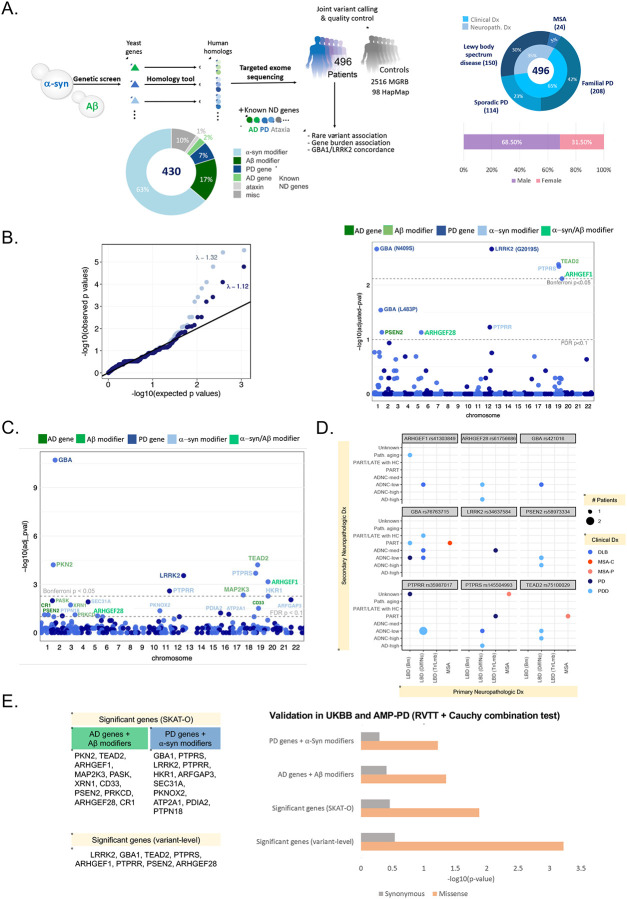
Figure 1. High-depth (~100X) patient exome screening identifies shared genetic risk among synucleinopathies, and an overlap with known PD and AD genes.
(A) Study design (sequencing and analysis workflow), breakdown of target genes, and primary diagnosis and demographics of the sequenced synucleinopathy cases.
(B) Quantile-quantile plot of observed versus expected p-values from the variant-level Fisher’s Exact test for association between cases and MGRB controls and their respective genomic inflation with and without ClinVar variants (left). Manhattan plot of FDR-adjusted (permutation-based case-control resampling) p-values resulting from the variant-level association (right). Dashed lines indicate Bonferroni and FDR significance thresholds. Amino acid changes are noted in parentheses for known ClinVar pathogenic variants. Eight missense variants and one splice region variant were significant at FDR adjusted p-value < 0.1.
(C) Manhattan plot showing FDR-adjusted p-values from the gene-level rare variant association test (cases vs. MGRB controls) using SKAT-O. Dashed lines indicate Bonferroni and FDR significance thresholds. At FDR adjusted p-value < 0.1, 22 significant genes were identified to have increases rare nonsynonymous variant burden in cases.
(D) Top variant-level hits are shared across clinical synucleinopathy diagnoses in pathologically confirmed cases. Each dot is colored by the clinical diagnosis. Size of each dot indicates the number of patients with a particular diagnosis. Primary neuropathological diagnoses are shown on the x-axis and secondary neuropathological diagnoses are shown on the y-axis. See Supplemental Figure 1 for the expanded list. Here, ADNC: Alzheimer disease neuropathologic change; LATE: limbic predominant age-related TDP-43 encephalopathy; MCI: mild cognitive impairment; MSA-C: multiple system atrophy cerebellar type; MSA-P: multiple system atrophy parkinsonian type; PART: primary age-related tauopathy (tau deposits found without beta-amyloid); PDD: Parkinson’s disease with dementia, LBD (Brn): LBD (Brainstem), LBD (Diff/Nc): LBD (Diffused/Neocortical), and LBD (Tr/Lmb): LBD (Translational/Limbic), Path. aging: pathologic aging with beta-amyloid deposits but no tau.
(E) Validation of variant- and gene-level rare variant burden in Parkinson’s disease (PD) in the UK Biobank (UKBB) and AMP-PD datasets using the rare variant trend test (RVTT). We tested variant-level significant-genes, SKAT-O significant genes, as well as two subsets of significant genes: (i) AD genes and Aβ modifiers, and (ii) PD genes and α-syn modifiers. We observed a significant increasing trend in rare missense variant occurrences in PD cases compared to control in both cohorts. There was no enrichment of synonymous variants. Cauchy combination test was performed to combine the RVTT p-values from individual datasets. Combined p-values on a negative log10 scale are shown in the bar chart.