Abstract
Objective
Acute severe behavioural disturbance (ASBD) is a condition seen with increasing frequency in EDs. It poses a significant risk to the patient and those around them. Little is known about the epidemiology or most effective management in the paediatric population. The aim of the present study is to clarify the practice of senior emergency doctors in Australia when managing paediatric ASBD.
Methods
The present study was a voluntary electronic questionnaire distributed to and undertaken by senior medical staff in EDs affiliated with the Paediatric Research in Emergency Departments International Collaborative (PREDICT) network. Respondents reported on exposure to and confidence in managing paediatric ASBD and their current practices.
Results
A total of 227 (33%) clinicians completed the survey between February and May 2020. Most clinicians were caring for at least two young people with ASBD each week (72%), felt confident regarding the majority of components of management and referred to local clinical practice guidelines (69%). Agitation/sedation rating scales were seldom used (19%). There was a significant variation in self‐reported management practices. The choice of whether to use medication at all, the medication chosen and route of administration all varied greatly. Respondents were more willing to provide parenteral medication to young people reported as having recreational drug intoxication (84%) than those with neurodevelopment disorders (65%) when the same degree of agitation was reported.
Conclusions
Within Australia, there is considerable variation in paediatric ASBD practice, in particular regarding medication provision. Further prospective research is required to inform best clinical practice.
Keywords: child psychiatry, hypnotic and sedative, paediatric emergency medicine, psychomotor agitation
Paediatric acute severe behavioural disturbance is a common ED presentation. Within Australia, there is considerable variation in paediatric acute severe behavioural disturbance practice, in particular relating to medication provision. Further prospective research is required to inform best clinical practice.

Key findings.
Paediatric ASBD is a common ED presentation.
There is significant variation in practice for the management of these young people.
Further research is warranted to determine the most effective oral and parenteral medications for the safe management of paediatric ASBD in the ED setting.
Introduction
Acute severe behavioural disturbance (ASBD) is a common ED presentation. It poses considerable physical and psychological risk to the patient, their family and ED staff. 1 , 2 The epidemiology and most effective management options are well elucidated in the adult population; 3 , 4 , 5 , 6 , 7 , 8 however, this information is lacking for children and adolescents.
The contributing factors for paediatric ASBD differ from those seen in adults. In adults, acute drug intoxication is common. 9 In the paediatric population, mental health disorders predominate. 10 , 11 Young people with underlying neurodevelopmental disorders such as autism spectrum disorder (ASD) are over‐represented. 12 There is also a strong female preponderance, whereas in adult ASBD the majority are male. 10 , 11 , 13
A step‐wise approach is endorsed for the management of these young people. Verbal de‐escalation is attempted first. 14 If this fails to achieve behavioural containment, oral and parenteral medications are then used. Many institutions have a clinical practice guideline (CPG) which includes an approach to the management of paediatric ASBD. 14 , 15 , 16 , 17 However, the medications and doses suggested vary considerably between CPGs across Australia. This is likely because of the lack of specific literature examining the most effective management options, including medications, in this population. 18
Before further prospective research can be undertaken to determine the most effective management strategies for these young people, it is essential to understand what constitutes current management. This will provide baseline information to allow for targeted prospective research.
Methods
Participants and design
Between February and May 2020, a previously piloted electronic survey was undertaken by fellows and consultants in EDs across PREDICT (Paediatric Research in Emergency Departments International Collaborative) network‐affiliated departments within Australia.
An invitation to participate was sent to the nominated research lead at EDs across the PREDICT network. Thirty‐two EDs were invited to participate with 28 accepting the invitation. Each research lead completed a site survey (Appendix S1) which contained questions relating to specific hospital staffing, procedures and processes. The research lead then distributed an email invitation to all eligible staff at their site inviting them to participate in an anonymous clinician survey (Appendix S2). A follow‐up email encouraging all eligible staff to complete the survey was sent by each nominated research lead four weeks after the initial email.
Eligible staff in this survey were defined as consultants and fellows. Fellows were identified as those doctors working in a nominated fellow position within their department.
The clinician survey posed a range of multiple‐choice questions regarding clinician's current practice for the assessment and management of paediatric ASBD. Questions addressed basic demographic information; exposure to and confidence in managing ASBD; current management practices and thoughts on future research in this area.
