); and lack of emotional clarity (three items; e.g., “I am confused about how I feel”; ω = 0.87). Responses were summed for each domain. The individual DERS domains have adequate internal reliability in prior research (Neumann et al., 2010) and have been used to assess specific ER in in various populations (e.g., Fowler et al., 2014; Giromini et al., 2012; Lee et al., 2012), including community (Brausch et al., 2022; Neumann et al., 2010) and clinical samples of adolescents (Hatkevich et al., 2019; Wolff et al., 2019).
2.2.5 |. Internalizing symptoms
The internalizing subscale of the Pediatric Symptom Checklist–Youth Form (Gardner et al., 1999) assessed internalizing symptoms (anxiety and depressive symptoms) via 5 Likert-type items ranging from 0 (Never) to 2 (Often). Items include: “Feel sad, unhappy” and “Worry a lot,” and items were summed to create a total score.
2.3 |. Data analysis
Missing data due to skipped items occurred at a low frequency for all measures: suicidal ideation (0%), suicide attempt (0%), ER subscales (4.9%), sleep disturbance (2.4%), and internalizing symptoms (1.7%). Missing data were estimated using multivariate imputation by chained equations (van Buuren & Groothuis-Oudshoorn, 2011). Bivariate associations between variables in the conceptual model and youth age, sex assigned at birth, ethnicity, and internalizing symptoms were evaluated for possible inclusion as covariates. Age, sex, and internalizing symptoms were significantly correlated with multiple variables in the conceptual model and were therefore included as covariates in the data analyses. A series of indirect effects models on the association between sleep disturbance and each suicide outcome (ideation and attempt) via each of the six ER domains were examined. Indirect effects analyses were tested using causal mediation (Tingley et al., 2014). For suicide attempt we used a generalized linear model with logit link function and binomial distribution and for all other mediators and outcomes we used a general linear model. Unstandardized indirect effects and nonparametric 95% confidence intervals (95% CIs) were generated using 1000 bootstrapped samples. Results from causal mediation are unbiased if the assumptions of no unmeasured confounding and temporal order are satisfied (VanderWeele, 2016). For this study, we included important potential confounders (age, sex, and internalizing symptoms) in the modeling. Temporal order may be suspect given the cross-sectional design and the potential for bidirectional relationships among sleep, ER, and suicidal ideation and behavior. That said, recent findings using momentary ecological assessment of sleep and suicidal ideation point to unidirectionality of self-reported sleep disturbance leading to subsequent suicidal ideation in adults (Littlewood et al., 2019). The following R packages were used in analysis: mice v3.14, mediation v4.50, stats v3.6.
3 |. RESULTS
Means, SDs, and correlation coefficients between variables are presented in Table 1, and partial correlation coefficients accounting for study covariates are presented in Table 2. There were 52 adolescents who endorsed the suicide attempt probe. Descriptive statistics of all study variables, stratified and contrasted by suicide attempt status, are presented in Table 3. In this sample, 40% of adolescents reported sleep disturbance at the level of T-score > 60. Tables 4 and 5 present the bootstrapped indirect effect estimates for each of the models with suicide attempt and suicidal ideation as outcomes.
TABLE 1.
Means of, SDs of, and correlations between study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. SA | - | - | - | - | - | - | - | - | - | - | - | - |
| 2. SI | 0.25* | - | - | - | - | - | - | - | - | - | - | - |
| 3. Sleep | 0.09 | 0.25* | - | - | - | - | - | - | - | - | - | - |
| 4. Nonacc | 0.18* | 0.61* | 0.34* | - | - | - | - | - | - | - | - | - |
| 5. Strategy | 0.20* | 0.65* | 0.41* | 0.65* | - | - | - | - | - | - | - | - |
| 6. Impulse | −0.002 | 0.20* | 0.19* | 0.27* | 0.50* | - | - | - | - | - | - | - |
| 7. Goals | 0.06 | 0.49* | 0.29* | 0.56* | 0.62* | 0.48* | - | - | - | - | - | - |
| 8. Aware | 0.01 | −0.27* | −0.15* | −0.17* | −0.26* | −0.25* | −0.13* | - | - | - | - | - |
| 9. Clarity | 0.13* | 0.46* | 0.25* | 0.57* | 0.44* | 0.24* | 0.43* | −0.19* | - | - | - | - |
| 10. Int. | 0.20* | 0.75* | 0.36* | 0.70* | 0.71* | 0.29* | 0.60* | −0.20* | 0.52* | - | - | - |
| 11. Age | −0.03 | −0.16* | −0.04 | −0.11 | −0.17* | −0.22* | −0.07 | 0.28* | −0.10 | −0.10 | - | - |
| 12. Sex | 0.11 | 0.31* | 0.15* | 0.20* | 0.24* | 0.03 | 0.14* | −0.13* | 0.14* | 0.25* | −0.11 | - |
| Mean | - | 39.75 | 26.58 | 8.23 | 8.46 | 6.76 | 10.20 | 8.08 | 7.92 | 6.51 | 15.17 | - |
| Range | - | 0–90 | 4–40 | 0–15 | 1–15 | 0–15 | 2–17 | 2–17 | 0–15 | 0–10 | 11.3–18.9 | - |
| SD | - | 27.48 | 7.78 | 4.20 | 3.63 | 3.55 | 4.02 | 3.63 | 3.86 | 2.80 | 1.72 | - |
Note: Aware, emotional awareness; Clarity, lack of emotional clarity; Goals, difficulty engaging in goal-directed behavior during emotional distress; Impulse, impulse control difficulties during emotional distress; Sleep, sleep disturbance; Strategy, perceived limited access to ER strategies.
