Abstract
As cancer therapies increase in effectiveness and patients' life expectancies improve, balancing oncologic efficacy while reducing acute and long-term cardiovascular toxicities has become of paramount importance. To address this pressing need, the Cardiology Oncology Innovation Network (COIN) was formed to bring together domain experts with the overarching goal of collaboratively investigating, applying, and educating widely on various forms of innovation to improve the quality of life and cardiovascular healthcare of patients undergoing and surviving cancer therapies. The COIN mission pillars of innovation, collaboration, and education have been implemented with cross-collaboration among academic institutions, private and public establishments, and industry and technology companies. In this report, we summarize proceedings from the first two annual COIN summits (inaugural in 2020 and subsequent in 2021) including educational sessions on technological innovations for establishing best practices and aligning resources. Herein, we highlight emerging areas for innovation and defining unmet needs to further improve the outcome for cancer patients and survivors of all ages. Additionally, we provide actionable suggestions for advancing innovation, collaboration, and education in cardio-oncology in the digital era.
Keywords: Cardio-oncology, Prevention, Cardiology oncology innovation network, Collaboration, Innovation, Education
1. Introduction
As cancer treatments have advanced to become more potent and effective over time, their detrimental cardiovascular side effects have also been established. Negative effects, such as left ventricular dysfunction, impact cancer treatment continuation and options, as well as cardiovascular health [1]. To address the negative impacts of vital cancer treatment on the cardiovascular system, cardiologists and oncologists among others partner to increase the longevity and quality of patients' lives. The population of cancer survivors in the United States is estimated to grow to over 26 million people in the next 20 years [2]. Cancer and cardiovascular disease (CVD) share several risk factors and underlying mechanisms, and consequently both conditions often coexist in the same individuals. The mortality risk of cardiovascular causes is greater than that of cancer for some cancer survivors, reinforcing the importance of preventive cardio-oncology for long-term health. Further, overall declines in cardiovascular mortality have slowed over the past decade. A scientific statement from the American Heart Association (AHA) has therefore called for innovation in learning healthcare systems to leverage digital implementation for optimizing cardiovascular health [3]. Indeed, numerous digital health advancements and innovations have the potential to improve cardiovascular health in oncology patients. Exposure to new technologies could improve physical activity and nutrition habits and optimize the prevention and treatment of cardiovascular disease. However, health care professional knowledge of these technologies and applications is not widespread. The lack of awareness of technologies can be remedied through organized communication and collaboration.
Digital technology spans from smart watches measuring heart rate, blood pressure, breathing rate, and notifying others in emergencies, to microchipped medications aiding medication compliance and implantable devices such as cardioverter-defibrillators and pacemakers [[4], [5], [6], [7]]. These burgeoning technologies may improve cardiovascular healthcare for oncology patients, if given the proper platform through a network based on cardio-oncology project partnerships and information sharing. Yet gaps exist in the identification and application of beneficial technologies in cardio-oncology patient populations. There is limited exposure to innovative tools and resources, know-how to implement the tools, and opportunities for collaborative research focused on predictive analytics and machine learning to predict cardiovascular adverse events in cancer patients and survivors.
To address these gaps, the Cardiology Oncology Innovation Network (COIN) was created to improve care for cancer survivors and patients through cooperation among international leaders and learners [8]. The consortium advances healthcare by investigating and disseminating information on cardio-oncology innovations and initiatives, involving stakeholders in fields such as healthcare, industry, education, and informatics. COIN addresses knowledge gaps by providing information about innovative tools and resources that can be shared with oncology patients. Education about the implementation of these tools in clinical practice can also be disseminated through network efforts, especially at the annual summit. Through this collaborative approach, exposure to collective research centered on predictive analytics and machine learning to predict cardiovascular risk in cancer patients and survivors is also shared in the network. The inaugural and second COIN summits were held in December 2020 and 2021, establishing the annual event. A collaborative and educational think tank, cardio-oncology registries, digital health, best practices, technologies for monitoring cardiovascular toxicities outside of the clinical office or hospital, continuing medical education (CME), and other crucial topics were discussed at each summit to advance these initiatives through the multi-stakeholder network.
2. Cardiology oncology innovation network
COIN uses innovative technological strategies to create and improve care delivery options, knowledge, and access for preventive cardio-oncology in the growing population of cancer survivors. Through the tripartite mission of innovation, collaboration, and education, COIN increases accessibility and knowledge of digitally integrated interventions to prevent cardiovascular adverse effects in oncology patients (Fig. 1). COIN increases collaborative efforts among thought leaders in the field, health care professionals, researchers, students, industry, and entrepreneurs to generate new knowledge that is disseminated at annual continuing professional development (CPD) and CME summits and think tanks. Efforts are led by network members around the country to collectively enhance clinical practice and great care of patients for years to come.
Fig. 1.
Cardiology oncology innovation network tripartite mission features.
The rapid expansion of cardio-oncology over the past few years continues to challenge clinicians to digest, interpret, and share an increasing amount of information in an efficient manner. Quality of healthcare indicators improves after practice guidelines are established and distributed. This demonstrates a need for health informatics to harness the power of educational data for medical providers at the point of care for making strategic healthcare decisions incorporating these expert recommendations [9]. Thus, as technology becomes increasingly interwoven with healthcare, COIN is being leveraged to increase knowledge regarding innovative tools for clinical care, along with the ability to further collaborate and advance innovation in the field. Through the network, education of health professionals and patients regarding cardio-oncology, especially with the application of innovation, are key to altering the trajectory of cardiovascular disease in individuals with a current or prior history of cancer. COIN incorporates the experience of our collaborative members to disseminate didactic pathways. Trainees acquiring expertise in this novel field ultimately provide excellent quality of care for generations of future patients. COIN is not only committed to setting a foundation for innovatively managing cardiovascular disease, but also to forming relationships with other medical disciplines to provide comprehensive healthcare before, during, and after cancer therapy. COIN generates easy access to cutting edge information for trainees, practitioners, and investigators. Multidisciplinary collaboration through this network allows for patients to benefit from innovative research advancing the field.
COIN involves a cohesive structure to maximize scientific participation and promote meaningful contribution, with representation from various institutions worldwide. COIN utilizes health informatics to inform medical providers' clinical strategies through the power of data and dissemination of accessible information to healthcare sites. Additionally, education is promoted through the centralization of resources and creation of an innovative didactic curriculum with a patient care delivery focus. COIN is a nonprofit network that helps improve decision making through research and technology. Academic institutions, foundations, and sponsors provide support, through investigator-initiated funding and industry engaged in technology promotion targeting cardio-oncology patient care improvement.
COIN provides a national and international platform for interaction and collaboration among healthcare professionals, scientists, industry, and patients. Jointly, innovative solutions are explored, to overcome challenges involved in providing the most optimal care to patients at the interface of cardiology and oncology. Data-based clinical decision aids for use by healthcare practitioners are being developed to integrate scientific statements and guidelines into cardio-oncology patient care. COIN is contributing actionable insights applicable to clinical practice through leadership in thought, high-impact content and point-of care programming expertise, engagement, and promotion. A timeline of goals and objectives has been charted, displaying planned accomplishment and scholarly work together culminating in collaborative publications. Events and CME activities along with patient-facing innovation opportunities interfacing with technology and industry continue.
To address healthcare disparities and inequities, opportunities are provided to address the health of patients representing various cultural backgrounds, demographics, and geographies, including rural and urban populations. To support the development of de novo cardio-oncology programs, especially amidst the global pandemic, partnerships between the cardiology and oncology communities are facilitated in COIN. The use of virtual tools and technology are also facilitated in the network. With thousands of digital healthcare applications and devices available in the marketplace, COIN helps provide guidance for healthcare professionals and organizations on identifying digital technologies and implementation strategies appropriate for cardio-oncology clinical practice. COIN hosts primary research to establish evidence for their efficacy. Some consumer digital health technologies promise to alleviate burdens faced by cancer patients and survivors at risk for cardiovascular adverse events. However, before healthcare providers or organizations can recommend an application to their patients, user-friendliness and utility must be assured. The American College of Cardiology (ACC) has identified that the best method to support healthcare advances in digital medicine is through a shared vision between a broad range of stakeholders [10]. In keeping with this guidance, COIN assists prevention and treatment efforts by improving familiarity with new cardio-oncology technologies through stakeholder collaboration. During the COIN inaugural summit in 2020, attendees identified four themes to address for the widespread use of digital health and other forms of innovation in cardio-oncology clinical practice: [1] awareness of cardio-oncology digital health tools, [2] knowledge on implementation of cardio-oncology digital health tools [3] exposure to translational artificial intelligence and machine learning research in cardio-oncology and [4] experience using risk models for cardiovascular adverse events in cancer patients and survivors (Table 1).
Table 1.
Barriers and Facilitators of Digital Health and Innovation in Cardio-Oncology Clinical Practice Addressed by COIN SUMMIT 2020/2021 Continuous Professional Development Learning Objectives; COIN = Cardiology Oncology Innovation Network, AI = Artifical Intellegence.
| Awareness | Knowledge | Exposure | Experience | |
|---|---|---|---|---|
| Barriers | Lack of awareness and knowledge about cardio-oncology digital health tools | Complex and complicated digital health and innovation implementation | Lack of widespread translational Artificial intelligence and machine learning research in Cardio-oncology | Limited data access and gaps in provider education and training in utilizing machine learning, and digital tools to predict cardiovascular adverse events in cancer patients and survivors |
| Facilitators | Consistent Information on the efficacy and availability of innovative digital tools for cardio-oncologists and cancer patients and survivors | Continuing education on digital health and innovation implementation in cardio-oncology clinical practice | Increased collaborative research on machine learning and AI application in Cardio-oncology | Increased experiences for providers to utilize dynamic and explainable machine learning predictive risk models for cardiovascular adverse events in cancer patients and survivors |
The COIN mission pillars of innovation, collaboration, and education are being implemented with the development of several care-delivery and research programs. These pillars are led by national and international champions, with cross-collaboration among academic institutions and between academia and industry (software, technological device, and pharmaceutical companies) within the network. A digital health platform, the Connected Health Innovation Research Program (C.H.I.R.P.), has been created for cardio-oncology patients. This is facilitated by collaborations with industry/tech companies that facilitate various initiatives throughout the network. Advanced analytics including artificial intelligence/machine learning are being used, and virtual cardiac rehab and other virtual care initiatives for enhancing the practice of telemedicine or telehealth are being pursued. The collaborative electronic health record dot phrase/templates project for the use and integration of management algorithms in the electronic health records is underway to help optimize the care of survivors of childhood and adult cancers in cardio-oncology. Social media is being leveraged to disseminate information on innovation in cardio-oncology, using the established @Twitter handles @CardioOncCOIN and @CardioOnc_Bot, which also provide avenues for innovative collaborative research. Mobile health applications are being created for education, collaboration, and patient care. Data from the surveillance, epidemiology, and end results (SEER) registries funded by the National Cancer Institute (NCI) may also be incorporated into the global cardio-oncology registry to study prospective and retrospective cohorts.
3. Historical evolution
COIN was created to provide a collaborative space for innovation in cardiology and oncology, and especially at their interface in cardio-oncology for the prevention, screening, management of cardiovascular adverse effects of cancer or cancer therapy. The three tenets of the network mission - innovation, collaboration, and education – form the structure of each Summit. Various forms of innovation are the focus of the network, including artificial intelligence, digital health, and telemedicine. National and global cardiology and oncology influences come together as presenters, moderators, and attendees at the interactive annual summit each year, working together to build a network spanning various cardiology and oncology societies and organizations, in partnership with industry representatives.
4. Network milestones
In order to provide value to the Cardio-Oncology community, COIN has established various outputs that serve as milestones in an effort to reach its overarching mission. These milestones have been pivotal in keeping the program on track throughout its startup years, and they continue to help preserve structure as various COIN initiatives take deeper dives into their respective disciplines. The first years have provided a key foundation in order to ensure successful longevity. At the outset, COIN established a steering committee to serve in an organizational and operational capacity with respect to planning and execution of goals and initiatives. The committee is composed of a diverse panel of volunteers within cardiology and oncology, with terms of service and roles and responsibilities outlined in the COIN founding charter. Key accomplishments of the steering committee in the first years include shaping the vision and objectives of the network, procuring early funding to support top initiatives, and planning and carrying out the first two annual summit meetings (Table 2).
Table 2.
Accomplished and future proposed Cardiology Oncology Innovation Network milestones; COIN = Cardiology Oncology Innovation Network, CME = Continuing Medical Education.