Clinicians were also presented with five clinical vignettes, each describing young people of different ages, weights, comorbidities and underlying causes for their ASBD. Respondents were asked to indicate whether they would provide medication to each child, and if so, to select the route, medication and dose that they would offer.
Study data were collected and managed using REDCap (research electronic data capture) hosted at the Murdoch Children's Research Institute. 19 Approval to conduct the study was obtained from the Royal Children's Hospital Human Research Ethics Committee (HREC/59344/RCHM‐2019).
Data analysis
Descriptive statistics were prepared using Stata (16.1; StataCorp LLC, College Station, TX, USA).
Results
Of the 697 medical staff invited to participate, 227 (33%) responded. The majority of respondents held a Fellowship of the Australasian College for Emergency Medicine (FACEM), had been practising medicine for 10 or more years (92%) and worked in EDs that provided care to both adults and paediatric patients (58%) (Table 1). Participants from all states and territories of Australia except for the Australian Capital Territory were included.
TABLE 1.
Respondent characteristics
| n (%) | |
|---|---|
| Primary place of practice | n = 227 |
| Victoria | 75 (33) |
| New South Wales | 32 (14) |
| Western Australia | 29 (13) |
| Queensland | 49 (22) |
| South Australia | 25 (11) |
| Tasmania | 13 (6) |
| Northern Territory | 4 (2) |
| Fellowship held | |
| FACEM | 123 (54) |
| FRACP | 22 (10) |
| FRACP or FACEM with PEM qualification | 63 (28) |
| FRACGP/FACCRM | 8 (4) |
| No fellowship | 11 (5) |
| Years in practice | |
| <10 years | 19 (8) |
| 10–20 years | 100 (44) |
| 21–30 years | 78 (34) |
| >30 years | 30 (13) |
| Primary place of work | n = 227 |
| Paediatric ED | 96 (42) |
| Mixed ED (paediatric and adult) | 131 (58) |
FACCRM, Fellowship of the Australian College of Rural and Remote Medicine; FACEM, Fellowship of the Australasian College for Emergency Medicine; FRACGP, Fellowship of the Royal Australian College of General Practitioners; FRACP, Fellowship of the Royal Australasian College of Physicians; PEM, paediatric emergency medicine.
Paediatric ASBD appears to be a common clinical condition in Australian EDs (Fig. 1). The majority of clinicians (51%) reported they are caring for two or more young people with ASBD each week. In paediatric‐specific EDs, one in five clinicians (21%) reported caring for more than five young people with ASBD in an average week.
Figure 1.

Number of children and adolescents with acute severe behavioural disturbance each clinician reported they were caring for in an average week. ( ), Paediatric EDs; (
), Paediatric EDs; ( ), mixed EDs; (
), mixed EDs; ( ), overall.
), overall.
Most respondents agreed that they felt confident attempting verbal de‐escalation (79%) (Fig. 2). The majority also reported feeling confident providing oral (84%), intramuscular (IM) (74%) and intravenous (IV) (64%) sedation for paediatric ASBD (full details in Table S1).
Figure 2.
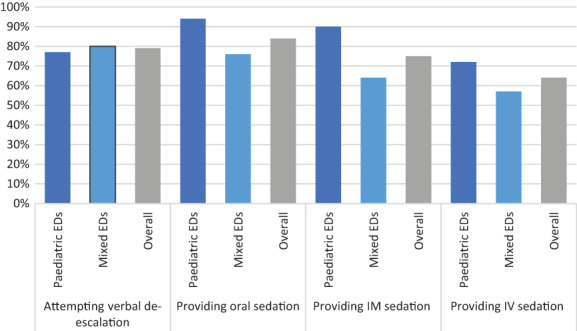
Clinician confidence in managing paediatric acute severe behavioural disturbance.
Most clinicians (81%) are not using a sedation/agitation rating scale when managing these young people (Table S2).
If medication provision was required to assist with behavioural containment, most clinicians (69%) use a guideline to determine which medication and dose to provide (Table S2). Guideline use was reported as higher by those working in paediatric EDs (84%) than in mixed EDs (57%). The Royal Children's Hospital Melbourne CPG 14 was the most commonly selected guideline (38%) with 33% of total respondents from Victoria.
