Abstract
The dry root of the soybean plant Astragalus membranaceus (Fisch) Bge. var. mongholicus (Bge) Hsiao or A. membranaceus (Fisch) Bge, Astragali Radix (AR) has a long medicinal history. Astragalus polysaccharide (APS), the natural macromolecule that exhibits immune regulatory, anti-inflammatory, anti-tumor, and other pharmacological activities, is an important active ingredient extracted from AR. Recently, APS has been increasingly used in cancer therapy owing to its anti-tumor ability as it prevents the progression of prostate, liver, cervical, ovarian, and non-small-cell lung cancer by suppressing tumor cell growth and invasion and enhancing apoptosis. In addition, APS enhances the sensitivity of tumors to antineoplastic agents and improves the body’s immunity. This macromolecule has prospects for broad application in tumor therapy through various pathways. In this article, we present the latest progress in the research on the anti-tumor effects of APS and its underlying mechanisms, aiming to provide novel theoretical support and reference for its use in cancer therapy.
Keywords: Astragalus polysaccharides, anti-tumor therapy, cancer, anti-tumor mechanism, apoptosis, autophagy
1. Introduction
According to the 2020 Global Cancer Statistical Report, cancer is the second leading cause of death globally, with an increase in incidence in recent years (1, 2). Malignant tumors are the primary reason for chronic noninfectious disease-related deaths and are the chief obstacle to a better life expectancy (3). Both gene mutation and epigenetic changes are important factors that lead to cancer occurrence and progression (4). Epigenetics refers to the reversible and heritable changes in gene function without changes in the nuclear DNA. Epigenetic changes include histone modification, DNA methylation, chromatin remodeling, and non-coding RNA regulation, which can affect the expression and silencing of oncogenes and tumor suppressor genes, respectively (4–7). Therefore, epigenetic regulation offers a promising direction and strategy for the development of anti-tumor therapeutics. However, as the pathogenesis of cancer remains unclear, the development of effective treatment methods is limited. Currently, cancer treatment primarily involves surgical resection, radiotherapy, chemotherapy, or a combination of two or all three approaches. During treatment, both cancerous and normal cells are killed, triggering a series of adverse reactions and toxic side effects with varying degrees of impact on prognosis and patients’ quality of life (QOL). Recently, with advancements in tumor microenvironment research, immunotherapy has emerged as a promising therapeutic approach (8, 9). Tumor immunotherapies, such as the use of immune checkpoint inhibitors (targeting programmed cell death protein-1, programmed cell death ligand-1, cytotoxic T lymphocyte-associated antigen 4, etc.) and adoptive cell transfer (such as chimeric antigen receptor T-cell therapy, T cell receptor-engineered T cells therapy, tumor-infiltrating lymphocytes therapy, etc.) (10–13), have demonstrated promising outcomes; however, their efficacy must be validated using clinical trial.
Traditional Chinese medicine has been essential in tumor prevention and management, with significant advantages, particularly in improving and managing clinical symptoms, enhancing the efficacy of anti-cancer drugs, reducing the toxicity of radio- and chemotherapies, enhancing the patient’s immunity and QOL, and effectively prolonging survival time (14), making it a critical strategy for tumor prevention and management. Astragali Radix (AR), a common traditional Chinese herbal medicine used in China for over 2,000 years, is also extensively used in numerous countries and has been included in the pharmacopeias of the United States, Japan, and South Korea (15). Medical research shows that AR exhibits various therapeutic activities, including anti-tumor (16–19), anti-aging (20), immune regulatory (21), anti-fibrosis (22), antibacterial (23), antiviral (24, 25), and anti-radiation (26) effects. Astragalus polysaccharide (APS), a major active component of AR (27–30), is extensively used in medicine as it demonstrates beneficial activities and low toxicity (31).
APS is a mixture of macromolecules, mainly composed of glucans (both water-soluble and water-insoluble) and heteropolysaccharides (mostly water-soluble and acidic), with molecular weights ranging from 8.7×103 to 4.8×106 Da (31–34). According to recent pharmacological studies, APS has a wide spectrum of biological activities, such as anti-inflammatory (35–37), immune regulation (38, 39), anti-fiber (40), anti-radiation (41, 42), anti-aging (21), anti-metabolic disorders (43), protective effects on the cardiovascular system (44, 45), anti-diabetes (46), anti-tumor (47, 48), and anti-infection (49).
Owing to its high efficacy and low toxicity, the role and value of APS in the management of malignancies have garnered increasing research attention in recent years. The anti-cancer mechanism of APS involves inducing the apoptosis of tumor cells by regulating various pathways; inhibiting proliferation, migration, and invasion of tumor cells; regulating immune function and autophagy; and enhancing the efficacy of chemotherapeutic or targeted drugs by reducing their toxicity. However, a comprehensive understanding of how APS works has not been put into perspective. In this study, the anti-tumor mechanisms of APS and its targets are comprehensively reviewed to render a new theoretical basis for cancer treatment.
2. Anti-tumor mechanism of APS
2.1. Role of APS in inducing tumor cells apoptosis
Apoptosis, also referred to as programmed cell death, plays a key role in maintaining internal environment homeostasis (50, 51). Induction of cell death is a major mechanism underlying the activity of anti-tumor drugs (52).
2.1.1. B-cell lymphoma-2 (Bcl-2) family
The Bcl-2 family contains a class of molecules involved in apoptosis-associated pathway modulation. Bcl-2 is an anti-apoptosis gene highly expressed in various tumors (53, 54), whereas Bcl-2-associated X (Bax) is a pro-apoptotic gene (55). Huang et al. proposed that APS induces H22 (a hepatocellular cancer [HCC] cell line) apoptosis by downregulating Bcl-2 and upregulating Bax expression (56). Similarly, Lv et al. reported that after APS treatment, the apoptosis of HepG2 cells is accelerated (57). Specifically, APS decreased the levels of Bcl-2, β-catenin, c-myc, and Cyclin D1 in cells, suggesting that the mechanism of tumor suppression may be related to the inhibition of Bcl-2 expression by downregulating the Wnt/β-catenin signaling pathway. Xie et al. provided additional data demonstrating that APS effectively inhibited the growth of MDA-MB-231 (a human breast cancer [BC] cell line) graft tumor (58). In terms of mechanism, APS concentration-dependently increased Bax protein expression and decreased Bcl-2 protein expression, thus inducing MDA-MB-231 apoptosis.