Abbreviations: ER, emotion regulation; Int., internalizing symptoms; Nonacc, nonacceptance of emotional responses; SA, suicide attempt within past 7 days; SI, suicidal ideation.
p < 0.05.
TABLE 2.
Partial correlations between study variables controlling for age, sex, and internalizing symptoms.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. SA | - | - | - | - | - | - | - | - | - |
| 2. SI | 0.15* | - | - | - | - | - | - | - | - |
| 3. Sleep | −0.01 | −0.04 | - | - | - | - | - | - | - |
| 4. Nonacc | 0.05 | 0.17* | 0.13* | - | - | - | - | - | - |
| 5. Strategy | 0.07 | 0.22* | 0.24* | 0.30* | - | - | - | - | - |
| 6. Impulse | −0.06 | −0.04 | 0.10 | 0.11 | 0.43* | - | - | - | - |
| 7. Goals | −0.08 | 0.08 | 0.11 | 0.26* | 0.37* | 0.40* | - | - | - |
| 8. Aware | 0.06 | −0.14* | −0.09 | −0.04 | −0.15* | −0.18* | −0.02 | - | - |
| 9. Clarity | 0.03 | 0.11 | 0.08 | 0.34* | 0.11 | 0.10 | 0.18* | −0.09 | - |
Note: Aware, emotional awareness; Clarity, lack of emotional clarity; Goals, difficulty engaging in goal-directed behavior during emotional distress; Impulse, impulse control difficulty during emotional distress; Sleep, sleep disturbance; Strategy, perceived limited access to ER strategies.
Abbreviations: ER, emotion regulation; Nonacc, nonacceptance of emotional responses; SA, suicide attempt within past 7 days; SI, suicidal ideation.
p < 0.05.
TABLE 3.
Study variables by suicide attempt status.
| No suicide attempt | Endorsed suicide attempt | t | p | |
|---|---|---|---|---|
| (n = 232) | (n = 52) | |||
| M (SD) | M (SD) | |||
| Sleep disturbance | 26.25 (7.97) | 28.04 (6.71) | −1.67 | 0.09* |
| Suicidal ideation | 36.50 (27.8) | 54.37 (20.40) | −5.32 | <0.001** |
| Nonacceptance | 7.87 (4.14) | 9.82 (4.17) | −3.06 | 0.003** |
| Perceived limited access to strategies | 8.13 (3.48) | 9.94 (3.40) | −3.46 | <0.001** |
| Impulse control difficulty | 6.77 (3.57) | 6.75 (3.45) | 0.03 | 0.97 |
| Goal-directed behavior difficulty | 10.09 (4.09) | 10.67 (3.64) | −1.02 | 0.31 |
| Emotional awareness | 8.07 (3.62) | 8.14 (3.69) | −0.12 | 0.91 |
| Lack of clarity | 7.68 (3.78) | 8.97 (4.04) | −2.10 | 0.03** |
p < 0.10;
p < 0.05.
TABLE 4.
Indirect effects estimates and nonparametric bootstrap CIs (suicide attempt outcome).
| ER domain | Estimate | 95% Lower CI | 95% Upper CI | p |
|---|---|---|---|---|
| Nonacceptance | 0.0002 | −0.0007 | 0.001 | 0.59 |
| Perceived limited access to strategies | 0.0007 | −0.0008 | 0.002 | 0.31 |
| Impulse control difficulties | −0.0003 | −0.002 | 0.0002 | 0.37 |
| Goal-directed behavior difficulty | −0.0005 | −0.002 | 0.0002 | 0.21 |
| Emotional awareness | −0.0002 | −0.001 | 0.0003 | 0.45 |
| Lack of clarity | 0.00009 | −0.0006 | 0.0009 | 0.82 |
Note: Outcome, suicide attempt; Predictor, sleep; Covariates, age, sex, internalizing symptoms.
Abbreviations: CI, confidence interval; ER, emotion regulation.