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
|---|---|---|---|---|
| Inaugural annual summit | Annual summit | Annual summit | Annual summit | Annual summit |
| + | + | + | + | |
| Inaugural annual think tank | Think tank | Think tank | Think tank | Think tank |
| Cultivate funding to support initiatives | Cultivate funding to support initiatives | Cultivate funding to support initiatives | Cultivate funding to support COIN initiatives | Cultivate funding to support initiatives |
| Identify steering committee | Further develop committee roles, responsibilities, and terms of service | Maintain/update online enduring CME material | Maintain/update online enduring CME material | Maintain/update online enduring CME material |
| Initial needs assessment | Launch online enduring CME material | Develop mobile site or app to provide point of care reference for drug-drug interactions | Develop mobile site or app to enhance long-term survivorship care/connectivity | Develop a multidisciplinary, innovative online cardio-oncology boot camp to train and continually develop an innovation-focused team-based workforce |
| Determine CME content development, educational medium, educational calendar, and funding | Consolidate cardio-oncology guidelines and recommendations in smartphone app or mobile site | Develop collection of cardio-oncology team-based best practices and how to integrate innovation into care models | Disseminate collection of cardio-oncology team-based best practices and how to integrate innovation into care models | Partner to launch the global cardio-oncology registry to track practice and outcomes and improve patient care especially for racial and ethnic minorities to achieve health equity |
| Identify partners in education, research, and innovation | Design mobile site or app to provide point of care reference for drug-drug interactions and cardiotoxicity | Partner to launch the global cardio-oncology registry to track practice and outcomes and improve patient care especially for racial and ethnic minorities to achieve health equity | Partner to launch the global cardio-oncology registry to track practice and outcomes and improve patient care especially for racial and ethnic minorities to achieve health equity | Additional milestones based on outcomes of think tank in prior year |
| Devise avenues for project management and framework for collaboration | Envision collection of cardio-oncology team-based best practices and how to integrate innovation into care models | Additional milestones based on outcomes of think tank in prior year | Additional milestones based on outcomes of think tank in prior year | |
| Launch Connected Health Innovation Research Program (C.H.I.R.P.) |
The inaugural COIN Summit in late 2020 was a major achievement for the steering committee and program overall. The entirely virtual meeting was instrumental in bringing together thought leaders from around the world with the common goal of advancing innovation and collaboration within cardiology and oncology. The kickoff summit was followed by a leadership think tank in mid-2021 specifically focused on education and collaboration advancements in innovation. The culmination of the first year included launching a virtual site as a platform for the purpose of hosting online continuing education, promoting ongoing global networking, increasing awareness, and helping the program further its core missions.
COIN's second year ventured into tackling specific objectives laid out by the steering and additional key committees. These efforts and successes were presented at the entirely virtual COIN Summit 2021. This follow-up meeting to the inaugural summit was of paramount importance and showcased COIN activities, while demonstrating longitudinal sustainability. A special issue connected to the 2021 Summit with rolling submission through April 2022 highlights much of the work presented and discussed at the 2021 Summit, in greater detail. The second annual think tank was combined with the summit in 2022.
Ongoing milestones set forth by the steering committee include several projects with goals for completion within the first 5 years. A project planned for completion throughout the 5 years is the launch of our online enduring CME material gleaned from each annual summit, as well as additional material introducing various forms of innovation, such as “Artificial Intelligence 101”. A second project with aims for completion by the end of year three is to develop a mobile site or smartphone app to provide a point of care reference for drug-drug interactions and cardiotoxicity risk and management. A third project with a goal of completion at the end of year three is to develop a collection of cardio-oncology team-based best practices and how to integrate innovation into care models. A fourth project with a goal for completion in year five is to develop a multidisciplinary innovative online cardio-oncology bootcamp to train and continually develop an innovation-focused team-based workforce. A fifth project with a goal for completion in years three to five is to collaboratively develop a global cardio-oncology registry with incorporation of informatics, artificial intelligence, and precision medicine, in order to track practice and outcomes trends and support efforts to use innovation to improve patient care while advancing health equity.
5. Sustainability
We will continue to expand this dynamic network to improve the practice of cardiovascular health care, optimize the health of cancer patients and survivors, and evaluate the impact of various forms of innovation in cardio-oncology. We hope to grow the population benefiting from innovation in cardio-oncology. We will continue to include more hospitals and clinics within the network and encourage greater use of these technologies by cancer patients and survivors. We work towards these goals while promoting a culture of teamwork and quality among our diverse network of professionals. While some of the collaborations are early, the network has been actively collaborating with other cardiology and oncology organizations including the International Cardio-oncology Society (ICOS), American College of Cardiology (ACC), and American Heart Association (AHA). These efforts are anticipated to expand the reach of COIN and attract new partner members with interests that align closely with the COIN mission. High standards of quality will be maintained across all domains of COIN – innovation, collaboration, and education. As COIN matures as an organization, metrics will be established in order to gauge each of these areas and ensure consistency in maintaining standards during growth.
We anticipate continued growth of the network with additional end-users on an individual level for trainees and faculty on an annual basis particularly surrounding our summit. The annual summit is self-sustaining from registration fees particularly in the digital era and provides CME content specific to innovation in cardio-oncology and team-based care. Trainees supervised by member faculty submit COIN related abstracts and projects to the annual meeting. In addition, we are hosting a thematic issue of Frontiers in Cardiovascular Medicine focused on digital health technology and innovation in cardio-oncology.
We will continue to actively partner with technology companies in our mission. Innovation tools for the most part will be donated by network tech and industry companies, while some cost will be incurred by the network to avoid any direct costs to patients and limited expenses from individual sites for the research collaboration projects. The creation of these digital resources will be iteratively updated to build upon prior established products to minimize waste and maximize productivity. A particular strength is the close relationship with industry partners that will facilitate incorporation of the newest technologies and allow adaptation to industry standards beyond what is utilized in healthcare. We continue to iterate C.H.I.R.P. as a research platform to interface with tech companies as well as clinicians and patients involved in study projects. We will also maintain study records and compliance and help plan for future network research coordination and infrastructure needs, particularly in preparation for the collaborative multi-center informatics-driven global cardio-oncology registry optimized for precision health and incorporating SEER data.
Alignment of targets for funding will be emphasized at the level of individual institutions and in collaboration across COIN in the pursuit of extramural funding and support. While many COIN participants and local collaborators pursue research in these areas, the hope is to shape several of these local projects into multi-institutional and national efforts with successful large-scale funding. Results from the initial studies will be used to unveil and highlight focus areas that require exploration in an iterative process through additional sources and cycles of funding. Indeed, we will maintain flexibility and adaptability as technology and innovation evolve. We are committed to cumulative and disruptive growth, with focus and emphasis on novel areas with the highest need.
6. Coin summit structure
The annual COIN Summit is virtual and in the style of a steering committee meeting open to all network members, guests, friends, and partners. The virtual environment maintains engagement in the chat box as well as through live speaking among participants. Everyone is welcome to freely use the chat box throughout the sessions for announcing their presence, greeting each other, posing questions, sharing answers and comments, describing network initiatives, and private messaging with friends. Each annual summit opens with introductions from the network steering committee and founder, providing history on the network's beginnings, as well as describing the purpose and nature of the summit and network. This is then followed by perspectives shared by patient representatives/advocates, encouraging us all in our patient-centered network.
Network-wide discussions then ensue, with reports given by network leaders about specific network initiatives, followed by all attendees participating in conversations about national and global partnerships in innovation, collaboration, and education, in the zoom main room, or in multiple breakout rooms, or both. Network-wide discussions in the breakout rooms and the zoom main room then lead into an engagement break with a virtual exhibit during which participants can engage with each other in the chat boxes and also view network announcements and plans scrolling in the zoom main room. The second session for each annual summit consists of rapid abstract presentations by network trainees, moderated by network leaders, and discussed by all attendees. The rapid abstract presenters are selected from among network trainees, labs, and institutions.
The rapid abstracts cover topics in innovation such as artificial intelligence, natural language processing, machine learning, deep learning, big data, predictive analytics, precision medicine, registry data gathering and analysis, and digital health, in the context of cardio-oncology topics including childhood and adult cancer survivorship, strain imaging, cardiomyopathy, chimeric antigen receptor T cell therapy, risk prediction, perioperative care, and cardiac amyloidosis. The abstracts all adhere to prespecified learning objectives (Fig. 2) that capture and address knowledge gaps in innovation, collaboration, and education preidentified by the network steering committee. These learning objectives facilitate continuous professional development during the COIN summit and provide the foundation for enduring online CME materials that will be presented on the COIN website. Another engagement break with a virtual exhibit follows the rapid abstract session, to continue to encourage active networking among participants, even in the virtual settings.
Fig. 2.
COIN SUMMIT 2020/2021 learning objectives.
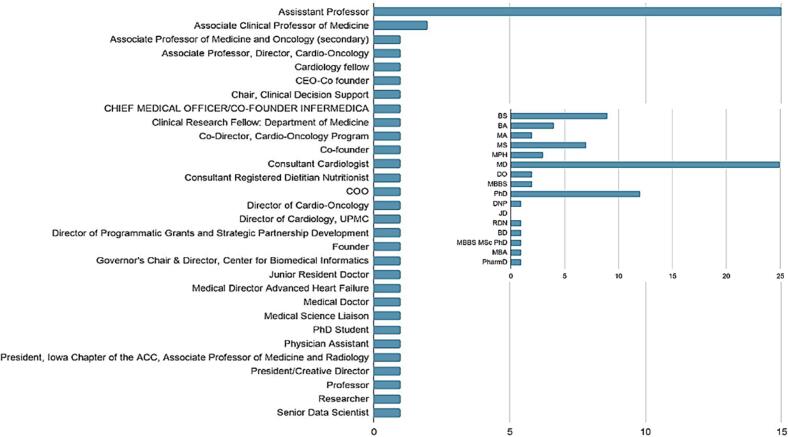
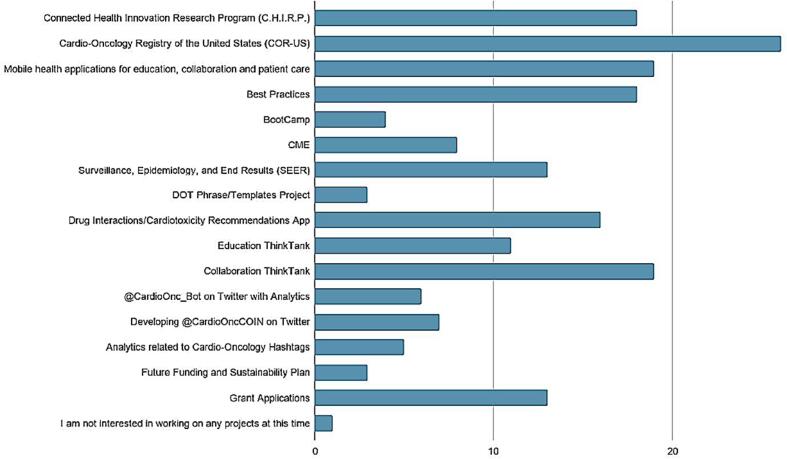
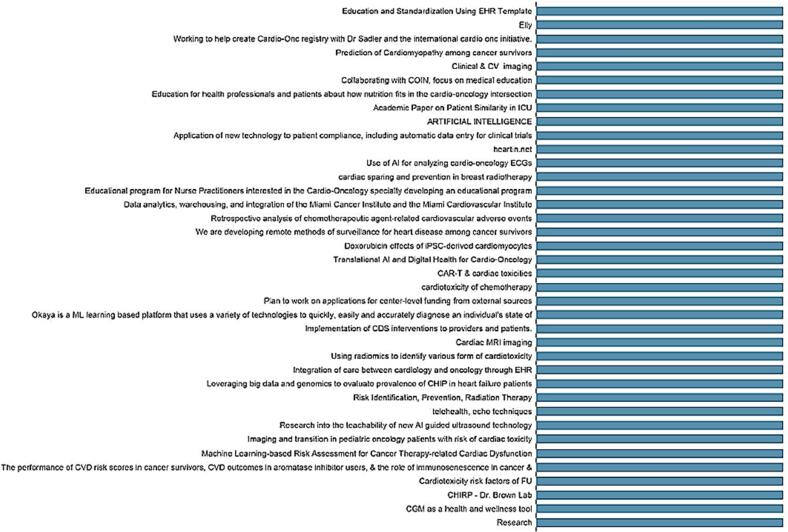
The final session of each COIN Summit consists of three speed panels, then closing remarks. Each speed panel focuses on one of the three tenets of the COIN mission: Innovation, Collaboration, and Education. Each speed panel was moderated by a cardiology or oncology society leader, and also by a partner trainee in 2020. Each panel was composed of an academic panelist, as well as a company/industry panelist. The first speed panel each year focused on innovation in cardiology and oncology. The second speed panel focused on collaboration in cardiology and oncology, and the third speed panel focus on education in cardiology and oncology. A range of cardiology and oncology society leaders composes the mix of panelists and moderators, to give long-ranging insight on network initiatives and direction (Fig. 3, Fig. 4, Fig. 5, Fig. 6).
Fig. 3.