Clinicians reported that when providing parenteral sedation, the behavioural endpoint they were aiming to achieve was a patient who is asleep but rouses if their name is called (68%) (Table S3). Clinicians working in mixed departments were more likely (75%) to aim for this level of sedation than those working in paediatric‐specific EDs (59%), where one‐third of clinicians (33%) said they were aiming for a patient who is awake and responds easily.
Clinicians were asked to outline the timeframes that they felt it was reasonable to wait before providing a second or subsequent dose for further treatment of the young person's behavioural disturbance (Fig. 3, further details in Table S3). For oral medication, the majority of clinicians (69%) suggested waiting for 15–30 min. For IM sedation, most (71%) were waiting 15–30 min. For IV sedation, 78% would provide a subsequent dose after 5–10 min.
Figure 3.
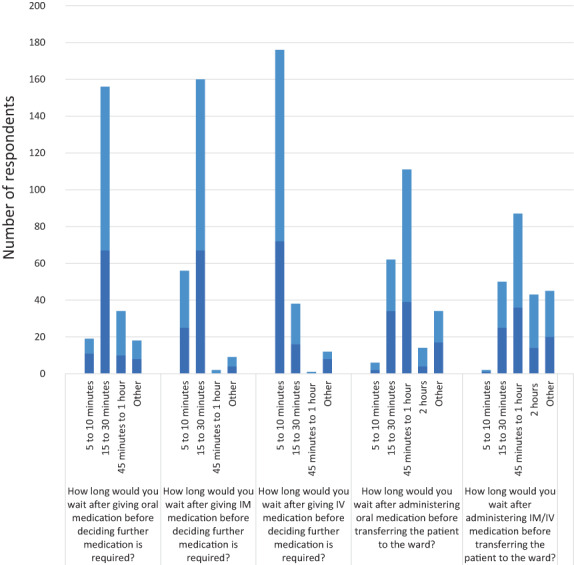
Medication dosing timeframes in paediatric acute severe behavioural disturbance. ( ), Paediatric EDs; (
), Paediatric EDs; ( ), mixed EDs.
), mixed EDs.
The majority of clinicians stated that they would be willing to transfer a patient from ED to the ward within 1 h of providing either oral and parenteral medication.
The first vignette (Fig. 4, further details in Table S4) presents a 14‐year‐old male with mild agitation likely secondary to recreational substance use who is requesting medication to ‘calm him down’. The majority (84%) of respondents reported they would provide oral medication. This rate was higher in the mixed ED respondents (88%) than in the paediatric ED respondents (78%). No respondents suggested that they would use parenteral medication as their first choice. The most popular drug class selected was a benzodiazepine (75%). The majority of respondents used diazepam (59%) with a smaller proportion selecting lorazepam (16%). Nearly a quarter (24%) reported they would use olanzapine.
Figure 4.

Clinical vignettes. ( ), No medication; (
), No medication; ( ), oral; (
), oral; ( ), IM; (
), IM; ( ), IV.
), IV.
The second vignette also presents a mildly agitated 15‐year‐old male who has a diagnosis of ASD. Just over half of the participants (51%) responded that they would not provide any medication. Of those clinicians that reported they would provide medication, all except one selected oral medication as their first choice (49%). The most popular oral medication selected was olanzapine (45%).
In the third vignette, a 10‐year‐old male presents from out of home care after an altercation occurred there. He is agitated and verbally aggressive but is co‐operative. The majority (66%) would not provide medication in this instance. Of those that did, all reported they would provide oral medication (34%). There was a range of medications selected as the first option, with diazepam (39%), olanzapine (39%) and lorazepam (20%) being the most popular.
The fourth vignette describes a 10‐year‐old male who presents from school by ambulance, accompanied by police. He has psychomotor agitation and is handcuffed to the ambulance trolley. He has a diagnosis of ASD and an intellectual disability. There was wide variability in the approach to managing this child. A small proportion (7%) of clinicians stated they would not provide any medication. Of those that did provide medication, oral was offered in 29% of cases, IM provided in 59% and IV in 6%. Those working in mixed departments more often (76%) used a parenteral medication as first‐line than those working in a paediatric ED (49%). Antipsychotic medication was the most common drug class across the oral and IM routes, with 63% using oral olanzapine, 55% using IM droperidol. Those clinicians who selected IV medication were more likely to use midazolam (62%).
