Abstract
Introduction and importance
Uterine torsion are extremely rare in pregnancy as few cases have been reported. Torsion of the pregnant uterus is defined as the rotation more than 45 degrees around the long axis of the uterus. It has been referred as, once-in-a-lifetime diagnosis by obstetricians and gynecologists. This paper reports a case of uterine torsion and velamentous cord insertion from our obstetrical practice, along with a review of reported cases.
Case presentation
The 30-year-old patient (G2P1) at 38 weeks' gestation with a singleton pregnancy, was admitted to the Obstetrical Unit with uterine cramping and decreased fetal movement. Her prior obstetrical history included one uncomplicated term Cesarean section (2016), the current pregnancy had been velamentous cord insertion at 20 weeks' gestation and intra-uterine growth restriction at the 33rd -week gestation until the presentation date. Emergency Cesarean section was performed the 90 degrees uterine torsion and was diagnosed intra-operatively. This patient and her baby recovered and were discharged home on the fifth post-operative day.
Clinical discussion
Uterine torsion, a rare pregnancy complication, should be considered when evaluating acute abdominal pain or performing a Cesarean delivery, especially in cases of abnormal fetal presentation, pelvic adhesions, uterine fibroids, malformations, or ovarian tumors. Early diagnosis and proper treatment are crucial due to the negative prognosis for both mother and baby.
Conclusion
Uterine torsion along with velamentous cord insertion is difficult to diagnosis due to its rarity. It is essential to focus on uterine malformations during ultrasound examinations in the first, second, and third trimesters.
Keywords: Uterine torsion, Pregnancy, Velamentous cord insertion, Obstetric complications
Highlights
-
•
Uterine torsion and velamentous cord insertion are rare obstetric complications.
-
•
Severe acute uterine torsion can result in placental abruption, intrauterine fetal death and maternal death. In addition, velamentous cord insertion is associated with increased risks of preterm delivery.
-
•
The routine obstetric ultrasound is important in systematic assessment of the uterine malformations and placental cord insertion site.
-
•
Early detection and appropriate peripartum management will highly reduce complications during labor.
-
•
Delivery was achieved via classical cesarean section.
1. Introduction and importance
The uterus usually rotates along the longitudinal axis of the uterus by less than 45 degrees in approximately two-third of the cases in the last month of pregnancy [1]. Uterine torsion is defined as the phenomenon when the uterus twists more than 45 degrees along the longitudinal axis of the uterus. It occurs at the junction of the cervix and uterine corpus. When the uterus is twisted, the blood supply from the veins is impeded first, followed by the arteries. This causes symptoms listed as abdominal pain, fetal distress and placental abruption [1]. Most clinical cases of uterine torsion are associated with uterine fibroids, ovarian cysts, abnormal uterine growth, adnexal tumors and trauma. Nevertheless, in 30 % of the cases, the cause cannot be found [3].
Up to our knowledge, the first human case was detected in postmortem examinations and was reported by Virchow [2]. However, it was in 1876 when Labbe actually published the first case of uterine torsion in a human and the first maternal death was recorded in 1960 [4]. Although uterine torsion is not common, with most of the literature comprising single case reports, it is a dangerous complication that can cause serious consequences. Approximately 250+ cases of uterine torsion are reported worldwide. The fact that maternal and perinatal mortality rates depend on gestational age and torsion severity [3].
The pre-operative diagnosis is absolutely challenging, most of which will be diagnosed intra-operatively. Some cases can be diagnosed with MRI.
At the hospital where we conducted our study, we encountered a case of intrauterine torsion with velamentous cord insertion at 90 degrees in a 38-week slow-growth fetus. The condition was successfully treated with emergency surgery, and both the mother and her baby responded well. They were discharged after a 5-day treatment period. In our case, the presentation was gradual compared with the acute presentations that have been reported, which may mislead clinicians towards more benign diagnoses. Our case report aims to add to the literature on uterine torsion, providing a unique presentation, clinical features, and treatment.
2. Case presentation
In terms of clinical case, this is a 30-year-old pregnant woman with gravid 2, para 1. The patient's medical history is a normal medical and surgical history. In terms of personal obstetric history, the patient underwent a Cesarean section in 2016 for an unknown reason.