Titles and expertise of the first 50 summit registrants at the inaugural cardiology oncology innovation network summit in 2020. Distribution of titles; Inset, Distribution of expertise. Horizontal axis = number of participants; CEO = chief executive officer, COO = chief operations officer, and ACC = American College of Cardiology.
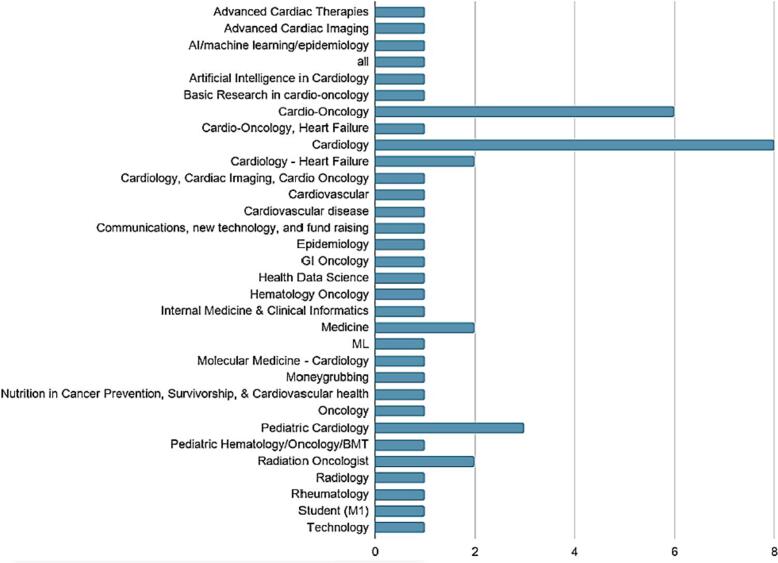
Fig. 4.
Distribution of specialties of the first 50 summit registrants at the inaugural Cardiology Oncology Innovation Network Summit in 2020. Horizontal axis = number of participants; AI = artificial intelligence, GI = gastrointestinal, ML = machine learning, and BMT = bone marrow transplant.
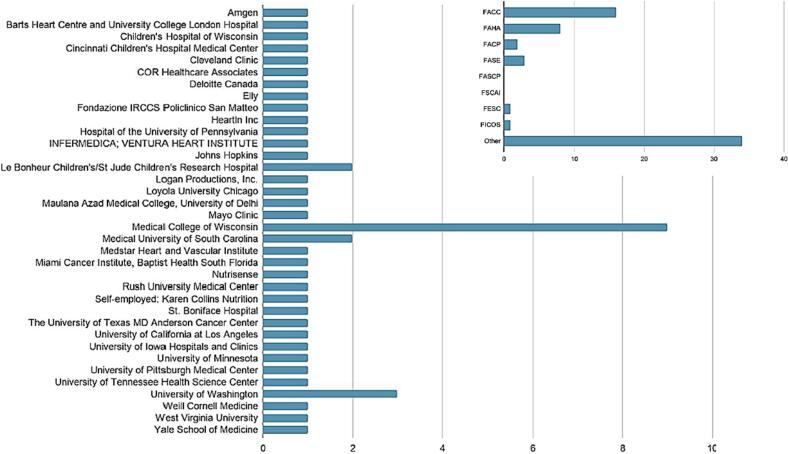
Fig. 5.
Societies and organizations of the first 50 Summit registrants at the inaugural Cardiology Oncology Innovation Network Summit in 2020. Distribution of organizations; Inset, Distribution of societies. Horizontal axis = number of participants.
Fig. 6.
Planned Cardiology Oncology Innovation Network Summit (COIN) Projects of Interest of the First 50 Summit Registrants at the Inaugural COIN Summit in 2020. Horizontal axis = number of participants; CME = continuing medical education.
6.1. COIN Summit 2020 summary
In Session I, the inaugural COIN Summit began with introduction of the network and COIN steering committee members by the network founder Dr. Sherry-Ann Brown. Mr. Jim Logan, a chronic myeloid leukemia (CML) survivor and cardio-oncology patient, then presented a Patient Advocate Perspective, describing ways in which technology may be embraced in patient-centered care. This was followed by Network Mission Updates on Innovation (Dr. Avirup Guha), Collaboration (Dr. Diego Sadler), and Education (Dr. Joshua Levinson). The three central questions for network-wide discussions in Session 1 were: a) How can we best leverage this network for innovation in cardio-oncology?, b) How do we use innovation to care for our patients and ensure we have a complete team-based workforce?, and c) What should our strategic goals be for collaboration?.
In Session II, Dr. Martha Gulati (President-Elect, American Society for Preventive Cardiology) and Dr. Carmen Bergom (Vice Chair, Research Grant Committee, American Society of Radiation Oncology) moderated five cardio-oncology trainee rapid abstract presentations. The five key topics for the abstracts were artificial intelligence, big data, machine learning, predictive analytics, and opportunities for natural language processing in cardiac amyloidosis. In Session III, Dr. Roohi Ismail-Khan (Chair, Advocacy Committee, International Cardio-Oncology Society) facilitated three speed panels which focused on Innovation, Collaboration, and Education in cardiology and oncology. Each panel included a faculty moderator and trainee moderator and perspectives from both academia and industry. Together, these sessions served as a foundation for the integration of emerging technologies in cardio-oncology.
6.2. COIN Summit 2021 summary
In Session I, Dr. Sherry-Ann Brown kicked off the meeting with introduction of the network and Ms. Kathi Hansen, a breast cancer survivor and cardio-oncology patient. Ms. Hansen then presented a Patient Advocate Perspective and challenged us all to advocate for patients by genuinely listening, providing high quality care, and focusing on patient-centered research advancements. This was followed by Network Mission Updates and discussions in breakout rooms. Discussions on the @CardioOnc_Bot and the potential for various smartphone apps in cardio-oncology were mediated by Dr. Craig Beaver and Dr. Avirup Guha in the Innovation room. An open discussion on patient registries and databases was led by Dr. Richard Cheng and Dr. Eric Yang in the Collaboration room. Standardized clinic notes and patient education resources, along with the C.H.I.R.P., a collaborative research program between healthcare and technology companies investigating the use and clinical efficacy of digital health interventions targeted towards cardiovascular health in cardio-oncology patients, were covered in the Education room, guided by Dr. Courtney Campbell and Dr. Austin Steward (at the time a medical student). In two bonus rooms, Dr. Brijesh Patel facilitated a discussion on the prerecorded lecture titled “Artificial Intelligence 101” presented by Dr. Irving Loh, and Mrs. Juby George-Vaze guided a group on the discussion of blockchain, global health innovation, and quantum computing.
In Session II, Dr. Anne Blaes (Past Chair, American Society of Clinical Oncology Cancer Survivorship) moderated five cardio-oncology trainee rapid abstract presentations. The five key topics for the abstracts were digital health, opportunities for artificial intelligence in strain imaging, opportunities for machine learning in risk assessment, opportunities for mobile health in survivorship, and opportunities for artificial intelligence and precision medicine in the global cardio-oncology registry. In session III, Dr. Michael Fradley (Board of Directors, International Cardio-Oncology Society) facilitated three speed panels which focused on Innovation, Collaboration, and Education in cardiology and oncology. Each panel included a moderator and perspectives from both academia and industry. These sessions provided space for idea-sharing, hypothesis generation, and networking among cardiology and oncology leaders to stimulate further discovery and innovation in cardio-oncology.
7. Patient perspectives in the cardiology oncology innovation network
Following the network introduction and history, perspectives were shared by a cardio-oncology patient representative each year - Mr. Jim Logan in 2020 and Ms. Kathi Hansen in 2021.
7.1. Digital technologies paradigm shift for patients
In 2020, Mr. Logan described his experience as a patient living with CML for over 20 years, having been in some of the original clinical trials for mainstay treatment, and now being managed in cardio-oncology. Mr. Logan highlighted the paradigm shift in the use of digital technologies in the midst of the pandemic. Mr. Logan provided great insight for patients and health care professionals in the network, to help ensure that network pursuits are extremely applicable for patients.
7.2. Patient advocacy in cardio-oncology
In 2021, Ms. Kathi Hansen shared her perspectives as a patient representative. Her experiences as a cancer survivor and now also as a cardiology patient have led her to become an advocate. An advocate is a person who offers support and information to those in need, or who publicly supports or recommends a particular cause or policy. Ms. Hansen's advocacy started as a breast cancer peer counselor, working with a number of national organizations to share information and support with women and men on their breast cancer journeys. This involved answering calls on a 24/7 hotline, being matched with patients for more in-depth conversations, and volunteering at retreats for women with breast cancer as they process and heal during and after their cancer experiences. Using her 28 years of teaching experience, she also worked with a local foundation, promoting cancer risk reduction strategies with middle and high school students. She also provided the patient perspective on projects with a major pharmaceutical company and a prominent national medical center. Ms. Hansen also became involved in public policy advocacy, working with state and federal lawmakers on issues like research funding, screening programs, tobacco control, and palliative care. Putting a face on cancer and heart disease, using her personal story, and presenting relevant facts and data–these are how she uses her experiences to help bring about changes that can positively impact so many people. As illustrated, there are many ways in which one can be a patient advocate, and Ms. Hansen reminded us that each of us needs to be a patient advocate as well – an advocate for patients. How can we do that? In three simple ways:
-
•
First, listen so you know what patients think, feel, and want. Ask questions. Hear what they aren't saying as well as what they are. Take the necessary time and always respect what you discover.
-
•
Second, provide the best possible care for all patients. Think about and try to reduce implicit biases that may affect how some patients are treated. Strive to understand the barriers that patients may face in things like getting to appointments, having tests, and obtaining medications. Be creative in helping them overcome these barriers–do what you can to lessen or remove barriers to care in your clinic or hospital.
-
•
And finally, ensure that every advance in research always has the patient at its heart. Yes, there are puzzles to solve, conundrums to unravel, secrets to discover, connections to be made, and papers to be published. But the reason you do all those things? It really must be all about the patient. If it's not, then your time, energy, and expertise are not serving the people your research may impact.
If you do these three things–listen to patients, provide the best possible care to all patients, and ensure that research has the patient at its heart, then you will be a true patient advocate as well.
8. Network partnership updates
8.1. 2020 network mission updates
8.1.1. Innovation: @CardioOnc_Bot
Dr. Avirup Guha, who was an assistant professor of cardiovascular medicine at the Harrington Heart and Vascular Institute at Case Western and is now the Director of Cardio-Oncology at the Medical College of Augusta in Gerogia, described the @CardioOncBot created to keep up with and share cardio-oncology literature. The bot runs 24/7, and output increases in volume during national conferences in which the use of popular cardio-oncology hashtags is increased. The bot may provide opportunities as an educational and research tool to keep up-to-date with new discoveries and best practices in cardio-oncology.
8.1.2. Education: Dot Phrase Templates
Dr. Joshua Levenson from the University of Pittsburgh Medical Center shared about the Dot Phrase Templates project envisioned by Dr. Courtney Campbell, with input from Dr. Sherry-Ann Brown and Dr. Levenson. The project in collaboration with ICOS, ACC, and AHA leverages standardized clinical note templates, smart phrases, and smart lists for use locally and globally in electronic health records. These templates provide an opportunity for education, efficiency, and consistency in cardio-oncology patient charts to capture complex and extensive cancer therapy history and their associated cardiotoxicity risk assessment and management, supported by references from published literature. In collaboration with partner organizations and societies, an online repository has been collated and is hosted on the COIN website (CardioOncCOIN.Org).
8.1.3. Collaboration: global cardio-oncology registry and advocacy
Dr. Diego Sadler from Cleveland Clinic Florida discussed the international collaborative cardio-oncology efforts for advocacy, community engagement, and building the global cardio-oncology registry. A program was launched for formal collaboration between ACC cardiologists and American Society for Clinical Oncology (ASCO) oncologists at the level of each geographic state, with a Chapter-Section grant from the ACC Board of Governors supported by the ACC Cardio-Oncology Section at the time led by Dr. Ana Barac. The program was formed to assess interactions and collaborations between cardiologists and oncologists at that community level and establish awareness and education addressing knowledge gaps about cardio-oncology in the community and also in academic centers. The program was launched nationally and internationally with wide participation from many members from different states and countries, including the US and Canada, as well as nations in Europe, Asia, Africa, and Latin America. The program partners with cardio-oncologist members of the AHA, European Society of Cardiology (ESC), and ICOS, in addition to ACC and ASCO. Multiple algorithms and protocols are in development to support work in practice patterns algorithms, registries for short- and long-term outcomes, access to cardio-oncology care in different settings, real world data, and clinical trials. The program will also evaluate socioeconomic barriers, health care disparities, quality of life, access to care and community awareness. and disparities in healthcare and cardio-oncology.
