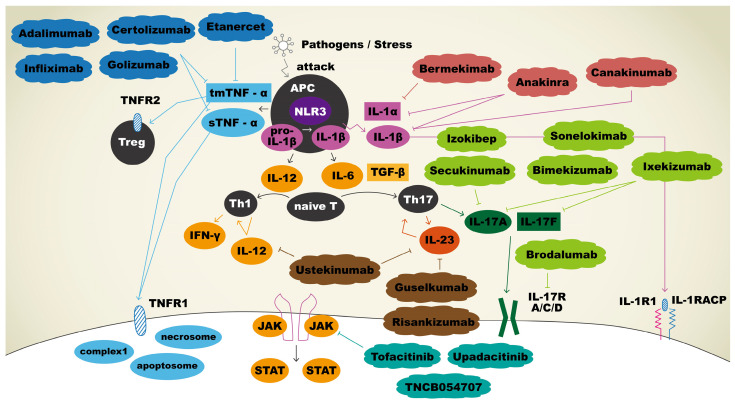
Figure 1.
Immunopathogenesis and therapeutic agents targeting immune mediators in hidradenitis suppurativa. Upon APCs sensing pathogens, tmTNF-α and sTNF-α were secreted, and both bound to TNFR1 to facilitate apoptosis, necroptosis, and inflammation reactions. tmTNF-α will also bind to TNFR2 to play a role in regulation of cell activation, migration, and proliferation. Adalimumab, certolizumab, golimumab, and infliximab bind and neutralize sTNF-α and tmTNF-α, thus inhibiting the inflammatory cascade. IL-1β is initially produced as a precursor and then cleaved by NLR3 to become a mature form. Mature IL-1β binds IL-1R1 with co-receptor IL-1RAcP to promote keratinocyte proliferation. Anakinra inhibits both IL-1α and IL-1β, whereas sonelokimab targets IL-1β, and bermekimab targets IL-1α specifically to use off-label for HS. APCs release IL-12 for the differentiation of naïve T cells into Th1 and IL-6 for the differentiation of naïve T cells into Th17 cells. Th17 cells produce IL-23, which promotes the production of IL-17. IL-17 binds to its receptor, contributing to the proliferation of keratinocytes. Sekukinumab, bimekizumab, izokibep, sonelokimab, ixekizumab, and brodalumab are biologic agents that block IL-17 pathway and thus have been explored as off-label treatments for HS. Ustekinumab is an antagonist that blocks both IL-12 and IL-23 to result in the downregulation of immune system. Guselkumab and risankizumab bind selectively to IL-23 only. Three biologics act as JAK inhibitors: tofacitinib, upadacitinib, and TNCB054707.