2.1.2. miRNA pathway
miRNAs, endogenous non-coding small RNAs that are critical in regulating almost all signaling pathways in eukaryotic cells (59), have recently been found to participate in tumor occurrence and progression by regulating apoptotic signaling pathways (60–63). miR-27a is over-expressed in various tumor cells (64–66). Guo et al. found that APS significantly and dose-dependently reduced miR-27a levels in cells, subsequently upregulating the expression of the tumor suppressor gene FBXW7, thereby inhibiting OV-90 and SKOV-3 proliferation and significantly increasing apoptosis (67). miR-133a, which inhibits cancer cell growth in multiple tumors, is considered a tumor suppressor molecule (68–70). According to Chu et al., after APS treatment, the apoptosis rate of human osteosarcoma MG63 cells increased owing to the upregulation of miR-133a and inactivation of the JNK signaling pathways (71).
2.1.3. Extrinsic apoptosis pathways
Extrinsic apoptosis, one of the major pathways of apoptosis, is mediated by death receptors on the cell surface (72). The binding of Fas ligands to Fas receptors or tumor necrosis factor (TNF) receptors to TNF ligands is the primary way of initiating this apoptotic pathway (73–75). Fas and its ligands, a class of important apoptosis-inducing molecules, exist in various tumor cells (76, 77). In an in vitro study of colon cancer CD133+/CD44+ cells, Li and Shen found that APS can induce apoptosis by activating the Fas death receptor pathway. Specifically, APS increases Fas expression and induces apoptosis in a concentration-dependent manner (78).
2.1.4. p53 protein
The p53 protein is a vital tumor suppressor, and its loss of function is a prerequisite for cancer development (79). In various cancers, p53 is a dominant force promoting apoptosis, cell cycle arrest, and DNA repair (80–83). Zhang et al. showed that APS could activate p53 and p21 and inhibit the expression of Notch1 and Notch3 in vitro, ultimately inhibiting cell proliferation and promoting their apoptosis (84) ( Table 1 ).
Table 1.
Effects of APS on the signaling pathways of apoptosis.
| Test type | Cancer types | Cell type/Animal model | Dosage/concentrations | Signaling pathways (↑upregulation, ↓downregulation) |
REF |
|---|---|---|---|---|---|
| in vitro | Hepatocellular carcinoma | H22 cells | 0.1, 0.5, 1 mg/mL | Bcl-2↓ and Bax↑ | (56) |
| Liver cancer | HepG2 cells | 100, 200 mg/L | Bcl-2↓, β-catenin↓, c-myc↓, Cyclin D1↓ and Wnt/β-catenin↓ | (57) | |
| Ovarian cancer | OV-90 cells and SKOV-3 cells | 0–2 mg/mL | miR-27a↓ and FBXW7↑ | (67) | |
| Osteosarcoma | MG63 cells | 10 mg/mL | miR-133a ↑and JNK↓ | (71) | |
| Colon cancer | RKO cells | 12.5, 25, 50 mg/mL | Fas↑ | (78) | |
| Non-small cell lung cancer | H460 cells | 0–30 mg/mL | p53↑, p21↑, Notch1↓and Notch3↓ | (84) | |
| in vivo | Breast cancer | BALB/c-nu nude mice♀, MDA-MB-231 cells | 200, 400 mg/kg bw | Bax↑ and Bcl-2↓ | (58) |
Bcl-2, B-cell lymphoma-2; Bax, Bcl-2-associated X; Cyclin D1, G1/S-Specific cyclin-D1; c-myc, Myelocytomatosis viral oncogene homolog; Wnt/β-catenin , Wnt/β-catenin signaling pathway; FBXW7, F-box/WD repeat-containing protein 7; JNK, c-Jun N-terminal kinases; Fas, Fas transmembrane glycoprotein; p53, p53 protein; p21, p21 protein.
2.2. Suppression of cancer cell proliferation
Tumors promote abnormal cell proliferation and metabolic activity by disrupting the regulation of growth-promoting signals (85); therefore, suppressing tumor cell proliferation is a vital strategy in the treatment of tumors.
2.2.1. Promotion of cell cycle arrest
Cell cycle regulation is coordinated by a complex network of interactions between enzymes, cytokines, and cell cycle signaling pathways. This regulation is essential for cell proliferation, growth, and repair (86). Abnormal regulation of the cell proliferation cycle is a major cause of tumor initiation (87). In an in vitro experiment, by inhibiting the JAK2/STAT3 pathway, Liu et al. found that APS induced the cell cycle of bladder cancer UM-UC-3 to stop in the G0/G1 phase, thus inhibiting its proliferation (88). Additionally, Yu et al. provided new evidence demonstrating that APS promotes mouse solid tumor S180 cell apoptosis in a dose-dependent manner through S-phase arrest (89). An in vitro study of APS against the proliferation of HCC cells established that APS increased the G1 phase arrest of human hepatoma HepG2 cells, enhanced their autophagic activity, suppressed proliferation, and enhanced apoptosis by inhibiting the AKT axis (90). Yan et al. showed that APS could inhibit the proliferation of colon cancer SW620 cells through cell cycle arrest, with G2/M phase arrest playing a dominant role (91).
2.2.2. Others
Abnormal activation of cell signal transduction pathways is closely related to the occurrence and development of malignant tumors (92, 93). In an in vitro experiment, APS was found to inhibit RT4 and T24 proliferation and migration by inducing the accumulation of Fe2+ and malondialdehyde in cells, and ferrostatin, an iron ptosis inhibitor, reversed this reaction (94). Furthermore, APS was found to reduce GPX4 expression, inhibit the activity of the light chain subunit SLC7A11 (xCT), and promote the formation of BECN1-xCT complex by activating AMPK/BECN1 signaling. These findings demonstrated the ability of APS to inhibit urothelial carcinoma progression by inducing iron ptosis. According to Guo et al., APS attenuated the proliferative and invading capacities of prostate cancer cells (PC3 and DU145) in vitro and inhibited PC3 xenograft growth in vivo, time- and dose-dependently (95). Moreover, APS significantly inhibited tumor development by upregulating miR-138-5p expression and inhibiting SIRT1 and SREBP1 expression. Furthermore, APS significantly suppresses HeLa cell growth, invasion, and migration (96). This may be achieved by increasing SHP2 and SOCS3 protein levels in cells and inhibiting JAK-STAT pathway overactivation. Wu et al. demonstrated that APS could control the proliferation of lung cancer cells (A549 and NCI-H358 cells) by inhibiting the NF-κB signaling pathway (97) ( Table 2 ).