The final vignette presents a 15‐year‐old female with significant agitation who has been mechanically restrained by police and the ambulance service. This agitation may be attributable to substance use. In this case, 97% of clinicians would provide some form of medication. A small proportion (13%) stated they would use oral medication, the majority (71%) would use IM medication and remaining (13%) would use IV. Similar to vignette four, the rate of parenteral medication use was higher in mixed EDs (92% vs 74%). There was variability in the medications selected across all routes. Diazepam (40%) and olanzapine (43%) were popular oral agents. Droperidol (63%) was the most selected IM medication. Midazolam (59%) was most commonly used IV.
Discussion
Paediatric ASBD is a relatively common condition. Most respondents reported caring for at least two children per week with the condition, felt confident regarding the major components of management, and referred to local CPGs. Despite this, we have identified considerable variation in self‐reported practice, particularly regarding medication use, and use of agitation/sedation rating scales.
The five posed clinical vignettes demonstrated significant variability in clinical practice. This is likely because of the limited evidence‐base, and variability across currently published Australian CPGs. 14 , 15 , 16 , 17 The most commonly selected oral medications were olanzapine and diazepam. In the vignettes in which clinicians elected to provide parenteral medication, there was a clear difference in drug class across the IM and IV routes. When providing IM medication, clinicians were most likely to use droperidol. When administering medication IV, clinicians were more likely to select midazolam. This is consistent with most CPGs, with recommendations for IM antipsychotic medications as first‐line parenteral agents, with IV midazolam recommended for refractory cases. 14 , 15 , 16 , 17
Of note, although patients in vignettes 4 and 5 were both profoundly agitated, they were managed differently by respondents. In vignette 4, the young male has a known diagnosis of both ASD and an intellectual disability and 65% of respondents reported they would provide parenteral medication. In the fifth vignette, the young female is also highly agitated with recent recreational substance use likely contributing to her ASBD, and 84% of respondents reported they would provide parenteral medication.
The reasons for these differences are unclear, but the patients' underlying comorbidities may be influencing medication choice. Previous retrospective literature has demonstrated that young people with neurodevelopmental disorders such as ASD commonly experience ASBD when presenting with mental health complaints. 12 Those with neurodevelopment disorders experience higher rates of physical restraint, seclusion and medication utilisation than their neurotypical counterparts. 12 Therefore, it is interesting that when presented a scenario with a child with this condition, clinicians reported that they were less likely to provide parenteral medication than to a young person with ASBD following substance use.
Although young people with ASBD are a common challenge for emergency physicians, there is inconsistent self‐reported practice, presumably because of the current gaps in evidence. Currently, the CPGs are based on expert opinion or have been extrapolated from the adult literature. To ensure that these young people have access to the most effective management, robust research into this clinical condition and the most effective non‐pharmacological and pharmacological strategies is required.
Once this evidence is available, the PREDICT network aims to utilise a knowledge translation strategy to create a national guideline for the management of paediatric ASBD in the ED setting. This guideline will assist in improving consistency in practice for this vulnerable cohort of patients.
Limitations
Our study has a number of limitations. The response rate for this survey was 33% which means the results may not be generalisable to all clinician's views; clinicians interested in the topic may be more likely to have responded. The strength of the responding cohort is that they are derived from a range of EDs across all states of Australia, from both tertiary and regional/rural settings, and represent clinicians from a range of disciplines.
As this is an electronic survey, clinicians' management recommendations may not represent how, in reality, they would manage that same young person in the ED.
Finally, as this survey targeted senior clinicians, it is not clear how doctors in training may manage this cohort. This is important, as they are often the sole decision makers overnight.
Conclusion
Senior ED clinicians regularly manage and are confident in providing care to young people with ASBD. Although most clinicians use CPGs to guide their management, there is significant variation, including medication choice and route of administration. Further prospective research relating to the epidemiology and effective management strategies for paediatric ASBD is required.
Author contributions
EMB developed the initial survey with feedback and review by JCK, SC and FEB. EMB coordinated the distribution of the survey and collection of responses. EMB analysed the responses and drafted the manuscript with input from all other authors.
Competing interests
FEB and SC are section editors for Emergency Medicine Australasia and were excluded from the peer‐review process and all editorial decisions related to the acceptance and publication of this article. Peer‐review was handled independently by members of the editorial board to minimise bias.