Further information regarding antenatal care is as follows: during antenatal care, velamentous cord insertion was detected at the 20th week of gestation and fetal growth restriction was noted at the 33rd week of gestation by ultrasound scan. Her result of GBS test (group B Streptoccocus) was negative. The patient was admitted because of abdominal pain, decreased fetal movement, and a history of Cesarean section scar at the 38th week of gestation.
Regarding initial admission examination at the hospital, the woman was conscious with a pink complexion and abdominal pain. Her heart rate was 90 beats/min, blood pressure was 120/80 mmHg. The uterine's height was 29 cm. The fetal heart rate was 150 beats per minute. Upon vaginal examination, cervix dilated 2 cm with 60 % effacement and positioned high with a posterior cervical lip.
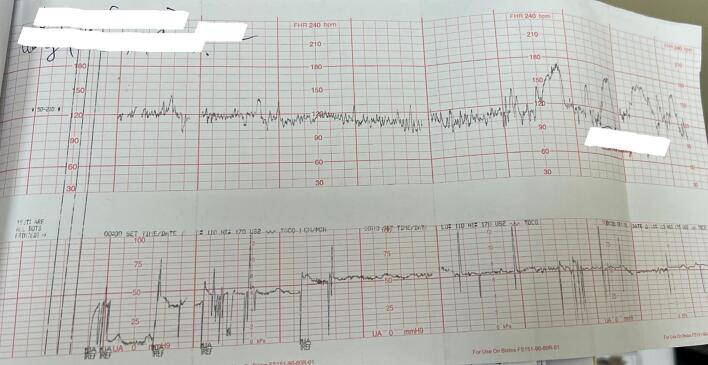
Additional information regarding sub-clinical procedures is to be presented as follows. In terms of ultrasound, 01 fetus with cephalic presentation. The fetal heart rate was 153 beats per min. On ultrasound, specific measurements are as follows: Biparietal diameter: 89 mm; Fermul length: 67 mm; Abdominal circumference: 325 mm. Ultrasound scan at 38 weeks of gestation showed estimated fetal weight <10th percentile (2667 g) and velamentous cord insertion. The anterior placenta was classified as Grade I, with no evidence of retroplacental hemorrhage. No free fluid was found in the abdominal cavity. The patient was hemodynamically stable during admission. Routine laboratory tests were within in normal limit. During routine management, the fetal heart rate monitoring (FHRm) on CTG was normal (Fig. 1).
Fig. 1.
Image of CTG at admision.
In terms of preoperative examination, it was within the accepted normal limits.
Further details concerning the general progress are to be presented as follows: The patient underwent the surgery at 08 am 05 on June 17, 2022. The pre-operative diagnosis was as follows: 2nd pregnancy, 38-week gestation, head down, transverse lie, intra-uterine growth restriction, velamentous cord insertion/scars of the previous Cesarean section.
The surgical report is as follows: Spinal anesthesia was administered, and surgery was performed through the previous Cesarean section scar. There was no bleeding in the abdominal cavity. On the other hand, the uterus was twisted to the right at a 90 degrees angle, with an enlarged blood vessel without adhering to the surrounding organs. The ovary, the Fallopian tube and the round ligament (T) were visible in front of the incision (Fig. 2). Diagnosis conlcluded this was one case of uterine torsion.
Fig. 2.
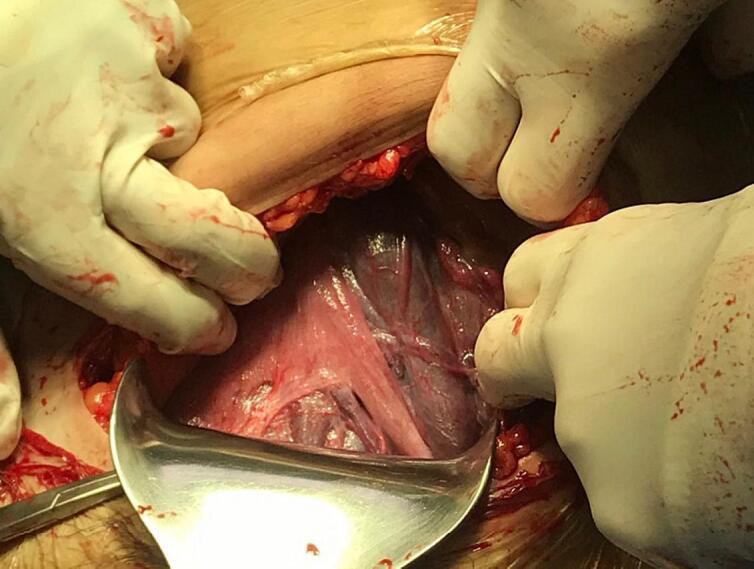
The uterus twisted to the right at 90 degrees, showing the Fallopian tube and the round ligament in front of the incision site, with many enlarged blood vessels.