Table 2.
Effects of APS on the signaling pathways of proliferation.
| Test type | Cancer types | Cell type/Animal model | Dosage/concentrations | Signaling pathways (↑upregulation, ↓downregulation) |
REF |
|---|---|---|---|---|---|
| in vitro | Bladder cancer | UM-UC-3 cells | 500, 1000 mg/mL | G0/G1 phase arrest and JAK2/ STAT3↓ | (88) |
| Liver cancer | HepG2 cells | 25, 50, 100 μg/mL | G1 phase arrest, AKT↓ and p-AKT↓ | (90) | |
| Colon cancer | SW620 cells | 1 g/L | G2 /M phase arrest | (91) | |
| Urothelial carcinoma | RT4 cells and T24 cells | 10, 15 μm | Fe2+↑, BECN1-xCT↑, GPX4↓, xCT↓ and AMPK/BECN1↑ | (94) | |
| Prostate cancer | PC3 cells and DU145 cells | 0-40 mg/mL | miR-138-5p↑, SIRT1↓ and SREBP1↓ | (95) | |
| Cervical cancer | Hela cells | 0–16 mg/mL | SHP2↑, SOCS3↑ and JAK-STAT↓ | (96) | |
| Non-small cell lung cancer | A549 cells and NCI-H358 cells | 20, 40 mg/mL | NF-κB↓ | (97) | |
| in vivo | Ascites tumor | Kunming mice , S180 cells |
150, 300 mg/kg bw | S phase arrest | (89) |
JAK2, anus kinase 2; STAT3, Signal transducer of activators of transcription; AKT, Protein kinase B; p-AKT, phospho- Protein kinase B; BECN1, Beclin-1; GPX4, Glutathione peroxidase 4; xCT, Light chain subunit SLC7A11; AMPK, Adenosine monophosphate activated protein kinase; SIRT1, Silent mating type information regulation 2 homolog- 1; SREBP1, Recombinant Sterol Regulatory Element Binding Transcription Factor 1; SHP2, SH2 domain-containing protein tyrosine phosphatase 2; SOCS3, Suppressor of cy-tokine signaling proteins; NF-κB, Nuclear factor kappa-B.
2.3. Role of APS in inhibiting tumor invasion and metastases
Tumor invasion and metastases are strongly correlated with adverse prognoses, and the invasion of tumor cells is a prerequisite for metastases. Tumor metastasis is a complicated process involving multiple stages, genes, and gene products. Inhibiting tumor metastasis can prevent tumor cell spread to other body sites, thereby mitigating tumor progression (98).
2.3.1. Epithelial–mesenchymal transition (EMT) pathway
Multiple studies have linked EMT to tumor progression, invasion, and metastases (99, 100). Yang et al. found through in vitro experiments that APS significantly prevents human BC cells, MCF-7 and Mda-MB-231, from invasion and migration (101). Further research demonstrated the ability of APS to inhibit BC cell invasiveness and migration by regulating the Wnt/β-catenin axis. In addition, macrophage migration inhibitory factor (MIF), a pro-inflammatory factor that is critical in the onset and progression of intestinal, breast, and prostate carcinoma among other malignant tumors (102–104), induces EMT in cancer cells (105, 106). Liao et al. found that an injectable preparation of APS (PG2) dose-dependently inhibited the migratory and invasive activities of lung adenoma A549 cells (107). For specific performance, APS treatment led to reduced EMT markers (vimentin, AXL) and MIF levels in cells.
2.3.2. Regulation of miRNA expression
miRNAs contribute to the proliferation, invasion, and migration of tumor cells by regulating gene transcription (108) and play a key regulatory role in the pathological process of various human tumors. In vitro experiments utilizing A549 and NCI-H1299 by Tao et al. substantiated that APS treatment markedly attenuated the migration and invasiveness of non-small-cell lung cancer (NSCLC) cells compared to that seen with the control, and the underlying mechanism may be related to the APS-related increase in cellular miR-195-5p levels (109). Notably, the increased expression of miR-133a in cells after APS treatment effectively prevents the proliferation, migration, and invasion of prostate cancer cells (DU145) (110).
2.3.3. Vascular endothelial growth factor (VEGF) pathway
Tumor angiogenesis is the direct path of tumor cell metastasis (111). VEGF can promote tumor progression in patients with cancer by regulating angiogenesis in cancer tissues (112, 113). Recent studies have shown that the downregulation of VEGF is a positive signal during tumor therapy (114). Zhao et al. reported that APS inhibits Lewis lung cancer growth and metastasis in mice by significantly reducing VEGF and EGFR expression in cancerous tissues (115). Additionally, in vitro studies by Tang and Li demonstrated that APS inhibits the metastasis of gastric cancer cells (SGC7901) induced by vascular endothelial cells (HUVECs) (116) ( Table 3 ).
Table 3.
Effects of APS on the signaling pathways of invasion.
| Test type | Cancer types | Cell type/Animal model | Dosage/concentrations | Signaling pathways (↑upregulation, ↓downregulation) |
REF |
|---|---|---|---|---|---|
| in vitro | Breast cancer | MCF-7 cells and Mda-MB-231 cells | 200, 400, 800 μg/mL | Cyclin D1↓, c-myc ↓and Wnt/β-catenin↓ | (101) |
| Non-small cell lung cancer | A549 cells and NCI-H1299 cells | 5, 10, 20 μg/mL | miR-195-5p↑ | (109) | |
| Prostate cancer | DU145 cells | 1, 2.5, 5 mg/mL | miR-133a↑ | (110) | |
| Gastric cancer | SGC7901 cells | 2.5, 5, 10, 20, 40 mg/mL | E-cadherin↑, Vimentin↓, MMP-13↓ and MMP-9↓ | (116) | |
| in vivo | Lung cancer | C57BL/6J mice and lung cancer Lewis tumor cells | 25, 50, 100 mg/kg bw | VEGF↓ and EGFR↓ | (115) |
| in vitro and in vivo | Adenocarcinoma of lung | A549 cells; NOD/SCID mice♂ |
0-1000μg/mL; 10, 40, 160 mg/kg bw |
E-cadherin↑, Vimentin↓, AXL↓ and MIF↓ | (107) |
Cyclin D1, G1/S-Specific cyclin-D1; c-myc, Myelocytomatosis viral oncogene homolog; Wnt/β-catenin , Wnt/β-catenin signaling pathway; MMP-13, Matrix metalloproteinase-13; MMP-9, Matrix metalloproteinase-9; VEGF, Vascular endothelial growth factor; EGFR, Epidermal growth factor receptor; MIF, Macrophage migration inhibitor factor; AXL, Recombinant AXL Receptor Tyrosine Kinase.