TABLE 5.
Indirect effects estimates and nonparametric bootstrap CIs (suicidal ideation outcome).
| ER domain | Estimate | 95% Lower CI | 95% Upper CI | p |
|---|---|---|---|---|
| Nonacceptance | 0.058 | −0.0002 | 0.14 | 0.05 |
| Perceived limited access to strategies | 0.142 | 0.06 | 0.25 | <0.001* |
| Impulse control difficulties | −0.009 | −0.06 | 0.03 | 0.56 |
| Goal-directed behavior difficulty | 0.023 | −0.01 | 0.08 | 0.16 |
| Emotional awareness | 0.031 | −0.01 | 0.09 | 0.14 |
| Lack of clarity | 0.024 | −0.01 | 0.08 | 0.22 |
Note: Outcome, suicidal ideation; Predictor, sleep; Covariates, age, sex, internalizing symptoms.
Abbreviations: CI, confidence interval; ER, emotion regulation.
Statistically significant indirect effect at p < 0.05.
Hypothesis 1.
Suicidal ideation was correlated with all variables in the conceptual model and in the expected direction, including ER domains and sleep disturbance.
Hypothesis 2.
Recent suicide attempt was correlated with the nonacceptance, strategy, and clarity ER domains in the expected direction. After accounting for internalizing symptoms, age, and gender, there was a minimal association between sleep disturbance and suicide attempt (r = −0.01), and minimal associations between the ER scales and suicide attempt (r ranging from −0.08 to 0.07).
Hypothesis 3.
Within the association between sleep disturbance and suicidal ideation, there was a statistically significant indirect effect only for the perceived limited access to ER strategies domain (Est.: 0.14, 95% CI: 0.06–0.25, p < 0.001) and no significant direct effect. That is, higher sleep disturbance was associated with higher suicidal ideation, and this association was explained by the attribution that one’s access to ER strategies is limited.
Hypothesis 4.
There were no statistically significant indirect effects of sleep disturbance on suicide attempt via any of the ER domains.
The R causal mediation analysis package requires mediator and outcome regression analyses as inputs to calculate the average indirect effect. These regression analyses are presented for the analysis that included the perceived access to ER strategies domain in Table 6. In ancillary analysis, the indirect effects model including the perceived access to ER strategies domain was examined, excluding all covariates (age, sex, internalizing symptoms), and statistical conclusions remained the same.
TABLE 6.
Mediator and outcome regression analyses.
| Model | Est. | SE | t | p |
|---|---|---|---|---|
| Outcome: Strategy [R2 = 0.544., p < 0.001] | ||||
| Age | −0.156 | 0.078 | −2.010 | 0.045* |
| Sex | 0.402 | 0.322 | 1.248 | 0.213 |
| Internalizing symptoms | 0.792 | 0.056 | 14.174 | <0.001* |
| Sleep disturbance | 0.080 | 0.020 | 4.082 | <0.001* |
| Outcome: Suicidal ideation [R2 = 0.612, p < 0.001] | ||||
| Age | −0.977 | 0.564 | −1.733 | 0.084 |
| Sex | 6.907 | 2.325 | 2.971 | 0.003* |
| Internalizing symptoms | 5.668 | 0.526 | 10.771 | <0.001* |
| Sleep disturbance | −0.234 | 0.145 | −1.610 | 0.108 |
| Strategy | 1.777 | 0.429 | 4.144 | <0.001* |
Note: Strategy, perceived limited access to ER strategies subscale. All equations included a constant.
Abbreviation: ER, emotion regulation.
Statistically significant t value.
4 |. DISCUSSION
The current study examined associations between self-reported sleep disturbance, ER domains, suicidal ideation, and suicide attempt among psychiatrically hospitalized adolescents. As expected, sleep disturbance was associated with suicidal ideation. Further, the association between sleep disturbance and suicidal ideation was explained by perceived limited access to ER strategies, after accounting for the effect of internalizing distress and demographic variables. However, there were minimal associations between recent suicide attempt and ER domains or sleep disturbance.
Contemporary explanatory models of suicide delineate distinct pathways to suicidal ideation and attempt (e.g., Klonsky & May, 2015; Van Orden et al., 2010), highlighting the significance of parsing associations with each outcome. The current study indicates that, among psychiatrically hospitalized adolescents, sleep disturbance may be indirectly associated with suicidal ideation by way of ER (specifically, perceived limited access to ER strategies). This finding is consistent with converging evidence that self-reported sleep disturbance and suicidal ideation are linked beyond the influence of internalizing distress (Harris et al., 2020), and prior literature demonstrating this association among general psychiatric inpatient samples (Kaplan et al., 2014; Shepard et al., 2022). Sleep disturbances may be more evident among adolescent psychiatric patients with a clinical profile involving suicidal ideation compared to patients with other profiles. Such profiles of co-occurring sleep disturbances and suicidality are consistent with research indicating the presence of marked agitated states (Ribeiro et al., 2015; Rogers et al., 2016) nighttime hyperarousal (Dolsen et al., 2017; Kalmbach et al., 2021) and sleep architecture abnormalities (e.g., reduced slow wave sleep; Boafo et al., 2019; Shahid et al., 2012) among individuals experiencing suicidality.