What is more, untwisting was difficult. After incision of lower segmental uterus, the amniotic fluid was cloudy and with the performance of amniotomy (AROM). A well-being male baby weighing 2300 g was delivered with APGAR (Appearance, Pulse, Grimace, Activity and Respiration) scores of 8 and 9 at the first and fifth minutes (Fig. 4).
Fig. 4.

Baby condition: weight 2300 g Apgar scores 8/9.
After delivery, the velamentous cord insertion was observed (Fig. 3). The uterus was repositioned and normal in size and color. The bilateral ureters were normal. The estimated blood loss was approximately 200 ml.
Fig. 3.

The post-partum image of velamentous cord insertion (the cord is attached to the membrane disc, 2-3 cm away from the edge of the disc).
After surgery, the mother's condition was stable, with the following measurements: a blood pressure of 120/70 mmHg and clear urine output via a catheter.
The post-operative diagnosis is follows: Uterine torsion at the 38th-week pregnancy with intrauterine growth restriction, velamentous cord insertion and the previous cesarean section scar. Because of the patient's normal post-operative recovery, she was discharged after 5-day treatment. The patient was scheduled 1 month later for follow-up routinely and their health conditions were still stable.
Method: This case report adheres to the SCARE criteria [5].
3. Discussion
Uterine torsion is a rare complication during pregnancy. Uterine torsion is defined as the uterus twisting more than 45 degrees along the longitudinal axis, usually approximately 180 degrees, and more than 180 degrees is unlikely to occur. However, few cases of torsion of a maximum of 720 degrees have also been reported in the literature [1]. In this case in this paper, it is 90 degrees. Uterine torsion is an unexpected condition with high perinatal mortality 12–13 % and occasional maternal mortality [6]. Maternal complications include complete or partial placental abruption and maternal hemodynamic shock [1]. There have been no maternal deaths reported before 20 weeks, mortality rates of 17 % reported between 20 and 28 weeks, 10 % at 29 to 34 weeks, and 9 % at term gestation [7]. Fetal complications associated with uterine torsion are fetal hypoxia, fetal antepartum hemorrhage, and death [6].
3.1. In terms of etiology and pathogenetic mechanisms
Uterine torsion occurs independently of the patient's age, the number of pregnancies, and fetal age [6]. The exact mechanism for uterine torsion is still unclear. Approximately 30 % of uterine torsion cases during pregnancy take place because of an unknown cause. Most cases are associated with risk factors listed as uterine fibroids, ovarian cysts, uterine malformations, pelvic adhesions, abnormal fetal position (especially transverse lie), history of Cesarean section or abdominal trauma [6]. The study by Kawagami that evaluated the uterine scar healing in the lower uterine segment of Cesarean section patients using MRI indicated the poor uterine scar healing. This poor healing can lead to poor recovery and result in elongated cervical length with weakened structure and angulation in the waist area, leading to torsion [21]. Robinson and Duvall suggest that some sudden movements of the patient during pregnancy may cause uterine torsion with abnormal structural and pathological changes in the pelvic area, approximately two-thirds, 66 % [8]. As in our case, an important risk factor was identified history of previous Cesarean section.
3.2. Diagnosis
The accurate diagnosis before treatment is impossible due to the inadequacy of the specific symptoms. Uterine torsion during pregnancy comprises the following symptoms listed as abdominal pain (95 %), shock, functional bowel obstruction, urinary symptoms, bleeding and prolonged labor. However, 11 % of cases are asymptomatic [6]. During labor, uterine torsion causes strong contractions; in contrast, the cervix is not dilated, resulting in fetal distress, increased uterine muscle tension, vaginal hemorrhage, and torsion of the vaginal tubes. Some signs described by Jensen during physical examination include palpating the round ligament through the abdominal wall, feeling the uterine artery pulsating during vaginal examination, vaginal torsion, cervical torsion, and rectal torsion [6].