2.4. Nano-drug delivery systems can increase efficiency and reduce toxicity
APS is a mixture of hydrophilic macromolecules (117) that cannot easily penetrate cell membranes, with only a small portion absorbed through the intercellular space (118), limiting its clinical application. Nano-drug delivery systems are highly selective and can deliver drugs to specific sites to enhance therapeutic effects and reduce adverse reactions (119, 120). Therefore, they show great potential for the development and application of anti-tumor drug delivery to improve the therapeutic effects.
Selenium nanoparticles, by virtue of having high bioavailability, potent bioactivity, and low toxicity (121–123), exert significant inhibitory effects on various malignant tumors (124–126). Ji et al. prepared a novel functionalized nanocomposite using alcohol-soluble APS and selenium nanoparticles and found that it was effective in suppressing HepG2 proliferation and accelerating apoptosis by triggering S-phase arrest, thereby stimulating ΔΨm (mitochondrial membrane potential) depletion, increasing the Bax/Bcl-2 ratio, and promoting intracellular reactive oxygen species accumulation (127). Jiao et al. developed selenium nanoparticles modified with macromolecular weight APS and observed positive results in hepatoma treatment, as indicated by the induction of apoptosis and inhibition of proliferation of HepG2 cells (128). The mechanism involved may be related to the increasing S-phase block, the significant enhancement of Bax levels, and the marked reduction of Bcl-2 levels and ΔΨm value. Studies have shown that the selenium nanoparticles modified by APS are cytotoxic to MCF-7 cells. This cytotoxicity is achieved by the induction of apoptosis through the mitochondrial pathway and the activation of autophagy at an early stage and inhibiting it at a late stage (129). Moreover, Huang et al. successfully constructed APS superparamagnetic iron-oxide nanocomposites and demonstrated that they could effectively induce M1 polarization of mouse monocytic macrophage RAW264.7 and improve the killing ability of macrophages against HepG2 cells in vitro. Furthermore, no inhibitory effect on macrophage proliferation was observed (130).
2.5. Combination of APS with anti-tumor drugs improves effectiveness and reduces toxicities
Resistance to chemotherapy is the primary reason for treatment failure and poor prognoses. Therefore, focusing on the mechanism of drug resistance and inhibiting it in tumor cells is essential to reducing drug resistance and optimizing effectiveness while improving patient survival rates.
2.5.1. Cisplatin (CDDP)
CDDP is widely used as an initial medication in cancer therapy owing to its exceptional ability to combat cancer and its broad spectrum of effectiveness against various cancer types. However, the prolonged utilization of this drug may result in the development of resistance, thereby restricting its practical implementation in clinical settings. The PI3K/AKT axis is crucial for tumorigenesis and progression (131). As indicated by Gong et al., APS reversed the acquired CDDP resistance in melanoma cell lines B16 in vivo by inhibiting the PD-L1/PI3K/AKT axis (132). Liu and Chen showed that APS was able to overcome the resistance of A549/CDDP cells to CDDP in vitro (133). Subsequent investigations revealed that APS can decrease the ΔΨm values and Bcl-2, p-PI3K, P-gp, and p-AKT levels while elevating Bax expression. This finding implies that the potential mechanism of action could encompass the inhibition of the PI3K/AKT pathway and stimulation of the mitochondrial apoptosis pathway. Lu et al. further demonstrated that APS combined with CDDP effectively inhibits proliferation, migration, and EMT progression of CDDP-resistant SW620 cells by inhibiting miR-10b-5p expression and upregulating AGPAT3 expression (134). The combination of APS and CDDP synergistically inhibits the invasion and metastasis of CNE-1 (a human nasopharyngeal carcinoma cell line). It is associated with the induction of G0/G1 and S phase arrest, downregulation of MMP-9 expression, and upregulation of p53 expression (135). Li et al. observed that APS could enhance the sensitivity of SKOV3 ovarian cancer cells to CDDP treatment by activating the mitochondrial apoptosis pathway and JNK1/2 signaling pathway (136).
2.5.2. Other drugs
In addition to CDDP, the application of APS can potentially augment the chemosensitivity of tumors to other medications. Li et al. showed that APS enhanced the sensitivity of HCC cells to doxorubicin chemotherapy and induced cancer cell apoptosis (137). In vitro tests have shown that by downregulating OGT (O-GlcNAc transferase) and upregulating OGA (O-GlcNAc transferase) expression in Hep3B cells, APS reduced O-GlcNAcylation and intensified endoplasmic reticulum stress responses. According to in vivo experiments, APS combined with doxorubicin inhibited xenograft tumor growth in mice, suggesting that APS can potentially be an optional sensitizer in HCC chemotherapy. A previous study demonstrated that APS effectively reversed the resistance of lung adenocarcinoma (PC9 and HCC827) cells to gefitinib by inhibiting the PD-L1/SREBP-1/EMT axis (138). In a mouse BC model, Bao et al. (139) found that APS effectively alleviated paclitaxel-induced cytotoxicity in mouse monocyte–macrophage RAW264.7 cells. The mechanism for this action is attributable to changes in the cell cycle and apoptosis. When studying the role of APS plus apatinib in human pancreatic cancer cell (ASPC-1 and PANC-1) proliferation and apoptosis, Wu et al. found that the combination therapy contributed to higher cell migration and invasion inhibition rates and apoptosis and lowered p-AKT, MMP-9, and p-ERK levels than those in the control group (140), suggesting that APS plus apatinib is a promising strategy for treating pancreatic cancer ( Table 4 ).
Table 4.