Evidence indicates that specific sleep health parameters (i.e., delayed sleep onset, rest-activity irregularity) are associated with poor behavioral control and mood instability (Gillett et al., 2021), key constructs conceptually aligned with a suicide attempt. The current study did not find an association between one index of sleep, self-reported sleep disturbance, and recent suicide attempt. These null findings, however, should be cautiously interpreted with attention to methodological and clinical considerations relevant to suicide attempts in the current sample. The full scope of active suicidal behavior may not have been captured by self-report of recent suicide attempt. Other behaviors may be important markers of active suicidality, including multi-informant measurement of behavior related to suicide method access (e.g., accumulating medication), partial completion of a suicidal plan (e.g., interrupted/aborted suicide attempts), and ancillary suicidal preparations (e.g., communicating suicide notes). The current reliance on self-report of suicide attempt in the current study also precludes examination of self-injury with serious medical implications that is embedded within suicidal ambivalence. Beyond assessment of active suicidality, the sample was drawn from a general inpatient psychiatric population which may have obscured the association between sleep disturbance and active suicidality. For example, among psychiatric adolescent inpatients, it is not uncommon to have a clinical presentation involving a thwarted imminent suicide attempt, possibly by caregiver or peer intervention (Hill et al., 2017). Patients hospitalized following a thwarted attempt would likely have a similar profile of sleep disturbance, ER, and ideation as those who were hospitalized following a recent attempt, making it difficult to distinguish those who reported a recent attempt from those who did not given the information we collected. Distinguishing among such subpopulations would likely require more robust assessment of sleep and circadian patterns over time and assessment of additional indices of active suicidal behavior including instrumental suicidal behavior, suicidal behavior with ambivalent suicidal intent, and thwarted suicide attempt.
These results are consistent with the explanatory role of perceived access to ER strategies and potentially nonacceptance of emotional distress (given the trend with significance level of p = 0.05). One possibility to be examined in future prospective research is that sleep disturbance may impair cognitive responses to emotional experience. This possible effect would be in agreement with research suggesting that complex problem-solving, like that required for ER, is fostered by intact sleep architecture (Lewis et al., 2018) and sleep restriction impairs creative and innovative cognition (Killgore, 2010). Further, the current results on possible indirect effects are consistent with the mindfulness-based conceptualization wherein cognitive reactivity (e.g., the activation of negative cognitive attributions about emotional experiences) is posited to be a precipitating and perpetuating factor involved in suicidal ideation (Williams et al., 2006). Further prospective research will help determine whether adolescents experiencing sleep disturbance, in the context of marked stressors characteristic of adolescents requiring psychiatric hospitalization, have constrained ability to generate novel, flexible, nonreactive strategies for responding to their emotional experiences.
Reduction of suicidal ideation is critical as this indicator of severe distress is associated with negative transdiagnostic outcomes and is often a precipitant of psychiatric hospitalization. The current findings suggest opportunities to examine high-acuity treatment configurations targeting both sleep disturbance and ER. Current treatment strategies appropriate for inpatient or recently hospitalized adolescents, like dialectical behavior therapy, target skills conducive to sleep promotion and ER (Miller et al., 2007). However, it is unclear whether any intensive treatment approaches are effective in reducing levels of sleep disturbance in psychiatric inpatients or those recently hospitalized; research indicates that treatment-as-usual does not result in the remission of sleep disturbances in psychiatrically hospitalized individuals (Schennach et al., 2019). There is also the possibility that inpatient psychosocial interventions could target adolescents’ cognitive attributions about emotional experiences, namely enhancing self-efficacy beliefs and non-reactivity in the context of emotional distress. Given that sleep disturbance likely limits the capacity of patients to learn and implement skills related to ER, it is possible that both intervention targets may need to be addressed for benefits to be realized. Collectively, there is a need for clinical research on the optimization of high acuity treatment, including psychosocial treatment configurations that explicitly promote both sleep health and specific ER domains.
