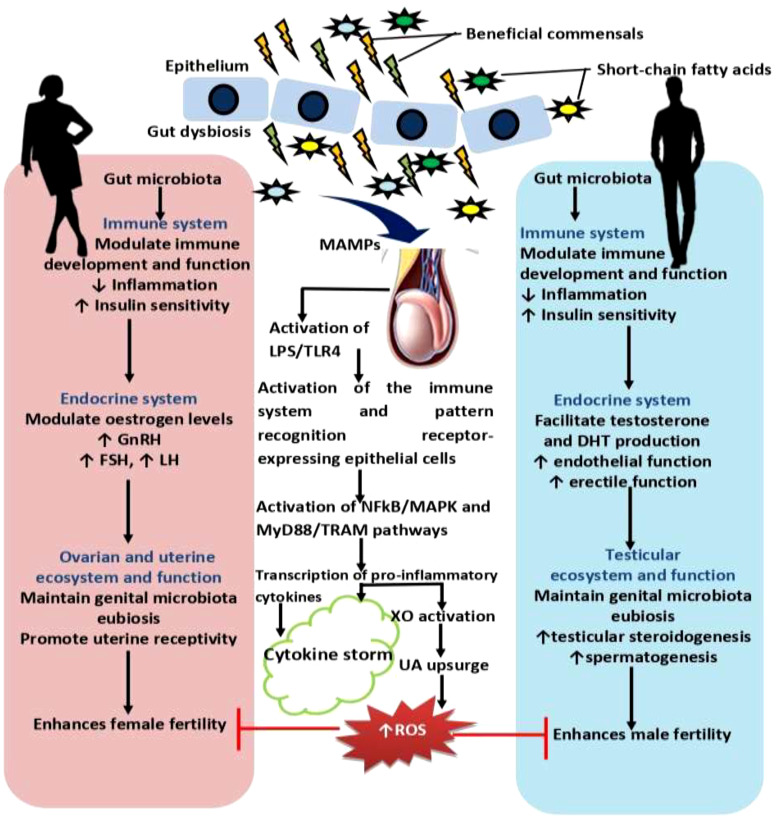
Figure 2.
Effect of gut microbiota and dysbiosis on male and female reproductive function. Gut microbiota promotes innate and adaptive immune development and function, and control inflammatory response, which in turn enhances insulin sensitivity. Improved insulin sensitivity and the maintenance of balance redox state facilitates the hypothalamic-pituitary-gonadal axis, culminating in optimal levels of gonadotropin releasing hormone, GnRH, follicle-stimulating hormone, FSH, and lutenising hormone, LH that results in optimal ovarian steroidogenesis (with optimal oestrogen production), testicular steroidogenesis (with optimal testosterone and dihydrotestosterone, DHT, production), and spermatogenesis. These events promote reproductive functions. However, gut dysbiosis promotes the translocation of microbial-associated molecular patterns, MAMPs, such as lipoprotein acids, lipoproteins, peptidoglycans, and lipopolysaccharide, LPS from the gut through the circulation via the hepatic portal vein or lymphatic system into the gonads to induce hyper-immunological response, chronic inflammation, and gonadal damage by activating the innate immune cells and pattern recognition receptors-expressing epithelial cells through LPS/toll like receptor 4 (TLR4), nuclear factor kappa-B (NFkB)/mitogen-activated protein kinases (MAPK), and MyD88 and TRAM-dependent signaling pathways. Activation of these pro-inflammatory processes stimulate xanthine oxidase, leading to increased uric acid generation and oxidative stress that causes ovarian and testicular injury and impairs fertility.