APS acts synergically with other chemotherapeutic drugs.
| Test type | Standard anti-cancer drugs |
Cancer types | Cell type/Animal model | Dosage/ concentrations | Signaling pathways (↑upregulation, ↓downregulation) | REF |
|---|---|---|---|---|---|---|
| in vitro | Cisplatin | Lung cancer | A549/CDDP cells | 100 mg/L | Bax↑, ΔΨm↓, Bcl-2↓, P-gp↓, and PI3K/AKT↓ | (133) |
| Colorectal cancer | SW620 cells, SW620/CDDP cells | 1 mg/mL | miR-10b-5p↓ and AGPAT3↑ | (134) | ||
| Nasopharyngeal carcinoma | CNE-1 cells | 200 μg/mL | MMP-9↓, p53↑, G0/G1 phase arrest and S phase arrest | (135) | ||
| Ovarian cancer | SKOV3 cells | 800 μg/mL | Bcl-2↓, Bax↑, caspase-3↑, and JNK1/2↑ | (136) | ||
| Gefitinib | Adenocarcinoma of lung | PC9 cells and HCC827 cells | 200 mg/L | PD-L1/SREBP-1/EMT↓ | (138) | |
| Apatinib | Pancreatic cancer | ASPC-1 cells and PANC-1 cells | 200 μg/mL | p-AKT↓, p-ERK↓ and MMP-9↓ | (140) | |
| in vivo | Taxol | Breast cancer | 4T1 cells, mouse mononuclear macrophage RAW264.7 and BALB/C mice | 40 mg/kg bw | G2/M phase arrest↓, Taxol-induced cytotoxicity↓ | (139) |
| in vitro and in vivo | Cisplatin | Melanoma | A375/CDDP cells, B16/CDDP cells; C57BL/6/SCID mice♂ |
200 mg/kg bw | PD-L1/PI3K/AKT↓ | (132) |
| Doxorubicin | Hepatocellular carcinoma | Hep3B cells; BALB/c nude mice♂ |
0-50 mg/L | OGT↓, OGA↑, O-GlcNAcylation↓ | (137) |
Bax, Bcl-2-associated X; ΔΨm, Mitochondrial membrane potential; Bcl-2, B-cell lymphoma-2; PI3K, Phosphatidylinositol-3-kinase; P-gp, P-glycoprotein; AKT, Protein kinase B; Fas, Fas transmembrane glycoprotein; AGPAT3, 1-acylglycerol-3-phosphate O-acyltransferase 3; MMP-9, Matrix metalloproteinase-9; p53, p53 protein; JNK, c-Jun N-terminal kinases1/2; PD-L1, Programmed cell death protein-ligand 1; SREBP1, Recombinant Sterol Regulatory Element Binding Transcription Factor 1; EMT, Epithelial-mesenchymal transition; p-AKT, phospho-Protein kinase B; p-ERK; phospho-Extracellular Regulated Protein Kinases; OGT, O-GlcNAc transferase; OGA, O-GlcNAcase;O-GlcNAcylation, Methods to detect the expression of O-GlcNAc.
2.6. Immunomodulation
The body’s immune system, through various pathways, identifies and removes mutated tumor cells under normal circumstances, which inhibits tumor cell growth to some extent. Recent evidence has indicated that immune suppression in the microenvironment before tumor metastasis is a key link in the initiation of tumor metastasis (141). Owing to its strong immunomodulating properties (142), APS can enhance the body’s immunity to treat various cancers.
Bamodu et al. reported that APS can downregulate the expression of interleukin (IL)-6/10, markedly increase the M1/M2 macrophage polarization ratio, contribute to the functional maturity of DC, enhance T cell-medicated anti-tumoral immune responses, improve the accuracy of tumor cell killing, and inhibit the growth of tumor cells (143). Wei et al. reported that, through the Notch signaling pathway, APS significantly promoted the production of cytokines such as IL-6 and TNF-α; increased the iNOS levels and polarization rate of M1/M2 macrophages; activated M1 macrophages; and inhibited M2 macrophages, thereby enhancing the killing and phagocytosis of tumor 4T1 cells and the inhibition of tumor growth and metastasis (144). Li et al. observed that the presence of APS can elevate the percentage of M1 macrophages within liver cancer tissues while simultaneously reducing the proportion of M2 macrophages, thereby inhibiting the growth of liver cancer tumor cells (145). Furthermore, APS activates the release of NO and TNF-α by macrophages, thus reinforcing the suppressive and killing impact of the immune system on MCF-7 BC cells (146).
Ding et al. showed that APS inhibits tumor growth in melanoma-bearing mice (147). Specifically, by regulating the composition of the intestinal flora and altering fecal metabolites, APS reduces the MDSC (Myeloid-derived suppressor cell) count, downregulates IL-10, arginase-1, and TGF-β expression, and decreases the immunosuppressive activity of MDSCs in mice with melanoma, thereby enhancing the killing ability of CD8+ T cells on tumors. Yu et al. prepared a novel APS using water at 4°C (148) and demonstrated that it activated anti-tumoral immune responses and enhanced anaerobic metabolism in the solid tumor microenvironment through the HIF-1 axis, ultimately promoting mouse S180 (a cancer cell line) apoptosis (89). He et al. injected APS into HCC BALB/c mice (100, 200, and 400 mg/kg per day for 12 consecutive days) and observed increased CD8+ T cell count, decreased PD-L1 levels, and reduced tumor size, weight, and volume. Furthermore, by upregulating miR-133a-3p and downregulating MSN, APS attenuated PD-L1-mediated immunosuppression, thereby suppressing tumors (149). Chang et al. found that APS downregulates PD-L1 protein levels by inhibiting the AKT/mToR/p70S6K axis, thereby enhancing the immune capacity of 4T1 (mouse BC) and CT26 (mouse colorectal cancer) cells (150) ( Table 5 ).
Table 5.