Supporting information
Table S1. Exposure to and confidence in managing ASBD.
Table S2. Use of scales and guidelines.
Table S3. Current practices regarding management of paediatric ASBD.
Table S4. Clinical vignettes.
Appendix S1. Management of paediatric acute severe behavioural disturbance (ASBD) in the ED.
Appendix S2. Management of paediatric acute severe behavioural disturbance (ASBD): a clinician survey.
Acknowledgements
We thank the PREDICT site representatives who have distributed the surveys: Franz Babl (Royal Children's Hospital), Amie Beattie (Tamworth Rural Referral Hospital), Meredith Borland (Perth Children's Hospital), Elyssia Bourke (Ballarat Health Services), Paul Buntine (Eastern Health: Box Hill Hospital, Angliss Hospital, Maroondah Hospital), Simon Craig (Monash Children's Hospital), Lalith Gamage (Port Augusta Hospital), Shane George (Gold Coast University Hospital), Nicola Ghedina (St John of God Midland Hospital), Jeremy Furyk (Barwon Health), Lambros Halkidis (Cairns Hospital), Jason Hort (Children's Hospital at Westmead), Alex King (Toowoomba Hospital), Amit Kochar (Women's and Children's Hospital Adelaide), Anna Lithgow (Royal Darwin Hospital), Ben McKenzie (Bendigo Health), Rob Millar (Austin Health), Natalie Phillips (Queensland Children's Hospital), Arjun Rao (Sydney Children's Hospital), Stephen Teo (Blacktown and Mt. Druitt Hospitals), Viet Tran (Royal Hobart Hospital), Tristan Turner (Townsville Hospital and Health Service), Russell Young (Albany Health Service), Michael Zhang (John Hunter Hospital). EMB is funded by a National Health and Medical Research Council (NHMRC) postgraduate scholarship, Canberra, Australia. FEB is funded by a grant from the Royal Children's Hospital Foundation and a NHMRC Practitioner Fellowship. The Royal Children's Hospital and the Murdoch Children's Research Institute, Parkville, Australia, are supported by the Victorian Government's Operational Infrastructure Support Program. This project is supported by the Medical Research Future Fund (MRFF) Million Minds Mission 2019 (GNT1179137): The Kids are Not Okay: ED management of acute mental health crises in children and young people. Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
Contributor Information
Elyssia M Bourke, Email: elyssia.bourke@mcri.edu.au.
the Paediatric Research in Emergency Departments International Collaborative (PREDICT) Research Network:
Franz Babl, Amie Beattie, Meredith Borland, Elyssia Bourke, Paul Buntine, Simon Craig, Lalith Gamage, Shane George, Nicola Ghedina, Jeremy Furyk, Lambros Halkidis, Jason Hort, Alex King, Amit Kochar, Anna Lithgow, Ben McKenzie, Rob Millar, Natalie Phillips, Arjun Rao, Stephen Teo, Viet Tran, Tristan Turner, Russell Young, and Michael Zhang
Data availability statement
The data that supports the findings of this study are available in the supplementary material of this article.