Differential diagnoses consist of ectopic pregnancy, hemoperitoneum (intra-abdominal hemorrhage), pelvic tumor torsion, peritonitis, prolonged labor, placental abruption, intense uterine contractions, degenerative uterine fibroids, acute polyhydramnios [10,11,12].
Some ultrasound images suggest a diagnosis listed as a change in placental position or uterine fibroids compared to those of the initial ultrasound, the ovarian vasculature anterior to the lower body of the uterus. In addition, there may be signs of intrauterine gas on CT scan [13]. MRI can be diagnosed: the first clinical case diagnosed by MRI was conducted by Nichosol in 1995 with an X-sign of the vagina. Normally vagina appears H shaped [9].
Most cases can only be diagnosed only during the delivery. Most of the cases were mis-diagnosed with abnormal fetal heart rate [1,12] and placental abruption [13,18]. The patient in this case was admitted to the hospital with symptoms of abdominal pain, decreased fetal movements in one fetus with slow growth inside the uterus, accompanied by the velamentous cord insertion and the required emergency surgery. This patient who was recorded a history of one previous Cesarean section had a risk factor for uterine torsion. Moreover, the clinical symptoms at the rescue time were consistent with the increasing abdominal pain. When the abdomen was opened, a tense uterus, a 90 degrees uterine torsion, was observed. Upon examination, the umbilical cord attached to the membrane, divided into three blood vessels connected to the placenta, was revealed.
Velamentous cord insertion was detected at the mother's 20th week of gestation. Velamentous cord insertion is relatively rare, approximately 1 % and 7 % in singleton pregnancies and twin pregnancies, respectively [14]. The determination of the attachment site of the umbilical cord should be paid more attention in the second and third trimester as the ultrasound can exclude the possibility of a placental precursor vessel by transvaginal ultrasound, especially in high-risk cases listed as velamentous cord insertion, low-lying placenta, marginal placenta, small fetus, and twin pregnancy. Velamentous cord insertion has the potential to result in poor pregnancy outcomes, listed as preterm birth, small fetus, fetal distress, emergency cesarean section, and high perinatal mortality [15,16]. The study by Boulis revealed that the incidence of small fetus was 31 %, that of preterm birth as 29.5 %, and that of the emergency cesarean section as 69.49 % in the group with abnormal cord attachment (12). Additionally, velamentous cord insertion has a risk of bleeding in the third labor stage; therefore, it is necessary to actively remove the placenta by hand [17].
On the other hand, the rates of intrauterine fetal death and perinatal mortality in both the group with abnormal cord attachment and the group with normal cord attachment, compared to those of the general population, demonstrated differences among the studies. According to a large study comprising 9500 cases of abnormal cord attachment and over 600,000 pregnancies with normal cord attachment, a disparity in the mortality rate was identified: 1.6 % compared to 0.7 % [16]. However, a study by Raisanen [17], based on samples of 26,894 pregnant women and 633 cases with abnormal cord attachment, concluded that there was no significant difference in the frequency of mortality between the two groups: 0.5 % compared to 0.3 %.
3.3. Treatment
Emergency surgery is necessary when the patient exhibits acute symptoms or suspected uterine torsion. The approach for treating uterine torsion is mostly performed as follows: detorsion, uterine incision and addressing the underlying cause. Detorsion, as the best option for both the mother and the fetus, should be performed first if possible. If detorsion is impossible, uterine decision is performed with a transverse incision on the posterior surface of the uterus with a short and circular suture [18].
The incision on the uterus can be a transverse or vertical incision, usually on the posterior surface of the uterus due to uterine torsion [18]. In theory, the risk of uterine rupture with a transverse incision would be lower than with that with a vertical incision although the exact risk has not been indicated yet. The anatomical landmarks need to be identified before cutting into the uterine muscle so as to prevent damage towards the blood vessels or other organs [18,19].
Hysterectomy may be indicated when the uterus cannot be preserved (due to uterine necrosis or thrombosis of blood vessels caused by prolonged torsion), or in the case that the mother has completed her childbearing [20].