8.2. 2021 network updates and discussions in breakout rooms
In 2021, five breakout room were utilized to optimize simultaneous network discussions. Innovation was the focus of the first breakout room co-moderated by Dr. Craig Beavers and Dr. Avirup Guha, with discussion ranging from smartphone apps to a potential publication on the @CardioOnc_Bot. Collaboration was the focus of the second breakout room co-moderated by Dr. Eric Yang and Dr. Richard Cheng, with discussion ranging from biomarkers to study and implementation of guidelines. Education was the focus of the third breakout room co-moderated by Dr. Austin Steward (at the time a medical student) and Dr. Courtney Campbell, with discussion ranging from Dot Phrase Templates in the electronic health records to the C.H.I.R.P.. In the fourth breakout room Dr. Brijesh Patel moderated the viewing and discussion of a pre-recorded presentation on Artificial Intelligence 101 by Dr. Irving Loh, who is a member of the World Health Organization and United Nations working topic groups for AI. In the fifth breakout room, Mrs. Juby George-Vaze led a discussion on blockchain, global health innovation, and quantum computing. Subsequently, scribes/speakers from the first three breakout rooms summarized breakout room discussions for all network-wide participants in the main zoom room.
8.2.1. Innovation breakout room
This room hosted a large focus on current cellphone-based tools being utilized in the care of cardio-oncology patients, in addition to discussing potential ideas for manuscripts about the Twitter @CardioOnc_Bot, and communication tools to improve multi-disciplinary care of cardio-oncology patients.
Multiple smartphone-based tools are currently being developed by members of COIN, focusing heavily on risk stratifying patients and point-of-care drug-drug interaction assessment. The apps would be stand-alone, or there may be communication with the electronic health records (EHR). Direct EHR integration across health systems may be challenging. A company collaborator in COIN is leading the charge to solve this issue with a patient-centric app co-managed by a patient to ensure their medication list is current, mobile, and accessible at their cardiology and oncology appointments. Collaboration across academia, industry, and various types of healthcare providers was a general theme emerging from this discussion.
Ideas for data analytics for manuscript publication on the Twitter @CardioOnc_Bot was discussed by Dr. Avirup Guha. He created this cardio-oncology retweeting bot using Python software. The bot is hosted on Twitter to improve the delivery of cardio-oncology content to end-users. The field of cardio-oncology is fairly new, and research is being rapidly created and disseminated through various sources such as table of contents, emails to authors, and individual journal-specific methods such as Twitter handles. The @CardioOnc_Bot is a Twitter handle that one can follow to streamline the cardio-oncology literature feed. The bot retweets any tweets associated with #CardioOnc, #CardioOncology, #OncoCardiology, #JACCCardioOnc, or #ESCCardioOnco. In addition, all tweets coming from the Twitter handles of @ICOSociety and @CardioOncCOIN are retweeted. Currently, there are over 550 followers of the @CardioOnc_Bot on Twitter, with 4.1million impressions for #CardioOnc and 1.7 million impressions for #CardioOncology in May–June 2022 at the time of submission of this manuscript.
The use of innovation to improve the quality of patient-related discussion was also discussed. VitalEngine.Org was discussed by Dr. Mary Branch who has found this Health Insurance Portability and Accountability Act (HIPAA) compliant website and mobile application clinical collaboration platform quite useful in improving communication with our oncology colleagues. COIN is discussing potential network-wide use of this tool, as communication is key in cardio-oncology. The breakout room ended with a discussion regarding policy changes to improve multidisciplinary care and more readily include cardio-oncology considerations in oncology care models.
8.2.2. Collaboration breakout room
Collaboration in cardio-oncology remains a critical yet challenging need due to heterogeneous healthcare systems. Barriers to information-sharing, resource availability, and funding also limit the ability to conduct effective clinical work and research. Recent advancements and innovative strategies to further improve collaborative efforts within cardio-oncology were discussed by a broad group of thought leaders spanning cardiology and oncology, including those from varying practice types (academic institutions, private practice, and hospital employed) to industry representation.
Initial discussion revolved around key registry developments. Host-cancer therapeutic interactions are being actively investigated through post-marketing, real world data examining clinical features of cardiotoxicity [11], immune checkpoint inhibitor myocarditis [12] and chimeric antigen T-cell therapy [13]. Advocacy at the state, national, and international levels is being developed avidly for the global cardio-oncology registry and in ICOS [14,15].
Regional/institutional biobanks with the ability to test for genetic mutations and variants which may yield insights into cardiotoxicity risk were identified as a topic of interest, although limited by logistical barriers between institutions. Healthcare systems such as at the University of Washington and the University of California have started initiatives in wide testing of their patient populations in the hopes of providing large-scale analyses of patients to predict cardiovascular and/or cancer risk [16,17]. Ideally, further collaborative work in this regard will lead to advances in implementing principles of precision medicine in cardio-oncology patients.
Relationships with our industry partners were also discussed to catalyze advances in cardio-oncology innovation research in COIN. Cardiovascular outcomes seen in Food and Drug Administration (FDA) approved cancer clinical trials seem to pale in comparison to the normal historical time course of cardiovascular disease-based registries [18]. Further collaboration is needed to optimize appropriate cardiovascular toxicity screening and surveillance during initial Phase I-III trials to ensure adequate identification of cardiovascular risk and safer deployment of these agents when they are used in higher risk populations in the post-marketing period [19]. Oversight and involvement—and perhaps redefining of—cardiac-related common terminology criteria for adverse events (CTCAE) will also ensure adequate cardiotoxicity monitoring and strategies to attenuate such toxicities. The partner society ICOS has recently published a statement to help address this [20].
8.2.3. Education breakout room
The conversation in the Education breakout room was directed towards how innovative and innovation education and training are shaping the field of cardio-oncology, at the interface of cardiology and oncology, with salient suggestions as follows. Cross-training between oncologists and cardiologists is needed so that cancer and cardiovascular treatment programs can be designed that include practical considerations for the patient from each specialty. All of the training discussed above is also relevant to primary care providers (PCPs), since the care of cancer survivors is gradually transitioned from oncologists to PCPs after treatment concludes. PCPs need to be aware of advances in cancer treatment programs and be equipped with the knowledge and tools to care for their patients' cardiovascular health.
The use of digital health tools may benefit health practitioners by facilitating the detection of early signs of cardiovascular disease, to better monitor individuals who already have cardiovascular disease, and to observe in real time how patients respond to cardiovascular disease treatment. Development of C.H.I.R.P. to research how digital health tools provide these benefits was discussed. The primary objective of C.H.I.R.P. is to conduct retrospective, prospective, and case studies on the clinical efficacy and adoption of digital health interventions that are targeted towards maintaining and improving cardiovascular health in the cardio-oncology patient population. Further research from C.H.I.R.P. and other innovation programs will be valuable in guiding cardio-oncology patients and their care providers towards digital health tools that are efficacious and suited to meet patients' personal needs.
Indeed, commentary on the impact of COVID-19 on cardio-oncology care acknowledged the reality that training on the use of digital health tools for telehealth and e-consults should be a focus for all of our institutions as we continue to adapt to a health technology-centered landscape. The session concluded with remarks stressing the necessity of providing equitable care to racial and ethnic minorities, as research demonstrates these patient populations experience poorer health outcomes with respect to cancer, cardiotoxicities, and follow-up care.
8.2.4. Network-wide discussion
Network-wide discussions were facilitated by Dr. Irving Loh (Member, World Health Organization/United Nations Artificial Intelligence Working & Topic Groups), Dr. Catherine Handy Marshall, and Dr. Carri Glide-Hurst (Scientific Education & Program Development, American Society Radiation Oncology). Dr. Irving Loh is a member of the World Health Organization and United Nations working topic groups for AI. Dr. Catherine Handy Marshall is a member of the ASCO Women Who Conquer Cancer Network. She is a medical oncologist at Johns Hopkins, with a clinical and research focused mostly on long term survival and cardiovascular health for those living with prostate cancer. Dr. Carrie Glide Hurst is a member of the Scientific Education and Program Development Committee for the American Society for Radiation Oncology (ASRO) and a radiation oncology physicist at the University of Wisconsin Madison, where she leads the physics division to support radiation oncology services. All summit attendees participated in discussion of three key questions:
-
•
Question 1: How can we best leverage this network for innovation in cardio-oncology?
-
•
Question 2: How do we use innovation to care for our patients and ensure that we have a competent team-based workforce?
-
•
Question 3: What should our strategic goals be for collaboration?
The overall network-wide discussion revolved around concepts of what makes a good collaborative network focused on innovation in cardio-oncology, from both a research and a clinical perspective. Among other needs, a strategic goal of this collaboration was considered to develop innovative and efficient methods to extract the most information from existing registries, as well as develop new registries that include complete data sets. More so, anticipation of future trends or goals, inasmuch as that is possible, was desired. While traditional oncology and cardio-oncology registries, like the SEER database and the Women's Health Initiative have been productive, many do not represent complete data sets for the cardiologist, or cannot anticipate questions that may arise in the future. Discussants therefore pondered how to leverage advanced technologies for data and trends that are not “visible to the human eye”, leading to conversations around a role for advanced artificial intelligence algorithms. Finally, we emphasized that prior efforts have regularly failed to include diverse and representative patient populations or to include social determinants of health. This collaborative network must have racial and ethnic diversity and the study of health disparities and equity as a primary driver in designing any registries and in formulating research questions. Once data are collected and interpreted, it will be vital to determine how can they be translated into clinical practice and public health applications, and how these changes can be disseminated to frontline clinicians and care providers. Finally, once these principles have been applied, the work would be incomplete without network-wide assessment of the practicality, efficacy, and safety of any changes put into action.
Another area that generated significant interest during the discussion was the use of “dot phrases” within the electronic heath record. These represent shortcuts in which typing a phrase preceded by a period or dot (e.g., “.cardiooncnote”) brings up a template, worksheet, phrase, or specified test results. The primary interest, in this case, was for template clinic or consult notes that not only help direct note writing, but also standardize data collection and documentation and allow for easier data mining through either automated data pull or free text searches with artificial intelligence software. Use of shared templates by providers within a network would streamline data collection for registries, research, and so on.
In addition, existing cardio-oncology risk calculators are limited, and while validated in published manuscripts and made available for free, they are outside of the medical record. Several members of the group discussed the best approach to incorporate those and use such tools in our documentation, patient education materials, and dissemination to our colleagues in other disciplines or who serve as primary care providers. An example discussed was the Childhood Cancer Survivor Cardiovascular Risk Calculator. Understanding the unique cardiovascular characteristics of children undergoing cancer therapies has paved the way for comprehensive care prior to, during, and after cancer treatment [21]. Survival rates for pediatric cancer patients have significantly increased. As these children become adult survivors of childhood cancers, they are at risk for long-range cardiovascular adverse effects of cancer therapy. A discussant commented that to assess cardiovascular risk in this population, they go to the public website and insert deidentified patient data, then copy and paste the predicted risk results into a patient note in the EHR. This process is cumbersome and could be made much more user friendly by incorporation of the risk calculator into a flowsheet within the EHR, and perhaps having some of the necessary data pulled directly into the worksheet, rather than manual entry. While there was general agreement as to the utility of such tools, some discussants expressed hesitation to have more “pop-up” messages or alerts in the EHR and additional steps that could hinder progress on a busy clinic day.
Taken together, the key themes in the network-wide discussion led to the following points for action.
Question 1: How can we best leverage this network for innovation in cardio-oncology?
Action Points:
-
•
Recruit more junior faculty and trainees into our networks, particularly those with backgrounds in computer science and data science, in order to become more facile in big data analytics and artificial intelligence (AI) including machine learning;
-
•
Develop large databases that include electrocardiograms and echocardiograms for predictive analytics;
-
•
Design retrospective and prospective preclinical, clinical, and translational studies that can help inform clinical practice and precision public health;
-
•
Establish multidisciplinary teams that provide input on innovative research project design from inception to completion;
-
•
Involve digital natives who understand and are interested in further developing AI especially machine/deep learning solutions;
-
•
Incorporate health professionals who are digital immigrants and can help ensure that the work translates well into clinical practice and public health;
-
•
Work together to improve the explainability of AI and therefore lower some of the barriers to clinical implementation.
Question 2: How do we use innovation to care for our patients and ensure that we have a competent team-based workforce?
Action Points:
-
•
Incorporate existing patient care pathways, risk calculators (e.g., Childhood Cancer Survivorship Study risk calculator [[22], [23], [24]], or other risk calculators [[25], [26], [27], [28]]), and other resources into the electronic medical record to assist with clinical decision-making at the point of care and to support clinician and patient education;
-
•
Capitalize on electronic medical record infrastructure that can automatically retrieve information about cancer treatment for a given patient by using dot phrases (e.g., incorporation of the types and doses of cancer treatments, including oral agents, from Beacon – the oncology module for EPIC);
-
•
Inclusion of primary care doctors into the Cardio-Oncology innovations team as many cancers are now chronic diseases and some primary care doctors have survivorship interests this [29,30];
-
•
Establish common strategic goals for collaborative innovation with cancer care organizations such as the National Cancer Institute and the American Cancer Society.
