Fig. 1 |. Antibiotic targets and antibiotic resistance strategies deployed by uropathogenic Escherichia coli.
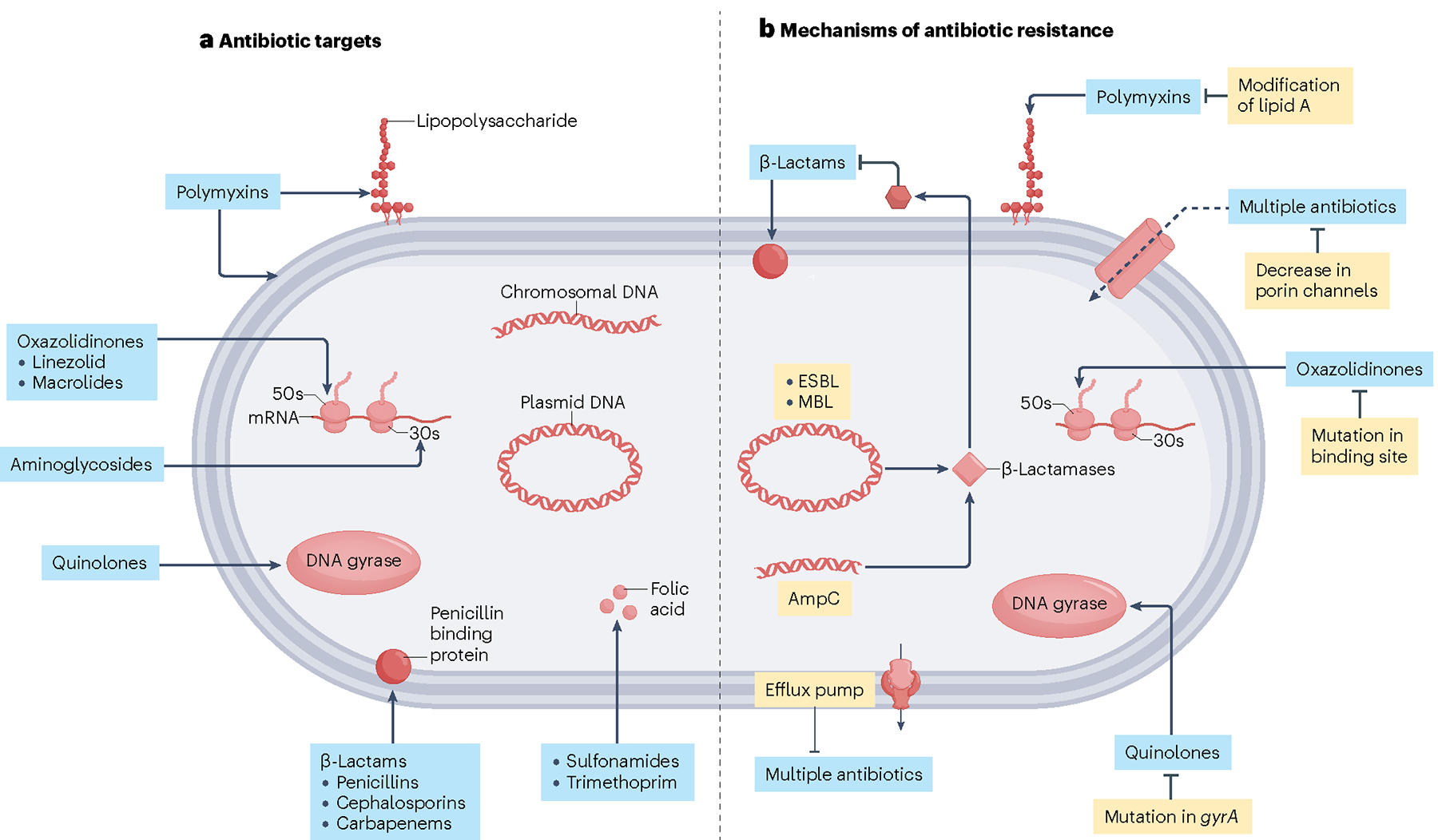
a, Targets of antibiotics used to treat uropathogenic Escherichia coli and Gram-negative uropathogens. Polymyxin antibiotics target outer membrane phospholipids and lipopolysaccharides of Gram-negative bacterial cell membranes. Oxazolidinones inhibit bacterial protein synthesis by blocking the large ribosomal subunit. Similarly, aminoglycosides inhibit bacterial protein synthesis by blocking the small ribosomal subunit. Quinolones target enzymes involved in bacterial DNA synthesis. β-lactam antibiotics prevent bacterial cell wall synthesis. Sulphonamides prevent folic acid synthesis in bacteria by targeting dihydropteroate synthase. b, Antibiotic resistance strategies adapted by uropathogenic E. coli and Gram-negative uropathogens. Bacteria can resist β-lactam antibiotics through the expression of β-lactamases, which disrupt the structure of the antibiotic and render it ineffective. They can also increase the expression of efflux pumps, which facilitate the removal of antibiotics from the bacterial cell interior. Conversely, bacteria can suppress expression of porin channels, reducing access to the bacterial cell interior to antibiotics. Bacteria can adapt to the selective pressure of antibiotics by modifying lipid A so that polymyxins no longer recognize their substrate. They can mutate their DNA or protein synthesis machinery so that oxazolidinones and quinolones can no longer bind their targets, respectively. ESBL, extended-spectrum β-lactamase; MBL, metallo-β-lactamase. Figure adapted from ref. 17, Springer Nature Ltd.