Other related factors listed as pelvic adhesions, uterine fibroids, or ovarian cysts should be addressed to prevent recurrence during the postpartum period.
Some preventive measures during the postpartum period can be implemented as follows: shortening the round ligaments of the uterus on both sides towards the front, reducing adhesion of the uterus on the posterior surface, reducing painful intercourse, or shortening the uterine ligaments on both sides [19,20].
4. Conclusions
Uterine torsion is a rare complication in pregnancy that is termed a “once-in-a-lifetime” diagnosis for obstetricians and gynecologists. Consequently, obstetricians should consider it upon evaluating a pregnant woman with acute abdominal pain or performing a Cesarean delivery in a pregnant woman having an abnormal fetal presentation, pelvic adhesions, uterine fibroids, uterine malformations or ovarian tumors. Early diagnosis and appropriate treatment are crucial as uterine torsion has a negative prognosis for both the mother and the baby. The anatomical landmarks should be identified before incising the uterine muscle with the purpose of preventing injury to the uterine blood vessels and assessing the torsion degree of the pregnant uterus.
What is more, the isue related to abnormal cord insertion needs attention because of the association with adverse pregnancy outcomes, especially the risk of anterior placental circulation.
It is essential to pay attention to uterine malformations in ultrasound in the first, second and third trimesters in order to determine the location of cord insertion, the lower uterine vascular system as well as to exclude the possibility of anterior placental circulation by transvaginal ultrasound in high-risk cases, listed as velamentous cord insertion, low-lying placenta, marginal insertion, small fetus, or twin pregnancy so as to avoid misdiagnosis. Concurrently, it is imperative any women should undergo gynecological examinations prior to conception with the purposse of identifying any potential underlying abnormalities.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
This report was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for Experiments in Humans.
This case report got ethical approval from our institution. The patient was given consent form before the surgery
Funding
Not applicable.
Author contribution
Thao Thi Kim Bui, Oanh Thi Kieu Nguyen, Huyen Thi Bich Tran, Tien Dong Phuong Nguyen, and Tung Viet Le were all equally contributing to the pre-, intra- and postoperative treatment of the patient. The first draft of the manuscript was written by Thao Thi Kim Bui and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Guarantor
Oanh Thi Kieu Nguyen MD, MSc.
Research registration number
None.
Conflict of interest statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We highly appreciate the support from the University Medical Center Ho Chi Minh City - Branch 2.
Contributor Information
Thao Thi Kim Bui, Email: thao.btk@umc.edu.vn.
Tung Viet Le, Email: tung.lv@umc.edu.vn.
Oanh Thi Kieu Nguyen, Email: oanhkieung@ump.edu.vn.
Huyen Thi Bich Tran, Email: huyen.ttb@umc.edu.vn.
Tien Dong Phuong Nguyen, Email: ndptien@ump.edu.vn.
References
- 1.Darido J., Grevoul Fesquet J., Diari J., El Haddad C., Bouzid N., et al. Hemorrhagic shock due to irreducible uterine torsion in a third trimester twin pregnancy: a case report. Clin. J. Obstet. Gynecol. 2020;3:085–089. [Google Scholar]
- 2.Piot D., Gluck M., Oxorn H. Torsion of the gravid uterus. Can. Med. Assoc. J. 1973;109 [PMC free article] [PubMed] [Google Scholar]
- 3.Liang R., Gandhi J., Rahmani B., Khan S.A. Uterine torsion: a review with critical considerations for the obstetrician and gynecologist. Transl. Res. Anat. 2020;21 [Google Scholar]