Question 3: What should our strategic goals be for collaboration?
Action Points:
-
•
Collect cardiotoxicity data serially from within the electronic medical records across specialties;
-
•
Use natural language processing to collect data buried within reports or notes;
-
•
Leverage big data (e.g., imaging registries, Women's Health Initiative, National Cancer Institute's Surveillance Epidemiology and End Results (SEER) database) to answer novel research questions;
-
•
Ensure that databases and registries include patients that can serve as a non-cancer control populations from the same geographic region(s) (e.g., 5 % of the SEER database population is a healthy cohort from the same region(s) as their cancer counterparts that can be used for comparison studies);
-
•
Incorporate socioeconomic information include zip codes, state, and/or county in registries and trials to study regional differences in cardiotoxicity and to facilitate advocacy for addressing health disparities especially in racial/ethnic minorities, who are at greatest risk for experiencing cardiovascular toxicities;
-
•
Utilize cardio-oncology registries as platforms for innovative clinical trials;
-
•
Use AI to more efficiently identify and match patients for clinical trials [31];
-
•
Maintain a platform for ongoing communication regarding new or evolving opportunities for strategic collaboration.
These action points can form the foundation for future collaboration and innovation in COIN.
9. Network rapid abstract presentations
9.1. 2020 trainee abstracts
The rapid abstract session in 2020 was co-moderated by Dr. Martha Gulati, who was the president-elect for the American Society for Preventive Cardiology (ASPC) and Dr. Carmen Bergom, who was the Vice Chair of the Research Grant Committee for the American Society for Radiation Oncology (ASRO) [32]. The first abstract on artificial intelligence was presented by Dr. Fatma Gunturkun (at the time a postdoctoral research fellow in cardiovascular data science and bioinformatics), who reported on using deep learning for improved prediction of late-onset cardiomyopathy among childhood cancer survivors from the St. Jude Lifetime Cohort (SJLIFE) [33]. The second abstract on big data was presented by Peter McGranaghan (at the time an academic institution data analytics consultant and PhD candidate), who reported on cardiovascular and cerebrovascular events associated with cancer surgery in the United States National Inpatient Sample [34]. The third abstract on opportunities for natural language processing was presented by Dr. Courtney M. Campbell (at the time a cardiology fellow), who reported on delays in diagnosis of transthyretin cardiac amyloidosis after establishing cardiac care [35]. The fourth abstract on machine learning was presented by Dr. Akshee Batra (at the time a medical student), who reported on cardiovascular events associated with chimeric antigen receptor T cell therapy in a cross-sectional FDA adverse events reporting system analysis [36]. The fifth abstract on predictive analytics was presented by Dr. Yadi Zhou, who presented on machine learning-based risk assessment for cancer therapy-related cardiac dysfunction in 4300 longitudinal oncology patients [37].
9.2. 2021 trainee abstracts
In 2021, the Trainee Rapid Abstracts presentations were moderated by Dr. Anne Blaes, who is a Past Chair of the ASCO Cancer Survivorship Committee [32]. The first abstract on digital health was presented by James MacLeod (at the time a medical student), who reported on building the C.H.I.R.P. involving patient engagement in digital transformation [8,38]. The second abstract on strain and opportunities for artificial intelligence was presented by Dr. Ogochukwu Ezoke, who reported on surveillance in pediatric cardio-oncology: an assessment of the prognostic value of global longitudinal strain in detecting anthracycline associated cardiomyopathy. The third abstract on risk assessment and opportunities for machine learning was presented by Dr. Sebastian Romann, who presented on risk stratification in cancer patients in a single-center cohort study [39]. The fourth abstract on survivorship and opportunities for mobile health was presented by Wadsworth Williams (at the time a medical student), who reported on pediatric Cardio-Oncology: The Changing Role of Interdisciplinary Survival Care. The fifth abstract on the global cardio-oncology registry and opportunities for artificial intelligence and precision medicine was presented by Dr. Abdullah Sarkar, who reported on the structure for a multi-national collaboration to build the registry [8,40].
10. Network speed panels
10.1. 2020 panels
In 2020, the Speed Panels session was overall moderated by Dr. Roohi Ismail- Khan, who was the Chair of the Advocacy Committee for the International Cardio-Oncology Society. Dr. Roohi Ismail-Khan introduced the moderators and panelists for each speed panel.
10.1.1. Innovation speed panel
Our Innovation speed panel was moderated by Dr. Donald Lloyd-Jones, who was the President-Elect of the American Heart Association, along with Hematology/Oncology fellow Dr. Prantesh Jain. Dr. Dipti Itchhaporia, who was the Vice President of the American College of Cardiology and Chair of the ACC Health Equity Task Force launched in 2020, was our academic panelist, and Nikhil Pooviahl, who is the co-founder of Elly and a Shark Tank Winner, was the company/industry panelist.
The Innovation speed panel highlighted achieving health equity in innovation, with salient suggestions as follows:
-
•
Recognize that while innovation is critical to moving our field forward, innovation can uncover or exacerbate health disparities;
-
•
Determine how to build innovation features that ensure and drive health equity;
-
•
Leverage culture and strategy to optimize innovation for health equity;
-
•
Equitably harness technology to facilitate access to care and participation in clinical and translation research;
-
•
Employ individual clinician advocacy efforts as well as those of professional societies and public health organizations to achieve health care equity through innovation;
-
•
Design innovative research agendas that are optimal for traditionally marginalized populations;
-
•
Invest in traditionally underrepresented subpopulations by supporting the cost of innovative interventions so that the expenses do not impede implementation in the populations that can be most impacted in cardio-oncology health equity work (e.g., sponsored penetrance of smart phones into underserved populations);
-
•
Lead health equity efforts in digital transformation that improve accessibility and support optimal implementation;
-
•
Create a path of beneficence, justice, and human connection, as we advance innovation in cardio-oncology health equity.
10.1.2. Collaboration speed panel
The Collaboration speed panel was moderated by Dr. Anne Blaes, who is a Past Chair of the ASCO Cancer Survivorship Committee, along with PhD candidate in Oncology Elizabeth Polter. Dr. Julie Gralow, who is the Chief Medical Officer of the ASCO, was our academic panelist, and Dr. Indrajit Choudhuri. who is the Chief Executive Officer of MediCardia, was the company/industry panelist.
The Collaboration speed panel highlighted potentially using innovative platforms to harmonize collaboration between cardiology and oncology, with salient suggestions as follows:
-
•
Develop innovative collaborative platform for near-real time dissemination and discussion of new oncology treatments with potential cardiotoxicity and ways to study and prevent these toxicities;
-
•
Establish digital engagement committee to better engage patients (e.g., using mobile phone text messages to collect patient reported outcomes for clinical trials and registries);
-
•
Leverage technology to facilitate collaboration among members of cardiology and oncology professional organizations on the development and revisions of cardio-oncology clinical guidelines and expert consensus statements;
-
•
Use cloud-based platforms to harness the information available from clinical and scientific data sources, such as data from the EHR and/or genomics [41] in the near future;
-
•
Create the regulatory and legal infrastructure to allow cancer centers and cardiology/cardio-oncology programs to bring information together and share data for collaborative machine learning and natural language processing studies.
10.1.3. Education speed panel
The Education speed panel was moderated by Dr. Erin Michos, who is on the Board of Directors for the ASPC and an Associate Professor of Medicine at Johns Hopkins School of Medicine, along with Cardiology fellow Dr. Douglas Leedy. Dr. Kathryn J Ruddy, who is a member of the ASCO Health Equity and Outcomes Committee and a Professor of Oncology at Mayo Clinic was our academic panelist, and Dr. Peter Orton, who is the Chief Science Officer of WellFlix was the company/industry panelist.
The Education speed panel discussed the use of innovative technology in medical and patient education, with salient suggestions as follows:
-
•
Identify an inclusive group of stakeholders for cardio-oncology education, including medical and graduate students, residents, fellows, hematologists/oncologists, cardiologists, primary care physicians, advanced practice providers, pharmacists, and other cardiovascular team members across subspecialties in heart failure, heart rhythm, interventional cardiology, cardio-oncology, and so on, as well as our patients;
-
•
Develop innovative case-based cardio-oncology education not only at the fellow level, but also at the resident, medical student, and staff level;
-
•
Use virtual platforms to expand the reach of conferences that have traditionally been restricted to in-person learning, with future integration of simulations and rich media;
-
•
Determine the best technology platforms to deliver education (e.g., Twitter journal clubs, educational apps, recorded CME events, real-time streaming events);
-
•
Use patient portals before and after clinic or hospital visits to ascertain patient reported outcomes and then deliver tailored patient education, resources, and health care team access;
-
•
Create and utilize of mobile apps to collect patient reported information and deliver patients ongoing education in frequent but smaller quantities [42];
-
•
Advance connected care with Long Term Evolution (LTE)-enabled (i.e., 4G wireless broadband) remote monitoring to increase equitable access, optimize outpatient management, and reduce hospitalizations [43,44];
-
•
Facilitate self-advocacy to encourage healthy lifestyle behaviors (e.g., message reminders to exercise and personalized videos for self-care before, during, and after cancer treatment), with potential to improve outcomes;
-
•
Emulate innovative behavioral modeling video enactment customized for patients to improve self-efficacy for future behavior change;
-
•
Promote existing patient-directed digital educational formats such as CardioSmart;
-
•
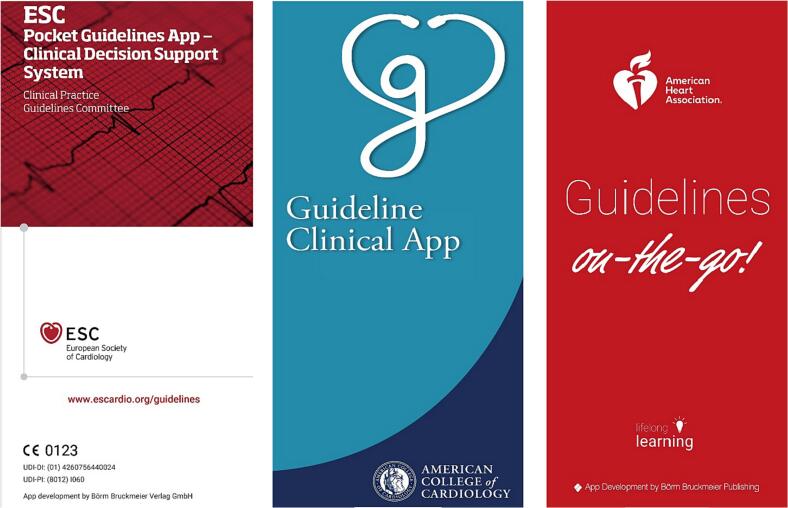
Translate oncology practice guidelines in easy to understand and readily accessible interactive formats via mobile apps accessed by both health care professionals and patients.
10.2. 2021 panels
In 2021, the Speed Panels were overall facilitated by Dr. Michael Fradley, who is a member of the Board of Directors for the International Cardio-Oncology Society and associate professor of clinical medicine at the University of Pennsylvania. Dr. Fradley introduced the moderators, who in turn presented each panelist.
10.2.1. Innovation speed panel
The Innovation speed panel was moderated by Dr. Julie Gralow, who is the Chief Medical Officer of ASCO. Dr. Karol Watson, who is an Association of Black Cardiologists Spirit of the Heart Distinguished Leader and a professor of Cardiology at the University of California at Los Angeles, was our academic panelist, and Robert Longyear, who is Vice President of Digital Health & Innovation for Avenue Health was the industry/company panelist.
The Innovation panel discussion emphasized achieving health equity in innovation initiatives, by listening and building solutions, with salient suggestions as follows:
-
•
Recognize that attempts to create equity must start by asking diverse questions and engaging diverse community of thought leaders, investigators, innovators and funders in problem-solving with equity implications in mind from the beginning;
-
•
Adopt a patient-centered focus for technology-dependent innovations to assess and facilitate broadband internet access of the patient population, technology access such as smartphones, and technology literacy, and including work-arounds and technology assistance where needed to avoid disparities;
-
•
Generate multi-lingual and multi-cultural platforms;
-
•
When conducting research in under-resourced settings, incorporate into the protocol inclusion of training and resources that serve the research itself but can also be left with the local health-care providers and patients to enhance health-care delivery in a more sustained manner;
-
•
Harness information from lower cost digital and connected medical devices that can be distributed or centralized in resource-constrained settings (e.g., blood pressure monitors, electrocardiograms, pulse oximeters) to better identify and serve cardio-oncology subpopulations that need more intensive monitoring and those that require less.
10.2.2. Collaboration speed panel
The Collaboration speed panel was moderated by Dr. Kim Williams, who is a Past President of the American College of Cardiology (ACC), as well as the Chief of Cardiology and a Professor of Medicine and Cardiology at Rush University. Dr. Eduardo Sanchez, who is the Chief Medical Officer for Prevention for the American Heart Association (AHA), was our academic panelist, and Dr. Saira Haque, who is the Senior Director for Clinical Informatics at Pfizer was the industry/company panelist.