The current findings should be considered in light of the study limitations. First, the study employed a cross-sectional design which limits conclusions about temporal associations and causality. Results are unbiased if the assumptions of no unmeasured confounding and temporal ordering depicted in Figure 1 are satisfied. The temporal ordering is the most challenged in the current study as the assessments were cross-sectional and there are likely bidirectional relaitonships and/or dynamic complexity (e.g., suicidal ideation leading to disruptions in sleep–wake patterns; bidirectional associations between internalizing distress and sleep-related outcomes; idiographic differences). Future research will benefit from high-resolution momentary assessments of the current study variables over a longer period. Second, the current study did not directly account for other domains of sleep health (e.g., timing, duration, regularity) that may be linked to ER and suicide outcomes. Third, the current study focused on a single psychiatric inpatient facility which tempers generalizability to other settings. Fourth, psychiatrically hospitalized adolescents may underreport symptoms due to a motivation to express discharge readiness and/or due to social desirability. Such limitations should be considered in the collective need for further research exploring the psychosocial constructs related to sleep health and ER domains amongst high acuity populations.
Sleep disturbance was cross-sectionally associated with suicidal ideation, and the relation between sleep disturbance and suicidal ideation was explained by perceived limited access to ER strategies. Findings are consistent with the explanatory role of specific ER strategies contributing to suicide-related distress, emphasizing the need to better understand and intervene on sleep disturbance and ER skills, particularly with respect to bolstering ER repertoires and self-efficacy, to mitigate suicide risk among vulnerable adolescents.
ACKNOWLEDGMENTS
Research reported in this publication was supported by the COBRE Center for Sleep and Circadian Rhythms in Child and Adolescent Mental Health funded by the NIGMS grant number P20GM139743. Victor Buitron was supported by the NIH FIRST award number U54CA267730 with funding from the Office of the Director at NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding information
COBRE Center for Sleep and Circadian Rhythms in Child and Adolescent Mental Health funded by the NIGMS, Grant/Award Number: P20GM139743; Victor Buitron was supported by the NIH FIRST, Grant/Award Number: U54CA267730
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Boafo A, Armitage R, Greenham S, Tavakoli P, Dale A, Nixon A, Lafrenière A, Ray LB, De Koninck J, & Robillard R (2019). Sleep architecture in adolescents hospitalized during a suicidal crisis. Sleep Medicine, 56, 41–46. 10.1016/j.sleep.2018.12.018 [DOI] [PubMed] [Google Scholar]
- Brausch AM, Clapham RB, & Littlefield AK (2022). Identifying specific emotion regulation deficits that associate with nonsuicidal self-injury and suicide ideation in adolescents. Journal of Youth and Adolescence, 51(3), 556–569. 10.1007/s10964-021-01525-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockmeyer T, Skunde M, Wu M, Bresslein E, Rudofsky G, Herzog W, & Friederich H-C (2014). Difficulties in emotion regulation across the spectrum of eating disorders. Comprehensive Psychiatry, 55(3), 565–571. 10.1016/j.comppsych.2013.12.001 [DOI] [PubMed] [Google Scholar]
- Carskadon MA (2011). Sleep in adolescents: The perfect storm. Pediatric Clinics of North America, 58(3), 637–647. 10.1016/j.pcl.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colmenero-Navarrete L, García-Sancho E, & Salguero JM (2022). Relationship between emotion regulation and suicide ideation and attempt in adults and adolescents: A systematic review. Archives of Suicide Research, 26, 1702–1735. 10.1080/13811118.2021.1999872 [DOI] [PubMed] [Google Scholar]
- Dahl RE (1996). The impact of inadequate sleep on children’s daytime cognitive function. Seminars in Pediatric Neurology, 3(1), 44–50. 10.1016/S1071-9091(96)80028-3 [DOI] [PubMed] [Google Scholar]
- Difrancesco S, Penninx BWJH, Antypa N, van Hemert AM, Riese H, & Lamers F (2021). The day-to-day bidirectional longitudinal association between objective and self-reported sleep and affect: An ambulatory assessment study. Journal of Affective Disorders, 283, 165–171. 10.1016/j.jad.2021.01.052 [DOI] [PubMed] [Google Scholar]