- 4.Kim S.K., Chung J.E., Bai S.W., Kim J.Y., Kwon H.K., Park K.H., Song C.H. Torsion of the pregnant uterus. Yonsei Med. J. 2001;42(2):267–269. doi: 10.3349/ymj.2001.42.2.267. [DOI] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cook K.E., Jenkins S.M. Pathologicaluterine torsion associated with placental abruption, maternal shock and intrauterine fetal demise. Am. J. Obstet. Gynecol. 2005;192:2082–2083. doi: 10.1016/j.ajog.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Yin F.L., Huang H.X., Zhang M., et al. Clinical analysis of uterine torsion and fibroids in full-term pregnancy: a case report and review of the literature. J. Int. Med. Res. 2020;48(6) doi: 10.1177/0300060520920404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson A.L., Duvall H.M. Torsion of the pregnant uterus. J. Obstet. Gynaec. Br. Commonw. 1931;38:55–84. [Google Scholar]
- 9.Nicholson W.K., Coulson C.C., McCoy C.M., Semelka R.C. Pelvic magnetic resonance imaging in the evaluation of uterine torsion. Obstet. Gynecol. 1995;85:888–890. doi: 10.1016/0029-7844(94)00283-j. [DOI] [PubMed] [Google Scholar]
- 10.Zeng G., Guo F., Gao Q., Liu C., Yang Z., Zhu Y. Acute gravid uterus torsion: a rare and dangerous obstetric emergency. Int. J. Gynaecol. Obstet. 2019;147(3):414–415. doi: 10.1002/ijgo.12954. [DOI] [PubMed] [Google Scholar]
- 11.Farhadifar Fariba, Nikkhoo Baharm, et al. Asymptomatic uterine torsion in pregnant woman. Indian J. Surg. 2014;76(4):321–322. doi: 10.1007/s12262-013-0981-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kimberly H, Adersen H. Uterine torsion in a full-term pregnancy presenting as prolonged latent phase and fetal intolerance of labor: a case report. Case Rep. Women's Health; 32 doi: 10.1016/j.crwh.2021.e00353. [DOI] [PMC free article] [PubMed]
- 13.Mokhtar Huda, Faridz Sumayyah, Ismail Rohana, Yaacob Nasuha, Ramli Roziana. Uterine torsion in pregnancy, expect the unexpected: case report. Int. J. Reprod. Contracept. Obstet. Gynecol. 2020;9:3473. doi: 10.18203/2320-1770.ijrcog20203343. [DOI] [Google Scholar]
- 14.Cathrine Ebbing Synnove L., Albrechtsen Johnsen Susanne, Ingvild D., Rasmussen S.C.V.S. Velamentous or marginal cordin sertion and the risk of spontaneous preterm birth, prelabor rupture of the membranes, and anomal ouscord length, a population-basedstudy. AOGS. 2016;96(1):78–85. doi: 10.1111/aogs.13035. [DOI] [PubMed] [Google Scholar]
- 15.Brouillet S., Dufour A., Prot F., Feige J.-J., Equy V., Alfaidy N., et al. Influence of the umbilical cord insertion site on the optimal individual birth weight achievement. Bio Med. Res. Int. 2014:2014. doi: 10.1155/2014/341251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebbing C.T.K., L JS, SA, SR. Third stage of labor risks in velamentous and marginal cord insertion: a population-based study. Acta Obstet. Gynecol. Scand. 2015;94(8):878–883. doi: 10.1111/aogs.12666. [DOI] [PubMed] [Google Scholar]
- 17.Raisanen S., Georgiadis L., Harju M., Keski-Nisula L., Heinonen S. Risk factors and adverse pregnancy outcomes among births affected by velamentous umbilical cord insertion: a retrospective population-based register study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012;16 doi: 10.1016/j.ejogrb.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 18.Agar N., Canis M., Accoceberry M., Bourdel N., Lafaye A.L., Gallot D. Torsion utérine avant travail avec décollement placentaire et mort foetale [Prelabour uterine torsion complicated by partial abruption and fetal death] Gynecol. Obstet. Fertil. 2014;42(6):451–453. doi: 10.1016/j.gyobfe.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Albayrak M., Benian A., Ozdemir I., Demiraran Y., Guralp O. Deliberate posterior low transverse incision at cesarean section of a gravid uterus in 180 degrees of torsion: a case report. J. Reprod. Med. 2011;56(3–4):181–183. [PubMed] [Google Scholar]
- 20.Augustin G. Acute Abdomen During Pregnancy. Springer; Cham: 2018. Torsion of the gravid uterus. [DOI] [Google Scholar]
- 21.Kawakami S., Togashi K., Sagoh T., et al. Uterine deformity caused by surgery during pregnancy. J. Comput. Assist. Tomogr. 1994;18:272–274. doi: 10.1097/00004728-199403000-00020. [DOI] [PubMed] [Google Scholar]