The Collaboration panel discussion highlighted ensuring common ground in cancer and cardiovascular disease prevention, with salient suggestions as follows:
-
•
Recognize and address disparities in race, ethnicity, socioeconomics (such as education attainment and household income), insurance status, and other patient social needs as we reach across various aisles to form a health equity collaboration hub for our patients and research endeavors;
-
•
Partner with primary care physicians whose office are the starting point for many patients accessing the health care system for preventive care;
-
•
Inform patients not just on what they can do to improve their health but also helping them implement change, by elucidating the context of their daily life and the availability or lack thereof regarding their community resources available to support lifestyle changes;
-
•
Incorporate the American Heart Association's Life Simple 7 (optimizing the following for ideal cardiovascular health: cholesterol, blood pressure, blood sugar, weight, diet, physical activity, and smoking status) [45], cardiorespiratory fitness, novel and established risk calculators in our efforts to address shared risk factors for heart disease and cancer;
-
•
Include non-medication oriented wellness interventions such as healthy eating, exercise, and weight reduction or maintenance that represent risk mitigation targets and prevention targets;
-
•
Establish interdisciplinary collaborative training opportunities and guidelines [30,[46], [47], [48]] and treatment and prevention guidelines [20,28,[49], [50], [51], [52], [53]] for cardio-oncology that can be accessible to clinicians, researchers, and other members of the cardiovascular team;
-
•
Harmonize data dictionaries and definitions to aid the progress of AI, machine learning and predictive analytics that ultimately can be used to develop management pathways to assist patient care through development of interactive mobile apps [8,54];
-
•
Collaborate across sectors by leveraging SMART (Substitutable Medical Applications Reusable Technologies) on FHIR (Fast Healthcare Interoperability Resources) for interoperability to integrate various digital health applications relevant to cardio-oncology patients and interdisciplinary research into the electronic health records;
-
•
Facilitate secure, private, and confidential health information exchange between electronic health records and health care organizations and industry partners, including departments of public and population health to facilitate patient care, registries, and clinical trials;
-
•
Call the attention of chief medical information officers in major medical centers to the particular needs and opportunities for health information technology applications in cardio-oncology;
-
•
Advocate for equitable distribution and enhancement of technology resources at the federal, state, and local governmental level so that health information exchanges, such as EHRs, are more uniform and better suited for population health strategies and initiatives.
10.2.3. Education speed panel
The Education speed panel was moderated by Dr. Kathryn J Ruddy, who was a member of the ASCO Cancer Survivorship Committee, member of the NCCN Survivorship Guidelines Committee, and a Professor of Oncology and Director of Cancer Survivorship for the Department of Oncology at Mayo Clinic Rochester. Dr. Martha Gulati, who was the chief of cardiology at the University of Arizona and President-Elect of the ASPC, was our academic panelist, and Dan Zavorotny, who is the Founder and Chief Operating Officer for NutriSense, was the industry/company panelist.
The Education speed panel discussed determining optimal modes for knowledge exchange, with salient suggestions as follows:
-
•
Use social media formats such as Twitter to facilitate up-to-date knowledge exchange of information among providers such as sharing guidelines and new research via community chats and journal clubs with CME, while ensuring there are alternative options for those who do not or cannot access digital platforms (to avoid a “digital divide”);
-
•
Employ graphics and pictographs in patient education and risk discussions to more meaningfully communicate customized risk and care plans in culturally sensitive conversations;
-
•
Ensure educational content that features patient images mirroring the ethnic backgrounds of the target populations on digital video or online platforms, as well as print;
-
•
Train allied health staff such as health coaches and dieticians who are less constrained than physician level providers and can spend the needed time to educate patients and provide tools such as iPads at the point of care for patient education and coaching;
-
•
Assess health literacy and then use appropriate chat functions to allow asynchronous communication with the appropriate level health staff for continued guidance outside of the office visit;
-
•
Encourage patient accountability by deploying features within mobile apps such as push notifications and nudges as prompts for sustained behavior modification;
-
•
Use podcasts to disseminate new information via brief interviews and quick sound bites targeted to either the patient or health care professional.
11. Humanism in the cardiology oncology innovation network
Summit attendees are given an attendee booklet featuring an agenda, abstracts, featured guests and speakers, space for note-taking and reflection, and more. In addition, an engagement break takes place during the summit to allow participants to connect using the chat feature while music plays and a virtual exhibit is displayed on the screen. This time is also an opportunity for participants to step away so that they are refreshed and ready to engage during the following segment. In the chat, a range of individuals introduce themselves and include fun details to help us connect, such as over our favorite flavors of ice cream: seven layer bar flavor from Jeni's Ice Cream, Chocolate Shoppe's Iced Latte-Da, Vanilla, Blue Bell Homemade Vanilla, Kikapoo – Vanilla, Jeni's Brown Butter Almond Brittle, Strawberry, Green Tea Flavor, Mint Ice Cream, Various Types of Chocolate with Espresso, Chocolate Peanut Butter, Dark Chocolate anything, Chocolate Chip Mint all the way; and does Ben and Jerry's count?
The physicians and scientists taking part in the summit also have myriad artistic talents. For example, each annual COIN Summit includes live poetry recital at the beginning or conclusion of the summit to ground our work in the context of humanism and caring for our patients. To highlight this, an excerpt from a poem Dr. Sherry-Ann Brown authored and published in Oncology Times entitled, “Protecting A Woman's Heart” is included. This poem was incorporated into presentations at Mayo Clinic resulting in Mayo Media Services capturing the writer's vision in an accompanying video.
The Heart Cries
Oh, my love.
When you see the hurt in me,
It is because I reach out
And wrap myself around you,
To protect you.
I cannot myself take the cancer from you.
But I can wrap myself around you
To hold and comfort you.
And shield you from the damage
Of radiation and chemotherapy.
I know the rays and potions
Are meant to cure you,
But I know they can also hurt
The healthy parts of you.
If you hurt, I hurt.
If you heal, I heal.
I don't want you to hurt alone.
It is my honor to hurt with you.
It is my honor to hurt for you.
The Breast Responds
No, my love,
Do not hurt for me.
Do not hurt with me.
…
If I cannot protect you,
Let me introduce you
To someone who will.
The Heart Responds
Yes, my love,
Introduce me.
Let me meet
Our cardio-oncologist.
Show me the way
To our preventive cardiologist.
Show me a most excellent way
To protect a woman’s heart.
The poem is included in a recently published book along with several other poems related to the heart and cancer. To improve patient access to humanistic works such as this, Dr. Brown includes a link to the poem on her patient-facing physician webpage at Froedtert and the Medical College of Wisconsin as a signature poem. Patients have described reading the poem before coming to see Dr. Brown in clinic. Dr. Brown hopes to make this book available for patients as an E-book or in physical form at no cost. The poetry E-book on the COIN website was made available free to all COIN members for five days following the summit to share the poetry and sentiments with their patients or to personally reflect upon the contents and their own creativity.
Overall, participants felt the summit was “uplifting” – “a collaborative conference of hope and healing!”
12. Summit outcomes
Initial outcomes from COIN over the past few years were previously published [8]. Many Summit registrants are involved in existing institutional innovation projects (Fig. 7). In addition, the creation of a cardio-oncology app as a tool to use for cardio-oncology guidelines and drug interactions was discussed at the COIN Summits. Such an app will act as a practical reference and facilitate the point of care application of evidence-based medicine. This COIN app or mobile site will have the potential to normalize screening and risk stratification tools in clinical practice and improve access to evidence-based medicine. The app may be somewhat similar to the guidelines apps accessible on the go from each cardiology society: ACC Guidelines App, AHA Guidelines App, and ESC Guidelines App, and will consolidate cardio-oncology recommendations from all three among other society statements (Fig. 8). An initial COIN webpage aggregating these cardio-oncology guidelines is now available to network members and all parties interested in joining the network.
Fig. 7.
Topics of Existing Institutional Innovation Projects of the First 50 Summit Registrants at the inaugural Cardiology Oncology Innovation Network Summit in 2020. Horizontal axis = number of participants; EHR = electronic health record, CV = cardiovascular, COIN = Cardiology Oncology Innovation Network, ICU = Intensive Care Unit, ECG = electrocardiogram, PSC = pleuripotent stem cell, CAR-T = chimeric antigen receptor T-cell, ML = machine learning, CDS = clinician decision support, MRI = magnetic ressonance imaging, CHIP = clonal hematopoiesis of indeterminate potential, CVD = cardiovascular disease, FU = fluorouracil, CHIRP = Connected Health Innovation Research Project and CGM = continuous glucose monitoring.
Fig. 8.
American and European cardiology society guidelines mobile applications. The American College of Cardiology (ACC), American Heart Association (AHA), and European Society for Cardiology (ESC) all provide apps for both iOS and Android platforms to host guidelines, scientific statements, and expert recommendations docuuments produced by each society, and the ideal state will be rapid inclusion of all cardio-oncology guidelines, scientific statements, and expert recommendations.
Additional support for the growth of the field of cardio-oncology has come from the AHA releasing scientific statements, and the development of educational structure. Many members of COIN are part of these writing groups and their reviewers advancing training, guidelines, and certification in the field [50,[55], [56], [57], [58], [59], [60]]. These scientific statements have spanned topics from cardiovascular biomarker utilization in cancer survivors, vascular and metabolic considerations in cardio-oncology, preclinical models, cardio-oncology rehabilitation, managing cardiovascular outcomes in cancer patients and survivors, prevention and management of arrhythmias and autonomic disorders in cardio-oncology, and more. These scientific statements can provide guidance for cardio-oncology clinical care, research, and education. Additional publications to advance the education of cardio-oncology trainees involve the new training guidelines from ACC and ICOS [30,[46], [47], [48]]. In addition, ICOS has also developed a certification exam for Cardio-Oncology. Cardio-oncology training and guidelines will continue to iterate and innovate and incorporate future data that address knowledge gaps such as the utility of cardio-oncology rehabilitation and telehealth [61], among other emerging topics.
13. Coin Summit 2022 update
The 2022 Summit was held virtually in December 2022. Session I began with an introduction by the network founder Dr. Sherry-Ann Brown. Then a patient advocate Ms. Monique McGahee described ways to maximize quality of life and the importance of empathetic and holistic care for cancer patients. This was followed by a panel discussion on innovation, collaboration, and education featuring panelists and moderator: Dr. Charles Thomas (Past Chair, Membership Committee, American Society of Clinical Oncology), Dr. Ana Barac (Founding Chair, Cardio-Oncology Section, American College of Cardiology), Dr. Travis Batts (Cardiologist, United States Air Force), Dr. Andrew Miller (Board of Trustees, American College of Cardiology) and Dr. Andriana Nikolova (CEO, Yosko Incorporated). This panel discussion built on themes of the previous years' summits suggesting ways to further expand the reach of COIN and ways to best serve cardio-oncology patients through various forms of innovation.
In Session II, Dr. Sandra Lewis (Founder of Sandra J. Lewis Cardiovascular Women's Leadership Institute, American College of Cardiology) moderated four rapid abstract presentations by cardio-oncology trainees. The abstracts covered four key topics: digital health, big data, health disparities and AI. Session III focused on COIN partnerships through network updates and discussions in breakout rooms followed by gathering in the main room to report on all the breakout room discussions. The innovation breakout room was led by Dr. Hugo Martinez and Dr. Joshua Levenson, focusing on leveraging innovations in bidirectional cardio-oncology. The collaboration breakout room was led by Dr. Diego Sadler and Dr. Anne Blaes who focused on identifying the key stakeholders in bidirectional cardio-oncology. The education breakout room was led by Ragasnehith Maddula and Jean Bikomeye (at that time an MD and PhD student, respectively) focusing on determining who needs education and how it should be delivered in the context of bidirectional cardio-oncology. Finally, closing remarks were accompanied by poetry and a virtual exhibit.
14. Coin Summit 2023 update
The 2023 Summit was held virtually in December 2023. Session I began with an introduction by the network founder Dr. Sherry-Ann Brown. Then patient advocate Ms. Gabby Mgabwu spoke about her experiences with patients while shadowing cardiologists in a cancer center, and the impact of recording her patient interactions in a journal through writing and drawing. The majority of Session I then consisted of an open forum discussion moderated by Dr. Brenton Bauer, exploring the breadth of topics to be included in the upcoming textbook titled “Innovation in Cardio-Oncology: Artificial Intelligence, Digital Health, Precision Medicine” with Editor and several authors from across COIN.
