Figure 12:
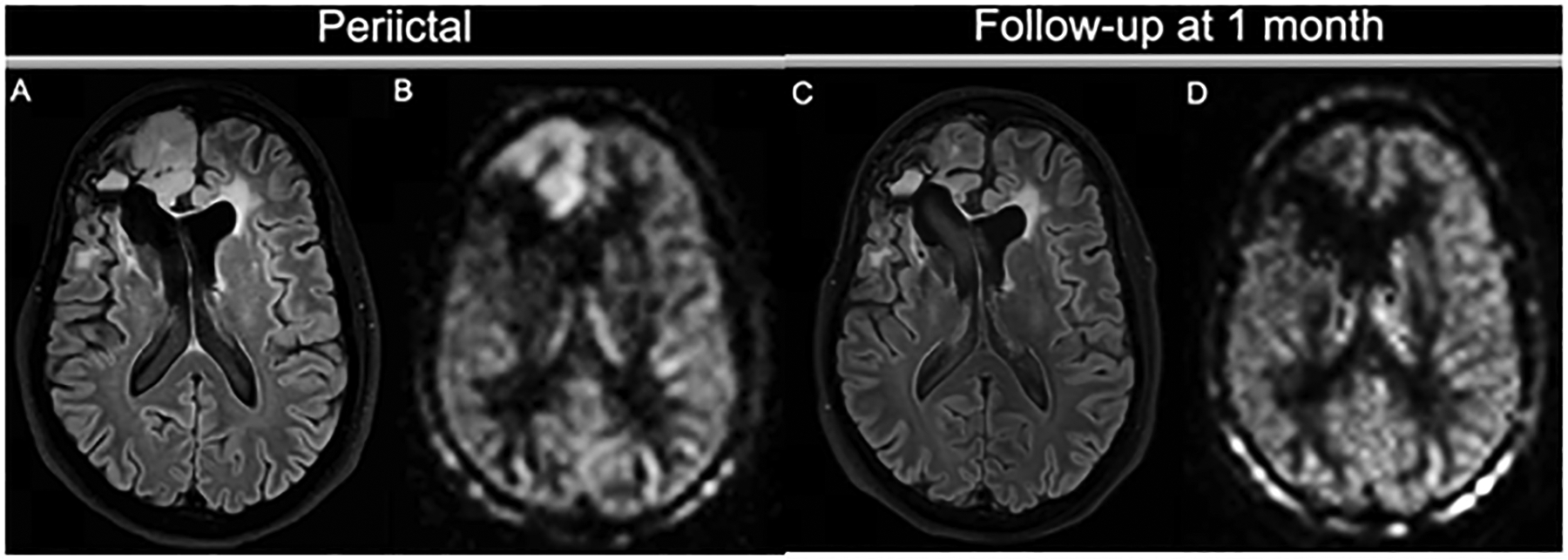
Seizure activity on ASL. A patient with a history of frontal ganglioneuroma resection 20 years before this presentation had an epileptic seizure, presumably due to encephalomalacia/gliosis. On the peri-ictal MRI, the FLAIR image (A) shows a swollen cortical ribbon in the right medial frontal lobe, with a corresponding increased perfusion signal on 3D ASL (B). Both the FLAIR abnormality and the hyperperfusion are limited to the cortex. Note the contrast between the perfusion signal in the cortex and the subcortical white matter. Lateral to this finding is the stable-appearing surgical cavity with fluid-fluid level and ex vacuo dilation of the right lateral ventricle. At follow-up, the cortical abnormality has almost completely resolved: the cortex is normal size and only minimal FLAIR hyperintensity is visible (C). The ASL scan (D) shows normalized perfusion in the affected region, similar to the left frontal lobe.
