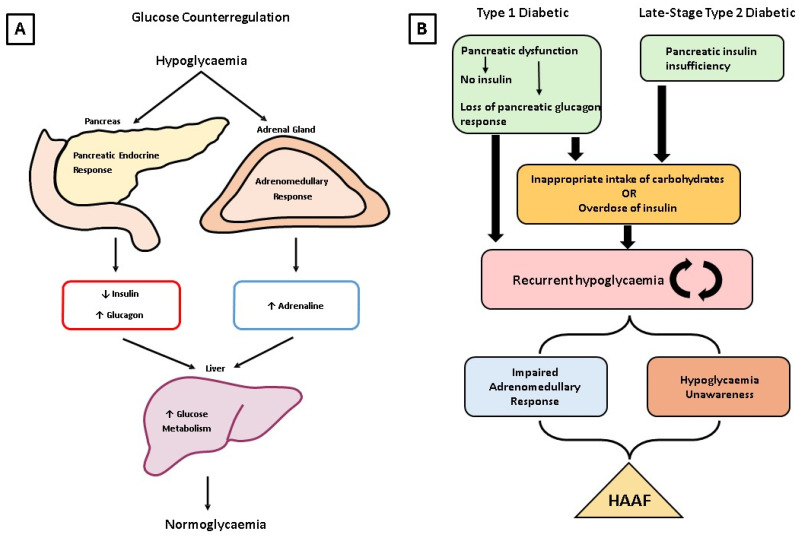
Figure 1.
(A) The glucose counterregulatory response to hypoglycaemia in non-diabetic individuals. Following hypoglycaemia stimuli, the pancreatic endocrine response leads to reduced insulin and elevated glucagon, while the adrenal medulla releases adrenaline into the circulation. These molecules have a profound impact on glucose metabolism in the liver, which brings blood glucose levels back up to normal. (B) The progression of HAAF in a type 1 or type 2 diabetic patient. A type 1 diabetic will use exogenous insulin administration to treat the loss of pancreatic beta cells, while some type 2 diabetics may require exogenous insulin due to the progression of the disease. However, overdose of insulin can lead to hypoglycaemia. Concurrently, loss of pancreatic beta cells leads to alpha cell dysfunction and subsequent loss of the pancreatic glucagon response to hypoglycaemia in type 1 diabetics. In type 2 diabetics, insulin resistance results in a compensatory response by the pancreas to produce more insulin, leading to hypoglycaemia. Delayed postprandial insulin secretion can also occur in type 2 diabetics, increasing hypoglycaemic risk. In the longer term, type 2 diabetics rely on the administration of exogenous insulin due to the development of absolute insulin deficiency, placing them at risk of hypoglycaemic episodes with inappropriate overdoses of exogenous insulin. In both types of diabetes, this culminates in the onset of recurrent hypoglycaemia, which further impairs the adrenomedullary response and neurogenic symptoms response. This leads to hypoglycaemia-associated autonomic failure (HAAF), where more frequent and severe hypoglycaemic episodes can cause seizures, coma, and death.