In Session II, two faculty experts presented on Advancing Cardio-oncology: Artificial Intelligence, Remote Physiologic Monitoring and Partnerships (Dr. John L. Jefferies) and Updates on Global Cardio-Oncology Registry (G-COR): From Pilot to Global (Dr. Diego Sadler). The final session focused on COIN collaborations and charting the course for the future, moderated by Dr. Courtney Campbell. The summit was closed with a review of the current state of COIN and future various initiatives, along with poetry as usual.
15. Discussion
The continuous expansion in the repertoire of cancer modalities has introduced the advent of premature cardiovascular adversities and long-term sequelae. Although our understanding of the biological components of cancer therapy-related cardiovascular dysfunction has improved, regulatory policies for drug administration have been established, and guideline recommendations have been generated for the management of this patient population, there remain gaps in the identification and application of beneficial technologies in cardio-oncology patients. For some survivors of cancer, the risk of cardiovascular death exceeds the risk of death from cancer, suggesting that cardio-oncology may become an important component for long-term health and well-being in cancer survivors. To this end, COIN has been inaugurated and has so far hosted two annual summits.
In this proceedings report, we have described crucial elements from the 2020 and 2021 annual COIN summits. During the two summits, knowledge was shared in the areas of innovation, education, and collaboration in breakout rooms, speed panels, and large group network-wide discussions. Topics included patient-centered solutions such as the global cardio-oncology registry, digital health platforms, social media activity including the @CardioOnc_Bot, and opportunities for standardization and efficiency including dot phrase templates, and these topic discussions complimented patient stories and trainee abstracts also presented. Participants shared their areas of current research or work to connect and find points of potential collaboration. Some of these interests focused on innovative community and neighborhood interventions to reduce the risk for major adverse cardiovascular events among women diagnosed with breast cancer who received anthracyclines or antibody therapies. Discussions also involved the potential use of blockchain, preclinical ultrasound imaging, cardiovascular biomechanics, molecular imaging, advanced cardiovascular imaging, and imaging biomarkers for early detection and characterization of cancer treatment-induced subclinical cardiac dysfunction and cardiotoxicity in adults and children. The contributions of researchers, clinicians, industry specialists, and learners in COIN highlighted at the Annual COIN Summit are a very important step in addressing the needs of the growing population of cancer survivors. By investigating and disseminating information on innovations, COIN furthers the field of cardio-oncology for cancer patients.
Key elements from the 2020 and 2021 annual summits regarding the dissemination of knowledge and discovery gained through the integration of digital medicine technologies and innovations into clinical practice, research, and health profession education have been presented, and support our previous publication on the launch of the network [8]. Recommendations were offered from attendees to direct health organization administrators and physician leaders towards valuing innovations such as the use of artificial intelligence algorithms, predictive analytics, and other cardio-oncology initiatives with “urgency”, recognizing that “a collective voice from organizations like COIN will have the greatest impact” for all cancer survivors, and especially to advance health equity for racial and ethnic minorities. As more exploration in the evolving realms of medical technology and system implementation is needed, ongoing projects will continue to be pursued and new endeavors undertaken at future annual COIN Summits and year-round through teamwork by COIN constituents, with particular emphasis on addressing (and not propagating) health disparities in cardio-oncology. The work of the network has become increasingly important, as health informatics is essential for deriving important guidelines from the vast amount of data collected by new devices and bringing them to the forefront of clinical medicine, research, and education. In our current and future technology-driven modern medical and scientific landscape, achieving COIN's goals will continue to require the collaboration of a diverse group of stakeholders, including leaders in medicine, informatics, education, and industry, among others; the international cooperation between institutions and individuals within COIN enables a synergistic effort greater than the sum of its parts.
All are welcome to join us at the COIN Summit in mid-December each year.
Detailed outcomes of the 2022, 2023, and 2024 (December 14th) Summits will be included in a subsequent manuscript reviewing accomplishments from five years in COIN.
Funding
This work was supported by the St. Jude Pediatric Research Recruitment Support Fund hosted by H.R.M. (R079700270). This publication was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Numbers UL1TR001436 and KL2TR001438. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Disclosures
Several industry and pharmaceutical companies sponsored the inaugural COIN Summit in 2020 and Frontiers in Cardiovascular Medicine sponsored the second COIN Summit in 2021. Our sponsors did not exert any restrictions on our work or publications. Additionally, our Summit panelists include industry representatives whose helpful comments are included in this manuscript; these industry panelists are therefore acknowledged in this manuscript. These industry organizations have had no input in the drafting or contents of the manuscript beyond the relevant comments made by industry panelists during the Summit.
CRediT authorship contribution statement
Sherry-Ann Brown: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. Craig Beavers: Conceptualization, Investigation, Supervision, Writing – original draft, Writing – review & editing. Brenton Bauer: Conceptualization, Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing. Richard K. Cheng: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft. Generika Berman: Investigation, Methodology, Writing – original draft, Writing – review & editing. Catherine H. Marshall: Conceptualization, Formal analysis, Validation, Writing – original draft, Writing – review & editing. Avirup Guha: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. Prantesh Jain: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. Austin Steward: Investigation, Methodology, Writing – original draft, Writing – review & editing. Jeanne M. DeCara: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. Iredia M. Olaye: Methodology, Writing – original draft, Writing – review & editing. Kathryn Hansen: Investigation, Writing – original draft, Writing – review & editing. Jim Logan: Investigation, Methodology, Writing – review & editing. Carmen Bergom: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. Carri Glide-Hurst: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Irving Loh: Conceptualization, Investigation, Supervision, Writing – original draft, Writing – review & editing. John Alan Gambril: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. James MacLeod: Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. Ragasnehith Maddula: Investigation, Methodology, Writing – original draft, Writing – review & editing. Peter J. McGranaghan: Writing – original draft, Writing – review & editing. Akshee Batra: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Courtney Campbell: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. Abdulaziz Hamid: Investigation, Methodology, Writing – original draft, Writing – review & editing. Fatma Gunturkun: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing. Robert Davis: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. John Jefferies: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Michael Fradley: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. Katherine Albert: Writing – original draft, Writing – review & editing. Anne Blaes: Conceptualization, Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing. Indrajit Choudhuri: Conceptualization, Investigation, Supervision, Writing – original draft, Writing – review & editing. Arjun K. Ghosh: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Thomas D. Ryan: Conceptualization, Investigation, Supervision, Writing – original draft, Writing – review & editing. Ogochukwu Ezeoke: Investigation, Methodology, Writing – original draft, Writing – review & editing. Douglas J. Leedy: Investigation, Supervision, Writing – original draft, Writing – review & editing. Wadsworth Williams: Investigation, Visualization, Writing – original draft, Writing – review & editing. Sebastian Roman: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Lorenz Lehmann: Investigation, Writing – original draft, Writing – review & editing. Abdullah Sarkar: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Diego Sadler: Conceptualization, Funding acquisition, Resources, Supervision, Writing – original draft, Writing – review & editing. Elizabeth Polter: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Kathryn J. Ruddy: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Neha Bansal: Investigation, Writing – original draft, Writing – review & editing. Eric Yang: Conceptualization, Investigation, Supervision, Writing – original draft, Writing – review & editing. Brijesh Patel: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. David Cho: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Alison Bailey: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. Daniel Addison: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. Vijay Rao: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. Joshua E. Levenson: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Dipti Itchhaporia: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Karol Watson: Formal analysis, Supervision, Writing – original draft, Writing – review & editing. Martha Gulati: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Kim Williams: Investigation, Supervision, Writing – review & editing. Donald Lloyd-Jones: Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. Erin Michos: Supervision, Writing – original draft, Writing – review & editing. Julie Gralow: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Hugo Martinez: Conceptualization, Funding acquisition, Project administration, Resources, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We are grateful to all members of the Connected Health Innovation Research Program (C.H.I.R.P.), Cardiology Oncology Innovation Network (COIN), and Cardio-Oncology Artificial Intelligence Informatics & Precision (CAIP) Research Team Investigators for local, regional, national and global partnership in this work.
References
- 1.Biasillo G., Cipolla C.M., Cardinale D. Cardio-oncology: gaps in knowledge, goals, advances, and educational efforts. Curr. Oncol. Rep. 2017;19(8):55. doi: 10.1007/s11912-017-0610-9. [DOI] [PubMed] [Google Scholar]
- 2.Bluethmann S.M., Mariotto A.B., Rowland J.H. Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol. Biomarkers Prev. 2016;25(7):1029–1036. doi: 10.1158/1055-9965.EPI-16-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foraker R.E., Benziger C.P., DeBarmore B.M., Cené C.W., Loustalot F., Khan Y., et al. Achieving optimal population cardiovascular health requires an interdisciplinary team and a learning healthcare system: a scientific statement from the American Heart Association. Circulation. 2021;143(2):e9–e18. doi: 10.1161/CIR.0000000000000913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peake J.M., Kerr G., Sullivan J.P. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front. Physiol. 2018;9:743. doi: 10.3389/fphys.2018.00743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maddox T.M., Albert N.M., Borden W.B., Curtis L.H., Ferguson T.B., Kao D.P., et al. The learning healthcare system and cardiovascular care: a scientific statement from the American Heart Association. Circulation. 2017;135(14) doi: 10.1161/CIR.0000000000000480. e826-e57. [DOI] [PubMed] [Google Scholar]
- 6.Ho P.M., Magid D.J., Shetterly S.M., Olson K.L., Peterson P.N., Masoudi F.A., et al. Importance of therapy intensification and medication nonadherence for blood pressure control in patients with coronary disease. Arch. Intern. Med. 2008;168(3):271–276. doi: 10.1001/archinternmed.2007.72. [DOI] [PubMed] [Google Scholar]
- 7.Masoudi F.A., Go A.S., Magid D.J., Cassidy-Bushrow A.E., Doris J.M., Fiocchi F., et al. Longitudinal study of implantable cardioverter-defibrillators: methods and clinical characteristics of patients receiving implantable cardioverter-defibrillators for primary prevention in contemporary practice. Circ. Cardiovasc. Qual. Outcomes. 2012;5(6):e78–e85. doi: 10.1161/CIRCOUTCOMES.112.965368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown S.A., Beavers C., Martinez H.R., Marshall C.H., Olaye I.M., Guha A., et al. Bridging the gap to advance the care of individuals with cancer: collaboration and partnership in the Cardiology Oncology Innovation Network (COIN) Cardiooncology. 2022;8(1):2. doi: 10.1186/s40959-022-00129-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ray-Coquard I., Philip T., de Laroche G., Froger X., Suchaud J.P., Voloch A., et al. A controlled “before-after” study: impact of a clinical guidelines programme and regional cancer network organization on medical practice. Br. J. Cancer. 2002;86(3):313–321. doi: 10.1038/sj.bjc.6600057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhavnani S.P., Parakh K., Atreja A., Druz R., Graham G.N., Hayek S.S., et al. 2017 roadmap for innovation-ACC health policy statement on healthcare transformation in the era of digital health, big data, and precision health: a report of the American College of Cardiology Task Force on health policy statements and Systems of Care. J. Am. Coll. Cardiol. 2017;70(21):2696–2718. doi: 10.1016/j.jacc.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 11.Guha A., Desai N.R., Weintraub N.L. Assessing cardiovascular risk in cancer patients: opportunities and challenges. Eur. J. Prev. Cardiol. 2021;28(9) doi: 10.1177/2047487320943002. e45-e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahmood S.S., Fradley M.G., Cohen J.V., Nohria A., Reynolds K.L., Heinzerling L.M., et al. Myocarditis in patients treated with immune checkpoint inhibitors. J. Am. Coll. Cardiol. 2018;71(16):1755–1764. doi: 10.1016/j.jacc.2018.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alvi R.M., Frigault M.J., Fradley M.G., Jain M.D., Mahmood S.S., Awadalla M., et al. Cardiovascular events among adults treated with chimeric antigen receptor T-cells (CAR-T) J. Am. Coll. Cardiol. 2019;74(25):3099–3108. doi: 10.1016/j.jacc.2019.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadler D., Fradley M.G., Ismail-Khan R., Raez L., Bhandare D., Elson L., et al. Florida inter-specialty collaborative project to improve cardio-oncology awareness and identify existing knowledge gaps. JACC CardioOncol. 2020;2(3):535–538. doi: 10.1016/j.jaccao.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sadler D., Arnold A., Herrmann J., Daniele A., Silva C.M.P.D., Ghosh A.K., et al. Reaching across the aisle: cardio-oncology advocacy and program building. Curr. Oncol. Rep. 2021;23(6):64. doi: 10.1007/s11912-021-01059-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NWBiospecimen: University of Washington; [Available from: https://depts.washington.edu/nwbios/.
- 17.UCLA ATLAS Community Health Initiative UCLA Health [Available from: https://www.uclahealth.org/precision-health/atlas.