- Dolsen EA, Cheng P, Arnedt JT, Swanson L, Casement MD, Kim HS, Goldschmied JR, Hoffmann RF, Armitage R, & Deldin PJ (2017). Neurophysiological correlates of suicidal ideation in major depressive disorder: Hyperarousal during sleep. Journal of Affective Disorders, 212, 160–166. 10.1016/j.jad.2017.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner P, Dean AC, Ghahremani DG, & London ED (2020). Neural basis of smoking-related difficulties in emotion regulation. International Journal of Neuropsychopharmacology, 23(7), 409–416. 10.1093/ijnp/pyaa015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler JC, Charak R, Elhai JD, Allen JG, Frueh BC, & Oldham JM (2014). Construct validity and factor structure of the difficulties in emotion regulation scale among adults with severe mental illness. Journal of Psychiatric Research, 58, 175–180. 10.1016/j.jpsychires.2014.07.029 [DOI] [PubMed] [Google Scholar]
- Freeman D, Sheaves B, Waite F, Harvey AG, & Harrison PJ (2020). Sleep disturbance and psychiatric disorders. The Lancet Psychiatry, 7(7), 628–637. 10.1016/S2215-0366(20)30136-X [DOI] [PubMed] [Google Scholar]
- Gardner W, Murphy M, & Childs G (1999). The PSC-17: A brief pediatric symptom checklist with psychosocial problem subscales. A Report from PROS and ASPN, 5(3), 225–236. [Google Scholar]
- Garnett MF, Curtin SC, & Stone DM (2022). Suicide mortality in the United States, 2000–2020. NCHS Data Brief, no 433. National Center for Health Statistics. 10.15620/cdc:114217 [DOI] [PubMed] [Google Scholar]
- Gillett G, Watson G, Saunders KE, & McGowan NM (2021). Sleep and circadian rhythm actigraphy measures, mood instability and impulsivity: A systematic review. Journal of Psychiatric Research, 144, 66–79. 10.1016/j.jpsychires.2021.09.043 [DOI] [PubMed] [Google Scholar]
- Giromini L, Velotti P, de Campora G, Bonalume L, & Cesare Zavattini G (2012). Cultural adaptation of the difficulties in emotion regulation scale: Reliability and validity of an Italian version: Reliability and validity of the DERS in Italy. Journal of Clinical Psychology, 68(9), 989–1007. 10.1002/jclp.21876 [DOI] [PubMed] [Google Scholar]
- Goldstein TR, & Franzen PL (2020). Sleep difficulties and suicidality in youth: Current research and future directions. Current Opinion in Psychology, 34, 27–31. 10.1016/j.copsyc.2019.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Gross JJ (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Hanish AE, Lin-Dyken DC, & Han JC (2017). PROMIS sleep disturbance and sleep-related impairment in adolescents: Examining psychometrics using self-report and actigraphy. Nursing Research, 66(3), 246–251. 10.1097/NNR.0000000000000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris LM, Huang X, Linthicum KP, Bryen CP, & Ribeiro JD (2020). Sleep disturbances as risk factors for suicidal thoughts and behaviours: A meta-analysis of longitudinal studies. Scientific Reports, 10(1), 13888. 10.1038/s41598-020-70866-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatkevich C, Penner F, & Sharp C (2019). Difficulties in emotion regulation and suicide ideation and attempt in adolescent inpatients. Psychiatry Research, 271, 230–238. 10.1016/j.psychres.2018.11.038 [DOI] [PubMed] [Google Scholar]
- Hill RM, Hatkevich CE, Kazimi I, & Sharp C (2017). The Columbia-Suicide severity rating scale: Associations between interrupted, aborted, and actual suicide attempts among adolescent inpatients. Psychiatry Research, 255, 338–340. 10.1016/j.psychres.2017.06.014 [DOI] [PubMed] [Google Scholar]
- Kalmbach DA, Ahmedani BK, Gelaye B, Cheng P, & Drake CL (2021). Nocturnal cognitive hyperarousal, perinatal-focused rumination, and insomnia are associated with suicidal ideation in perinatal women with mild to moderate depression. Sleep Medicine, 81, 439–442. 10.1016/j.sleep.2021.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SG, Ali SK, Simpson B, Britt V, & McCall WV (2014). Associations between sleep disturbance and suicidal ideation in adolescents admitted to an inpatient psychiatric unit. International Journal of Adolescent Medicine and Health, 26(3), 411–416. 10.1515/ijamh-2013-0318 [DOI] [PubMed] [Google Scholar]
- Kearns JC, Coppersmith DDL, Santee AC, Insel C, Pigeon WR, & Glenn CR (2020). Sleep problems and suicide risk in youth: A systematic review, developmental framework, and implications for hospital treatment. General Hospital Psychiatry, 63, 141–151. 10.1016/j.genhosppsych.2018.09.011 [DOI] [PubMed] [Google Scholar]
- Kheirandish L, & Gozal D (2006). Neurocognitive dysfunction in children with sleep disorders. Developmental Science, 9(4), 388–399. 10.1111/j.1467-7687.2006.00504.x [DOI] [PubMed] [Google Scholar]