Immunomodulatory effects of APS.
| Test type | Cancer types | Cell type/Animal model | Dosage/concentrations | Signaling pathways (↑upregulation, ↓downregulation) |
REF |
|---|---|---|---|---|---|
| in vitro | Breast cancer | MCF-7 cells and RAW264.7 cells | 200-1000 μg/mL | TNF-α↑and NO↑ | (146) |
| in vivo | Melanoma | B16-F10 cells and C57BL/6 mice♂ | 200 mg/kg bw | MDSC↓, Arginase-1↓, interleukin-10↓, transforming growth factor-β↓ and CD8+T cells↑ | (147) |
| Ascites tumor | Kunming mice, S180 cells | 150, 300 mg/kg bw | HIF-1↑, CD3+ cells↑, CD4+ cells↑ and CD8+T cells↑ | (89) | |
| in vitro and in vivo | Non-small cell lung cancer | H441 cells, H299 cells, LLC1 cells; C57BL/6 mice♂ |
16 mg/ml; 3 mg/kg bw |
IL-6/10↓, M1/M2 macrophage polarization ratio↑ and DC functions mature↑ | (143) |
| Breast cancer | 4T1 cells, RAW264.7 cells; BALB/c mice♀ |
30, 100, 300 μg/mL | IL-6↑, TNF-α↑, iNOS↑ and M1/M2 macrophage polarization ratio↑ | (144) | |
| Hepatocellular carcinoma | MHCC97H cells, Huh7 cells, THP1 cells; BALB/c nude mice♂ |
8, 16 mg/mL; 50, 100, 200 mg/kg bw |
M1 macrophages↑ and M2 macrophages↓ | (146) | |
| Hepatocellular carcinoma | SMMC-7721 cells, Huh7 cells; BALB/c mice |
0.1, 0.5, 1 mg/mL; 100, 200, 400 mg/kg bw |
CD8+T cells↑, PD-L1↓, miR-133a-3p↑ and MSN↓ | (149) | |
| Breast cancer; Colon cancer |
4T1 cells and CT26 cells; BALB/c mice |
10,000 ng/ml; 50 mg/kg bw |
PD-L1↓ and AKT/mTOR/p70S6K↓ | (150) |
TNF-α, Tumor necrosis factor-α; NO, Nitric oxide; MDSC, Myeloid-derived suppressor cells; HIF-1, Hypoxia-inducible factor-1; IL-6/10, Interleukin-6/10; IL-6, Interleukin-6; iNOS, Inducible nitric oxide synthase; PD-L1, Programmed cell death protein-ligand 1; MSN, Moesin; AKT, Protein kinase B; mTOR, Mammalian rapamycin target protein; P70S6K, P70 ribosomal protein S6 kinase.
Chang et al. revealed that APS enhances immune responses in 4T1 and CT26 tumor-bearing mice by downregulating PD-L1 protein levels by inhibiting the AKT/mTOR/p70S6K axis (140).
2.7. Other anti-tumorigenic effects of APS
2.7.1. Lipid metabolism
Lipid metabolism is a major pathway of cellular energy metabolism. Abnormal lipid metabolism can promote tumor progression (151, 152), which is an indicator of human cancer (153).
Lipid metabolism is a complex regulatory process that provides energy, lipid chains, and a large amount of fats required for the formation of new cell membranes for rapidly dividing and proliferating cancer cells (154). Abnormal lipid metabolism is often accompanied by the anomalous overexpression of related enzymes (155), abnormal transcription of related non-coding RNA (156), and activation of carcinogenic signaling pathways (157). Cholesterol and its metabolites are signaling molecules that promote tumor development (158). Triglycerides are closely related to the growth of various tumor cells (159, 160). APS effectively lowers cholesterol and triglycerides (161, 162).
As indicated by a recent study, APS inhibits prostate cancer growth and lipid metabolism in vivo and in vitro (95). By upregulating miR-138-5p, APS significantly suppressed SIRT1 and SREBP1 expression, decreased cholesterol and triglyceride levels in PC3 and DU145, and attenuated cell proliferation. Therefore, the role played by APS in mediating lipid metabolism is important for the prevention of cancer progression.
2.7.2. Autophagy
Autophagy refers to the biological process by which cells undergo intracellular degradation via lysosomes to protect cell integrity and maintain homeostasis under the influence of external environmental stimuli and metabolic pressures (163, 164). It is strongly linked to carcinogenesis and progression of various cancers and plays a dual role in the tumor process (165–167).
Zhi et al. found that after APS treatment, the expression of LC3B-II/I was significantly increased in colorectal cancer HCT-116 cells, while the expression levels of p-PI3K/PI3K, p-AKT/AKT, p-mTOR/mTOR, and p62 were significantly decreased (168). Therefore, they proposed that APS can induce autophagy in colorectal cancer cells by inhibiting the PI3K/AKT/mTOR axis and the development of cancer cells. The proportions of Beclin1 and LC3B in EC109 esophageal cancer cells increased significantly after APS treatment (169). Based on these findings, Chang et al. believed that the anti-tumor mechanism of APS was related to the enhancement of autophagy induced by APS. Li and Shen found that APS elevated caspase-9, caspase-3, and Bax protein levels, decreased Bcl-2 protein expression, and inhibited CD133 and CD44 co-positive colon cancer stem cell proliferation time- and concentration-dependently (78). Moreover, APS concentration-dependently induced apoptosis and this effect was reversed by an autophagy antagonist. These results suggest that APS can inhibit proliferation and promote apoptosis by inducing autophagy in colon cancer stem cells. However, given the dual role of autophagy in tumorigenesis and cancer progression, its exact mechanism in cancers requires further exploration.
2.8. Clinical trials on the anti-tumor effect of APS
The elucidation of the efficacy, safety, and tolerability of drugs administered to patients is the main focus of a clinical trial.
PG2 has recently been found to normalize the neutrophils-to-lymphocytes ratio in patients with lung cancer on combined immune checkpoint inhibitor therapy, suggesting that APS could be used to supplement anti-tumor agents (170). A trial of PG2 plus cytokine-induced killer cells for advanced NSCLC demonstrated that PG2 notably increased the proportion of peripheral blood CD4+ and CD3+ T lymphocytes (171), thus significantly improving patients’ functional status and relieving symptoms of qi deficiency, with remarkable clinical safety. A clinical study investigating PG2 plus gefitinib therapy for advanced lung cancer showed markedly higher serum CD3+, CD4+, and CD4+/CD8+ cell counts in the observation group than in the control group after treatment, accompanied by a better QOL (higher KPS scores) and fewer toxic and side effects (172). This study demonstrated that PG2 combined with gefitinib for advanced NSCLC can improve patients’ immunity, alleviate toxicity and side effects, and improve patients’ overall QOL. Zheng et al. showed that PG2 has a protective effect on the bone marrow, which can reduce the myelotoxicity of platinum-containing drugs combined with other drugs in patients with NSCLC and improve patient tolerance to chemotherapy (173).