- 18.Bonsu J.M., Guha A., Charles L., Yildiz V.O., Wei L., Baker B., et al. Reporting of cardiovascular events in clinical trials supporting FDA approval of contemporary cancer therapies. J. Am. Coll. Cardiol. 2020;75(6):620–628. doi: 10.1016/j.jacc.2019.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oren O., Neilan T.G., Fradley M.G., Bhatt D.L. Cardiovascular safety assessment in cancer drug development. J. Am. Heart Assoc. 2021;10(24) doi: 10.1161/JAHA.121.024033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrmann J., Lenihan D., Armenian S., Barac A., Blaes A., Cardinale D., et al. Defining cardiovascular toxicities of cancer therapies: an International Cardio-Oncology Society (IC-OS) consensus statement. Eur. Heart J. 2022;43(4):280–299. doi: 10.1093/eurheartj/ehab674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martinez H.R., Beasley G.S., Goldberg J.F., Absi M., Ryan K.A., Guerrier K., et al. Pediatric cardio-oncology medicine: a new approach in cardiovascular care. Children (Basel) 2021;8(12) doi: 10.3390/children8121200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Y., Chow E.J., Oeffinger K.C., Border W.L., Leisenring W.M., Meacham L.R., et al. Traditional cardiovascular risk factors and individual prediction of cardiovascular events in childhood cancer survivors. J. Natl. Cancer Inst. 2020;112(3) doi: 10.1093/jnci/djz108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chow E.J., Chen Y., Hudson M.M., Feijen E.A.M., Kremer L.C., Border W.L., et al. Prediction of ischemic heart disease and stroke in survivors of childhood cancer. J. Clin. Oncol. 2018;36(1):44–52. doi: 10.1200/JCO.2017.74.8673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St. Jude Children's Research Hospital. CCSS Cardiovascular Risk Calculator: St. Jude Children's Research Hospital; [Available from: https://ccss.stjude.org/tools-and-documents/calculators-and-other-tools/ccss-cardiovascular-risk-calculator.html.
- 25.Abdel-Qadir H., Thavendiranathan P., Austin P.C., Lee D.S., Amir E., Tu J.V., et al. Development and validation of a multivariable prediction model for major adverse cardiovascular events after early stage breast cancer: a population-based cohort study. Eur. Heart J. 2019;40(48):3913–3920. doi: 10.1093/eurheartj/ehz460. [DOI] [PubMed] [Google Scholar]
- 26.Ezaz G., Long J.B., Gross C.P., Chen J. Risk prediction model for heart failure and cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J. Am. Heart Assoc. 2014;3(1) doi: 10.1161/JAHA.113.000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dranitsaris G., Rayson D., Vincent M., Chang J., Gelmon K., Sandor D., et al. The development of a predictive model to estimate cardiotoxic risk for patients with metastatic breast cancer receiving anthracyclines. Breast Cancer Res. Treat. 2008;107(3):443–450. doi: 10.1007/s10549-007-9803-5. [DOI] [PubMed] [Google Scholar]
- 28.Herrmann J., Lerman A., Sandhu N.P., Villarraga H.R., Mulvagh S.L., Kohli M. Evaluation and management of patients with heart disease and cancer: cardio-oncology. Mayo Clin. Proc. 2014;89(9):1287–1306. doi: 10.1016/j.mayocp.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown S.A. Preventive cardio-oncology: the time has come. Front. Cardiovasc. Med. 2019;6:187. doi: 10.3389/fcvm.2019.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown S.A., Sandhu N. Proposing and meeting the need for interdisciplinary cardio-oncology subspecialty training. J. Card. Fail. 2016;22(11):934–935. doi: 10.1016/j.cardfail.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 31.Haddad T., Helgeson J.M., Pomerleau K.E., Preininger A.M., Roebuck M.C., Dankwa-Mullan I., et al. Accuracy of an artificial intelligence system for Cancer clinical trial eligibility screening: retrospective pilot study. JMIR Med. Inform. 2021;9(3) doi: 10.2196/27767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown S.A. 2022. Cardiology Oncology Innovation Network Annual Summit Abstract Book 2020/2021. [Google Scholar]
- 33.Güntürkün F., Akbilgic O., Davis R.L., Armstrong G.T., Howell R.M., Jefferies J.L., et al. Artificial intelligence-assisted prediction of late-onset cardiomyopathy among childhood cancer survivors. JCO Clin. Cancer Inform. 2021;5:459–468. doi: 10.1200/CCI.20.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saxena A., Rubens M., Ramamoorthy V., Das S., Bhatt C.B., Salami J.A., et al. Abstract P338: cardiovascular and cerebrovascular events associated with cancer surgery in the United States. Circulation. 2020;141(Suppl_1):AP338-AP [Google Scholar]
- 35.Campbell C., Mbeng C., Rodgers B., Bumma N., Efebera Y., Sharma N., et al. American College of Cardiology; Advancing the Cardiovascular Care of the Oncology Patient: 2020. Delays in Diagnosis of Transthyretin Cardiac Amyloidosis after Establishing Cardiac Care. [Google Scholar]
- 36.Guha A., Addison D., Jain P., Gutierrez J.M., Ghosh A., Roddie C., et al. Cardiovascular events associated with chimeric antigen receptor T cell therapy: cross-sectional FDA adverse events reporting system analysis. Biol. Blood Marrow Transplant. 2020;26(12):2211–2216. doi: 10.1016/j.bbmt.2020.08.036. [DOI] [PubMed] [Google Scholar]
- 37.Zhou Y., Hou Y., Hussain M., Brown S.A., Budd T., Tang W.H.W., et al. Machine learning-based risk assessment for cancer therapy-related cardiac dysfunction in 4300 longitudinal oncology patients. J. Am. Heart Assoc. 2020;9(23) doi: 10.1161/JAHA.120.019628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maddula R., MacLeod J., Painter S., McLeish T., Steward A., Rossman A., et al. Connected Health Innovation Research Program (C.H.I.R.P.): a bridge for digital health and wellness in cardiology and oncology. Am. Heart J. Plus: Cardiol. Res. Pract. 2022;20 doi: 10.1016/j.ahjo.2022.100192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Finke D., Romann S.W., Heckmann M.B., Hund H., Bougatf N., Kantharajah A., et al. High-sensitivity cardiac troponin T determines all-cause mortality in cancer patients: a single-centre cohort study. ESC Heart Fail. 2021;8(5):3709–3719. doi: 10.1002/ehf2.13515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sadler D.B., Moudgil R., Arco T., Collier P.H., Sarkar A., Barac A., et al. Global cardio oncology registry: structure for a multinational collaboration. Circulation. 2021;144(Suppl_1):A11675-A [Google Scholar]
- 41.Heintzelman H. Tempus accelerates its EHR integration scope with epic: business. https://www.businesswire.com/news/home/20211118005951/en/Tempus-Accelerates-Its-EHR-Integration-Scope-With-Epic Business Wire. November 18, 2021. Accessed January 20, 2023.
- 42.Stan D.L., Inselman J.W., Ridgeway J.L., Johnson K.N., Christopherson L.A., McColley S.M., et al. Pilot implementation to assess the feasibility and care team impact of an app-based interactive care plan to remotely monitor breast cancer survivors. J. Cancer Surviv. 2022;16(1):13–23. doi: 10.1007/s11764-021-01136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pritchett J.C., Borah B.J., Desai A.P., Xie Z., Saliba A.N., Leventakos K., et al. Association of a remote patient monitoring (RPM) program with reduced hospitalizations in cancer patients with COVID-19. JCO Oncol. Pract. 2021;17(9) doi: 10.1200/OP.21.00307. e1293-e302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coffey J.D., Christopherson L.A., Glasgow A.E., Pearson K.K., Brown J.K., Gathje S.R., et al. Implementation of a multisite, interdisciplinary remote patient monitoring program for ambulatory management of patients with COVID-19. NPJ Digit Med. 2021;4(1):123. doi: 10.1038/s41746-021-00490-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sanchez E. Life’s simple 7: vital but not easy. J. Am. Heart Assoc. 2018;7(11) doi: 10.1161/JAHA.118.009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alvarez-Cardona J.A., Ray J., Carver J., Zaha V., Cheng R., Yang E., et al. Cardio-oncology education and training: JACC council perspectives. J. Am. Coll. Cardiol. 2020;76(19):2267–2281. doi: 10.1016/j.jacc.2020.08.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lenihan D.J., Hartlage G., DeCara J., Blaes A., Finet J.E., Lyon A.R., et al. Cardio-oncology training: a proposal from the international CardiOncology society and Canadian cardiac oncology network for a new multidisciplinary specialty. J. Card. Fail. 2016;22(6):465–471. doi: 10.1016/j.cardfail.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 48.Tuzovic M., Brown S., Yang E., West B., Bassi N., Park S., et al. Implementation of cardio-oncology training for cardiology fellows. JACC: CardioOncol. 2020;2(5):795–799. doi: 10.1016/j.jaccao.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barac A., Murtagh G., Carver J.R., Chen M.H., Freeman A.M., Herrmann J., et al. Cardiovascular health of patients with cancer and cancer survivors: a roadmap to the next level. J. Am. Coll. Cardiol. 2015;65(25):2739–2746. doi: 10.1016/j.jacc.2015.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Campia U., Moslehi J.J., Amiri-Kordestani L., Barac A., Beckman J.A., Chism D.D., et al. Cardio-oncology: vascular and metabolic perspectives: a scientific statement from the American Heart Association. Circulation. 2019;139(13):e579–e602. doi: 10.1161/CIR.0000000000000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Curigliano G., Lenihan D., Fradley M., Ganatra S., Barac A., Blaes A., et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann. Oncol. 2020;31(2):171–190. doi: 10.1016/j.annonc.2019.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Iliescu C., Grines C.L., Herrmann J., Yang E.H., Cilingiroglu M., Charitakis K., et al. SCAI expert consensus statement: evaluation, management, and special considerations of cardio-oncology patients in the cardiac catheterization laboratory (endorsed by the Cardiological Society of India, and Sociedad Latino Americana de Cardiologıa Intervencionista) Catheter. Cardiovasc. Interv. 2016;87(5):895–899. doi: 10.1002/ccd.26375. [DOI] [PubMed] [Google Scholar]
- 53.Armenian S.H., Lacchetti C., Barac A., Carver J., Constine L.S., Denduluri N., et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. 2017;35(8):893–911. doi: 10.1200/JCO.2016.70.5400. [DOI] [PubMed] [Google Scholar]
- 54.Brown S.A., Rhee J.W., Guha A., Rao V.U. Innovation in precision cardio-oncology during the coronavirus pandemic and into a post-pandemic world. Front. Cardiovasc. Med. 2020;7:145. doi: 10.3389/fcvm.2020.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Asnani A., Moslehi J.J., Adhikari B.B., Baik A.H., Beyer A.M., de Boer R.A., et al. Preclinical models of cancer therapy-associated cardiovascular toxicity: a scientific statement from the American Heart Association. Circ. Res. 2021;129(1):e21–e34. doi: 10.1161/RES.0000000000000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chow S.L., Maisel A.S., Anand I., Bozkurt B., de Boer R.A., Felker G.M., et al. Role of biomarkers for the prevention, assessment, and management of heart failure: a scientific statement from the American Heart Association. Circulation. 2017;135(22) doi: 10.1161/CIR.0000000000000490. e1054-e91. [DOI] [PubMed] [Google Scholar]
- 57.Fradley M.G., Beckie T.M., Brown S.A., Cheng R.K., Dent S.F., Nohria A., et al. Recognition, prevention, and management of arrhythmias and autonomic disorders in cardio-oncology: a scientific statement from the American Heart Association. Circulation. 2021;144(3):e41–e55. doi: 10.1161/CIR.0000000000000986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gilchrist S.C., Barac A., Ades P.A., Alfano C.M., Franklin B.A., Jones L.W., et al. Cardio-oncology rehabilitation to manage cardiovascular outcomes in cancer patients and survivors: a scientific statement from the American Heart Association. Circulation. 2019;139(21):e997–e1012. doi: 10.1161/CIR.0000000000000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zaha V.G., Hayek S.S., Alexander K.M., Beckie T.M., Hundley W.G., Kondapalli L., et al. Future perspectives of cardiovascular biomarker utilization in cancer survivors: a scientific statement from the American Heart Association. Circulation. 2021;144(25) doi: 10.1161/CIR.0000000000001032. e551-e63. [DOI] [PubMed] [Google Scholar]
- 60.Lyon A.R., López-Fernández T., Couch L.S., Asteggiano R., Aznar M.C., Bergler-Klein J., et al. ESC guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS) Eur. Heart J. 2022;43(41):4229–4361. doi: 10.1093/eurheartj/ehac244. (2022) [DOI] [PubMed] [Google Scholar]
- 61.Batalik L., Filakova K., Radkovcova I., Dosbaba F., Winnige P., Vlazna D., et al. Cardio-oncology rehabilitation and telehealth: rationale for future integration in supportive care of cancer survivors. Front. Cardiovasc. Med. 2022;9 doi: 10.3389/fcvm.2022.858334. [DOI] [PMC free article] [PubMed] [Google Scholar]