- Killgore WDS (2010). Effects of sleep deprivation on cognition. In Kerkhof GA and Dongen H. P. A. van (Eds.), Progress in Brain Research (Vol. 185, pp. 105–129). Elsevier. 10.1016/B978-0-444-53702-7.00007-5 [DOI] [PubMed] [Google Scholar]
- Kirschbaum-Lesch I, Holtmann M, & Legenbauer T (2021). Deficits in emotion regulation partly mediate the relation between sleep problems and depressive symptoms in adolescent inpatients with depression. Frontiers in Psychiatry, 12, 622833. 10.3389/fpsyt.2021.622833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, & May AM (2015). The three-step theory (3ST): A new theory of suicide rooted in the “Ideation-to-Action” framework. International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Lee YJ, Cho SJ, Cho IH, & Kim SJ (2012). Insufficient sleep and suicidality in adolescents. Sleep, 35(4), 455–460. 10.5665/sleep.1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis PA, Knoblich G, & Poe G (2018). How memory replay in sleep boosts creative problem-solving. Trends in Cognitive Sciences, 22(6), 491–503. 10.1016/j.tics.2018.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlewood DL, Kyle SD, Carter LA, Peters S, Pratt D, & Gooding P (2019). Short sleep duration and poor sleep quality predict next-day suicidal ideation: An ecological momentary assessment study. Psychological Medicine, 49(3), 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Steele SJ, Hamilton JL, Do QBP, Furbish K, Burke TA, Martinez AP, & Gerlus N (2020). Sleep and suicide: A systematic review and meta-analysis of longitudinal studies. Clinical Psychology Review, 81, 101895. 10.1016/j.cpr.2020.101895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato N, & Gradisar M (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Medicine Reviews, 18(6), 521–529. 10.1016/j.smrv.2014.03.006 [DOI] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, & Linehan MM (2007). Dialectical behavior therapy with suicidal adolescents. Guilford Press. [Google Scholar]
- Miragoli S, Milani L, Di Blasio P, & Camisasca E (2020). Difficulties in emotion regulation in child abuse potential: Gender differences in parents. Child Abuse & Neglect, 106, 104529. 10.1016/j.chiabu.2020.104529 [DOI] [PubMed] [Google Scholar]
- Neacsiu AD, Fang CM, Rodriguez M, & Rosenthal MZ (2018). Suicidal behavior and problems with emotion regulation. Suicide and Life-Threatening Behavior, 48(1), 52–74. 10.1111/sltb.12335 [DOI] [PubMed] [Google Scholar]
- Neumann A, van Lier PAC, Gratz KL, & Koot HM (2010). Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. Assessment, 17(1), 138–149. 10.1177/1073191109349579 [DOI] [PubMed] [Google Scholar]
- O’Leary K, Bylsma LM, & Rottenberg J (2017). Why might poor sleep quality lead to depression? A role for emotion regulation. Cognition and Emotion, 31(8), 1698–1706. 10.1080/02699931.2016.1247035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer CA, & Alfano CA (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep medicine reviews, 31, 6–16. 10.1016/j.smrv.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Parsons CE, Schofield B, Batziou SE, Ward C, & Young KS (2022). Sleep quality is associated with emotion experience and adaptive regulation of positive emotion: An experience sampling study. Journal of Sleep Research, 31(4), e13533. 10.1111/jsr.13533 [DOI] [PubMed] [Google Scholar]
- Perez J, Venta A, Garnaat S, & Sharp C (2012). The difficulties in emotion regulation scale: Factor structure and association with nonsuicidal self-injury in adolescent inpatients. Journal of Psychopathology and Behavioral Assessment, 34(3), 393–404. 10.1007/s10862-012-9292-7 [DOI] [Google Scholar]
- Pigeon WR, Pinquart M, & Conner K (2012). Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. The Journal of Clinical Psychiatry, 73(9), e1160–e1167. 10.4088/JCP.11r07586 [DOI] [PubMed] [Google Scholar]
- Rapee RM, Oar EL, Johnco CJ, Forbes MK, Fardouly J, Magson NR, & Richardson CE (2019). Adolescent development and risk for the onset of social-emotional disorders: A review and conceptual model. Behaviour Research and Therapy, 123, 103501. 10.1016/j.brat.2019.103501 [DOI] [PubMed] [Google Scholar]
- Reynolds WM, & Mazza JJ (1999). Assessment of suicidal ideation in inner-city children and young adolescents: Reliability and validity of the Suicidal Ideation Questionnaire-JR. School psychology review, 28(1), 17–30. 10.1080/02796015.1999.12085945 [DOI] [Google Scholar]
- Ribeiro JD, Bender TW, Buchman JM, Nock MK, Rudd MD, Bryan CJ, Lim IC, Baker MT, Knight C, Gutierrez PM, & Joiner TE (2015). An investigation of the interactive effects of the capability for suicide and acute agitation on suicidality in a military sample. Depression and Anxiety, 32(1), 25–31. 10.1002/da.22240 [DOI] [PubMed] [Google Scholar]