References
- 1. Stevenson R, Derek TK. Acute behavioural disturbance: a physical emergency psychiatrists need to understand. BJPsych Adv. 2021; 27: 333–42. [Google Scholar]
- 2. Oliver M, Adonopulos AA, Haber PS et al. Impact of acutely behavioural disturbed patients in the emergency department: a prospective observational study. Emerg. Med. Australas. 2019; 31: 387–92. [DOI] [PubMed] [Google Scholar]
- 3. Calver L, Drinkwater V, Gupta R, Page CB, Isbister GK. Droperidol v. haloperidol for sedation of aggressive behaviour in acute mental health: randomised controlled trial. Br. J. Psychiatry 2015; 206: 223–8. [DOI] [PubMed] [Google Scholar]
- 4. Calver L, Page CB, Downes MA et al. The safety and effectiveness of droperidol for sedation of acute behavioural disturbance in the emergency department. Ann. Emerg. Med. 2015; 66: 230–8. [DOI] [PubMed] [Google Scholar]
- 5. Chan EW, Taylor DM, Knott JC, Phillips GA, Castle DJ, Kong DC. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicentre, randomized, double‐blind, placebo‐controlled clinical trial. Ann. Emerg. Med. 2013; 61: 72–81. [DOI] [PubMed] [Google Scholar]
- 6. Chan EW, Lao KS, Lam L et al. Intramuscular midazolam, olanzapine, or haloperidol for the management of acute agitation; a multi‐centre, double‐blind, randomised clinical trial. EClinicalMedicine 2021; 32: 100751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Taylor DM, Yap CY, Knott JC. Midazolam‐droperidol, droperidol, or olanzapine for acute agitation: a randomized clinical trial. Ann. Emerg. Med. 2017; 69: 318–26. [DOI] [PubMed] [Google Scholar]
- 8. Isbister GK, Calver LA, Page CB, Stokes B, Bryant JL, Downes MA. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioural disturbance: the DORM study. Ann. Emerg. Med. 2010; 56: 392–401. [DOI] [PubMed] [Google Scholar]
- 9. Gerdtz M, Yap CY, Daniel C, Knott JC, Kelly P, Braitberg G. Prevalence of illicit substance use among patients presenting to the emergency department with acute behavioural disturbance: rapid point‐of‐care saliva screening. Emerg. Med. Australas. 2020; 32: 473–80. [DOI] [PubMed] [Google Scholar]
- 10. Carison A, Babl FE, Hill A, O'Donnell SM. Children and adolescents with severe acute behavioural disturbance in the emergency department. Emerg. Med. Australas. 2020; 32: 747–55. [DOI] [PubMed] [Google Scholar]
- 11. Lovett CJ, Hiles JA, Calver L, Pallas JD, Thomas Bowe K, Downes MA. Factors associated with paediatric and adolescent emergency department presentations involving acute behavioural disturbance events. J. Paediatr. Child Health 2022; 58: 110–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bourke EM, Say DF, Carison A et al. Emergency mental health presentations in children with autism spectrum disorder and attention deficit hyperactivity disorder. J. Paediatr. Child Health 2021; 57: 1572–9. [DOI] [PubMed] [Google Scholar]
- 13. Yap CLC, Taylor DMD, Kong DCM et al. Risk factors for sedation‐related events during acute agitation management in the emergency department. Acad. Emerg. Med. 2019; 26: 1135–43. [DOI] [PubMed] [Google Scholar]
- 14. Royal Children's Hospital . The Royal Children's Hospital Melbourne. 2020. [Cited 15 Apr 2022.] Available from URL: https://www.rch.org.au/clinicalguide/guideline_index/Acute_behavioural_disturbance__Acute_management/
- 15. New South Wales Health, New South Wales Government . Management of Patients with Acute Severe Behavioural Disturbance in Emergency Departments. 2015. [Cited 15 Apr 2022.] Available from URL: https://www.health.nsw.gov.au/kidsfamilies/MCFhealth/Documents/management‐of‐patients‐with‐acute‐severe‐behavioural‐short.pdf
- 16. Perth Children's Hospital . Government of Western Australia Child and Adolescent Health Service. 2020. [Cited 15 Apr 2022.] Available from URL: https://pch.health.wa.gov.au/For-health-professionals/Emergency-Department-Guidelines/Behavioural-problems
- 17. Children's Health Queensland Hospital and Health Service, Queensland Government . Management of Patients with Acute Behavioural Disturbance. 2017. [Cited 15 Apr 2022.] Available from URL: https://www.childrens.health.qld.gov.au/wp-content/uploads/PDF/guidelines/gdl-00732.pdf
- 18. Page CB, Parker LE, Rashford SJ, Isoradi KZ, Isbister GK. A prospective study of the safety and effectiveness of droperidol in children for prehospital acute behavioural disturbance. Prehosp. Emerg. Care 2019; 23: 519–26. [DOI] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata‐driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009; 42: 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Exposure to and confidence in managing ASBD.
Table S2. Use of scales and guidelines.
Table S3. Current practices regarding management of paediatric ASBD.
Table S4. Clinical vignettes.
Appendix S1. Management of paediatric acute severe behavioural disturbance (ASBD) in the ED.
Appendix S2. Management of paediatric acute severe behavioural disturbance (ASBD): a clinician survey.
Data Availability Statement
The data that supports the findings of this study are available in the supplementary material of this article.