Concurrent radiotherapy and chemotherapy are standard therapies for patients with advanced head and neck squamous cell carcinoma; however, the resulting complications can affect patient QOL. Moreover, its efficacy is low. Relapse and metastases are found in half of the head and neck squamous cell carcinoma cases, leading to a 5-year survival rate lesser than 40% (174). Hsieh et al. showed that although compared to the placebo group, patients administered PG2 did not show any difference in their tumor response rate, disease-specific survival rate, or overall survival rate, their QOL was significantly improved as indicated by the reduction in pain and improvement in appetite (175) ( Table 6 ).
Table 6.
Clinical trials of APS'anti-tumor effect.
| Cancer type | Clinical Study Stage | Number of participants | Treatment plan | Dosage and treatment courses | Observation Results (↑upregulation, ↓downregulation) | REF |
|---|---|---|---|---|---|---|
| Lung cancer | Already on the market | 53 | Group 1: ICI treatment Group 2: ICI combined with PG2 |
500mg/d, 6 weeks (±2 weeks) | neutrophil-lymphocyte ratio↑ | (170) |
| Non-small cell lung cancer | Already on the market | 75 | Group 1: CIK therapy Group 2: CIK therapy combined with PG2 |
250mg/d, 10d | CD4+ cells↑, CD3+ cells↑, Symptom of Qi deficiency↓ | (171) |
| Non-small cell lung cancer | Already on the market | 80 | Group 1: Gefitinib Group 2: Gefitinib combined with PG2 |
250mg/d, 21d | CD4+ cells↑, CD3+ cells↑, CD4+/CD8+ cells↑ and adverse reaction rate↓ | (172) |
| Non-small cell lung cancer | Already on the market | 61 | Group 1: CT Group 2: CT combined with PG2 |
250mg/d, 10d | Myelosuppression rate↓ | (173) |
| Head and neck squamous cell carcinoma | Phase II clinical study | 17 | Group 1: CCRT Group 2: CCRT combined with PG2 |
500mg, tiw | adverse reaction rate↓, Pain relief and improved appetite | (175) |
ICI, Immune checkpoint inhibitors; CIK, Cytokine-induced killer cells; CT, Chemotherapy; CCRT, Concurrent chemoradiotherapy.
Although these results are encouraging, owing to the limited number of patients and the influence of other potential factors, more comprehensive research is needed to ensure the optimal use of APS and its clinical safety profile in cancer therapy.
3. Discussion
The rising morbidity and mortality due to cancer in recent years have posed a serious threat to human health; however, its pathogenesis has not been thoroughly understood. The effectiveness of existing therapies is limited, and complete tumor treatment is difficult. Radiotherapy and chemotherapy not only cause pain and reduce the QOL but also increase the economic burden on patients. Currently, effective agents with low toxicity and few side effects need to be explored for treatment or adjuvant therapy.
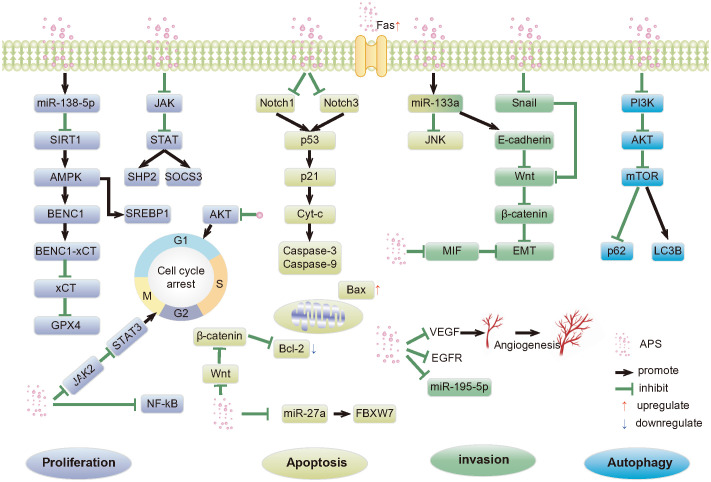
As a natural product, APS has high medicinal value. It has multi-pathway, multi-target, and multi-level anti-cancer mechanisms. These include inducing apoptosis; regulating tumor cell autophagy; inhibiting tumor cell proliferation, invasion, and metastasis; tumor-related inflammatory microenvironment; and synergism with anticancer drugs ( Figure 1 ). These mechanisms have broad research prospects, which warrant in-depth research.
Figure 1.
Anti-tumor pathways mediated by APS. APS, Astragalus polysaccharides; SIRT1, Silent mating type information regulation 2 homolog- 1; AMPK, Adenosine monophosphate activated protein kinase; SREBP1, Recombinant Sterol Regulatory Element Binding Transcription Factor 1; BECN1,Beclin-1; xCT, Light chain subunit SLC7A11; GPX4,Glutathione peroxidase 4; JAK, Janus kinase; STAT, Signal transducer of activators of transcription; SHP2, SH2 domain-containing protein tyrosine phosphatase 2; SOCS3, Suppressor of cy-tokine signaling proteins; AKT, Protein kinase B; NF-κB, Nuclear factor kappa-B; p53, p53 protein; p21, p21 protein; Cyt-c, Cytochrome c; Bcl-2, B-cell lymphoma-2; Bax, Bcl-2-associated X; FBXW7, F-box/WD repeat-containing protein 7; JNK, c-Jun N-terminal kinases; EMT, Epithelial-mesenchymal transition; MIF, Macrophage migration inhibitor factor; VEGF, Vascular endothelial growth factor; EGFR, Epidermal growth factor receptor; p63, p63 protein; PI3K, Phosphatidylinositol-3-kinase; mTOR, Mammalian rapamycin target protein; LC3B, Microtubule-associated protein 1 light chain 3 Beta.
Despite its promising benefits, the study of APS has some limitations. First, the potential mechanisms and causality of its active ingredients in complex cell signaling pathways are not comprehensively understood, and consistent models and evaluation criteria, particularly high-quality and large-sample clinical data, are lacking. Second, the literature survey showed that the APS dose used in related studies varied significantly. Therefore, the safe and effective dose of APS in follow-up studies should be determined, and a relatively safe regimen developed. Moreover, current research on APS is primarily limited to in vitro cell experiments and rodent models, and its optimal dose and safety need to be verified. Additionally, because APS is a hydrophilic macromolecular mixture, its bioavailability is low, and the combination of APS and nanocarriers can overcome this obstacle to achieve targeted drug delivery, effectively reduce drug dosage, and improve bioavailability. However, research on APS-modified nanocarriers to improve the specific targeting of tumor tissues is lacking.