- Rogers ML, Ringer FB, & Joiner TE (2016). A meta-analytic review of the association between agitation and suicide attempts. Clinical Psychology Review, 48, 1–6. 10.1016/j.cpr.2016.06.002 [DOI] [PubMed] [Google Scholar]
- Sadeh A (2007). Consequences of sleep loss or sleep disruption in children. Sleep Medicine Clinics, 2(3), 513–520. 10.1016/j.jsmc.2007.05.012 [DOI] [Google Scholar]
- Schennach R, Feige B, Riemann D, Heuser J, & Voderholzer U (2019). Pre- to post-inpatient treatment of subjective sleep quality in 5,481 patients with mental disorders: A longitudinal analysis. Journal of Sleep Research, 28, e12842. 10.1111/jsr.12842 [DOI] [PubMed] [Google Scholar]
- Scott J, Kallestad H, Vedaa O, Sivertsen B, & Etain B (2021). Sleep disturbances and first onset of major mental disorders in adolescence and early adulthood: A systematic review and meta-analysis. Sleep Medicine Reviews, 57, 101429. 10.1016/j.smrv.2021.101429 [DOI] [PubMed] [Google Scholar]
- Shahid A, Khairandish A, Gladanac B, & Shapiro C (2012). Peeking into the minds of troubled adolescents: The utility of polysomnography sleep studies in an inpatient psychiatric unit. Journal of Affective Disorders, 139(1), 66–74. 10.1016/j.jad.2012.01.034 [DOI] [PubMed] [Google Scholar]
- Shepard CA, Rufino KA, Lee J, Tran T, Paddock K, Wu C, Oldham JM, Mathew SJ, & Patriquin MA (2023). Nighttime sleep quality and daytime sleepiness predicts suicide risk in adults admitted to an inpatient psychiatric hospital. Behavioral Sleep Medicine, 21, 129–141. 10.1080/15402002.2022.2050724 [DOI] [PubMed] [Google Scholar]
- Simon EB, Vallat R, Barnes CM, & Walker MP (2020). Sleep loss and the socio-emotional brain. Trends in Cognitive Sciences, 24(6), 435–450. 10.1016/j.tics.2020.02.003 [DOI] [PubMed] [Google Scholar]
- Tamm S, Nilsonne G, Schwarz J, Golkar A, Kecklund G, Petrovic P, Fischer H, Åkerstedt T, & Lekander M (2019). Sleep restriction caused impaired emotional regulation without detectable brain activation changes—A functional magnetic resonance imaging study. Royal Society Open Science, 6(3), 181704. 10.1098/rsos.181704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson EC, Fox KA, Lapomardo A, Hunt JI, & Wolff JC (2020). Youth self report thought problems and sleep difficulties are linked to suicidal ideation among psychiatrically hospitalized adolescents. Journal of Child and Adolescent Psychopharmacology, 30(8), 522–525. 10.1089/cap.2019.0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, & Imai K (2014). Mediation: R package for causal mediation analysis. Journal of Statistical Software, 59(5), 1–38. 10.18637/jss.v059.i0526917999 [DOI] [Google Scholar]
- van Buuren S, & Groothuis-Oudshoorn K (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ (2016). Mediation analysis: A practitioner’s guide. Annual Review of Public Health, 37, 17–32. [DOI] [PubMed] [Google Scholar]
- Wall K, Vanwoerden S, Penner F, Patriquin M, Alfano CA, & Sharp C (2022). Adolescent sleep disturbance, emotion regulation and borderline features in an inpatient setting. Journal of Clinical Child and Adolescent Psychology, 51, 892–906. 10.1080/15374416.2020.1772081 [DOI] [PubMed] [Google Scholar]
- Weis D, Rothenberg L, Moshe L, Brent DA, & Hamdan S (2015). The effect of sleep problems on suicidal risk among young adults in the presence of depressive symptoms and cognitive processes. Archives of Suicide Research, 19(3), 321–334. 10.1080/13811118.2014.986697 [DOI] [PubMed] [Google Scholar]
- Williams JMG, Duggan DS, Crane C, & Fennell MJV (2006). Mindfulness-based cognitive therapy for prevention of recurrence of suicidal behavior. Journal of Clinical Psychology, 62(2), 201–210. 10.1002/jclp.20223 [DOI] [PubMed] [Google Scholar]
- Wolff JC, Frazier EA, Weatherall SL, Thompson AD, Liu RT, & Hunt JI (2018). Piloting of COPES: An empirically informed psychosocial intervention on an adolescent psychiatric inpatient unit. Journal of Child and Adolescent Psychopharmacology, 28(6), 409–414. 10.1089/cap.2017.0135 [DOI] [PubMed] [Google Scholar]
- Wolff JC, Thompson E, Thomas SA, Nesi J, Bettis AH, Ransford B, Scopelliti K, Frazier EA, & Liu RT (2019). Emotion dysregulation and non-suicidal self-injury: A systematic review and meta-analysis. European Psychiatry, 59, 25–36. 10.1016/j.eurpsy.2019.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, Johnston KL, & Pilkonis PA (2012). Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behavioral Sleep Medicine, 10(1), 6–24. 10.1080/15402002.2012.636266 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