In conclusion, APS has great potential in cancer therapy, particularly as nanoparticles obtained by APS processing. To establish the effectiveness of APS in clinical treatment and its broader anti-tumor mechanism and, thus, provide a more efficacious treatment for patients with cancer, further experimental exploration and research are essential.
Author contributions
QY: Writing – original draft, Investigation. DM: Investigation, Writing – review & editing. QZ: Project administration, Supervision, Writing – review & editing. JW: Data curation, Supervision, Writing – review & editing.
Glossary
| APS | Astragalus polysaccharides |
| Bcl-2 | B-cell lymphoma-2 |
| Bax | Bcl-2-associated X |
| HCC | Hepatocellular cancer |
| c-myc | Myelocytomatosis viral oncogene homolog |
| Cyclin D1 | G1/S-Specific cyclin-D1 |
| BC | Breast cancer |
| JNK | c-Jun N-terminal kinases |
| TNF | Tumor necrosis factor |
| JAK | Janus kinase |
| STAT | Signal transducer of activators of transcription |
| AKT | Protein kinase B |
| AMPK | Adenosine monophosphate activated protein kinase |
| BECN1 | Beclin-1 |
| GPX4 | Glutathione peroxidase 4 |
| xCT | Light chain subunit SLC7A11 |
| SIRT1 | Silent mating type information regulation 2 homolog- 1 |
| SREBP1 | Recombinant Sterol Regulatory Element Binding Transcription Factor 1 |
| SHP2 | SH2 domain-containing protein tyrosine phosphatase 2 |
| SOCS3 | Suppressor of cy-tokine signaling proteins |
| NF-κB | Nuclear factor kappa-B |
| EMT | Epithelial-mesenchymal transition |
| MIF | Macrophage migration inhibitor factor |
| PG2 | APS for injection |
| AXL | Recombinant AXL Receptor Tyrosine Kinase |
| NSCLC | Non-small cell lung cancer |
| VEGF | Vascular endothelial growth factor |
| EGFR | Epidermal growth factor receptor |
| HUVECs | Human umbilical vein endothelial cells |
| ROS | Reactive oxygen species |
| ∆Ψm | Mitochondrial membrane potential |
| CDDP | Cisplatin |
| PD-L1 | Programmed cell death protein-ligand 1 |
| PI3K | Phosphatidylinositol-3-kinase |
| P-gp | P-glycoprotein |
| MMP | Matrix metalloproteinase |
| OGT | O-GlcNAc transferase |
| OGA | O-GlcNAcase |
| ERK | Extracellular Regulated Protein Kinases |
| IL | Interleukin |
| DC | Dendritic Cells |
| iNOS | Inducible nitric oxide synthase |
| NO | Nitric oxide |
| TNF | Tumor necrosis facto |
| MDSCs | Myeloid-derived suppressor cells |
| CD | Cluster of Differentiation |
| HIF-1 | Hypoxia-inducible factor-1 |
| MSN | Moesin |
| mTOR | Mammalian rapamycin target protein |
| P70S6K | P70 ribosomal protein S6 kinase |
| LC3B | Microtubule-associated protein 1 light chain 3 Beta |
| Beclin1 | Bcl-2 interacting coiled-coil protein 1 |
| ICI | Immune checkpoint inhibitors |
| Cyt-c | Cytochrome c |
| CIK | Cytokine-induced killer cells |
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Ding Yuanqing National Famous Traditional Chinese Medicine Expert Inheritance Workshop.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. (2017) 3:524–48. doi: 10.1001/jamaoncol.2016.5688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 3. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. (2023) 73:17–48. doi: 10.3322/caac.21763 [DOI] [PubMed] [Google Scholar]
- 4. Yang Q, Chen Y, Guo R, Dai Y, Tang L, Zhao Y, et al. Interaction of Ncrna and epigenetic modifications in gastric cancer: focus on histone modification. Front Oncol. (2021) 11:822745. doi: 10.3389/fonc.2021.822745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cavalli G, Heard E. Advances in epigenetics link genetics to the environment and disease. Nature. (2019) 571:489–99. doi: 10.1038/s41586-019-1411-0 [DOI] [PubMed] [Google Scholar]
- 6. Nacev BA, Jones KB, Intlekofer AM, Yu JSE, Allis CD, Tap WD, et al. The epigenomics of sarcoma. Nat Rev Cancer. (2020) 20:608–23. doi: 10.1038/s41568-020-0288-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen Y, Long W, Yang L, Zhao Y, Wu X, Li M, et al. Functional peptides encoded by long non-coding Rnas in gastrointestinal cancer. Front Oncol. (2021) 11:777374. doi: 10.3389/fonc.2021.777374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Belli C, Trapani D, Viale G, D’Amico P, Duso BA, Della Vigna P, et al. Targeting the microenvironment in solid tumors. Cancer Treat Rev. (2018) 65:22–32. doi: 10.1016/j.ctrv.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 9. Xiang S, Li J, Shen J, Zhao Y, Wu X, Li M, et al. Identification of prognostic genes in the tumor microenvironment of hepatocellular carcinoma. Front Immunol. (2021) 12:653836. doi: 10.3389/fimmu.2021.653836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhao Q, Jiang Y, Xiang S, Kaboli PJ, Shen J, Zhao Y, et al. Engineered Tcr-T cell immunotherapy in anticancer precision medicine: pros and cons. Front Immunol. (2021) 12:658753. doi: 10.3389/fimmu.2021.658753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kakimi K, Karasaki T, Matsushita H, Sugie T. Advances in personalized cancer immunotherapy. Breast Cancer. (2017) 24:16–24. doi: 10.1007/s12282-016-0688-1 [DOI] [PubMed] [Google Scholar]
- 12. Pawłowska A, Suszczyk D, Okła K, Barczyński B, Kotarski J, Wertel I. Immunotherapies based on Pd-1/Pd-L1 pathway inhibitors in ovarian cancer treatment. Clin Exp Immunol. (2019) 195:334–44. doi: 10.1111/cei.13255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Solinas C, Aiello M, De Silva P, Gu-Trantien C, Migliori E, Willard-Gallo K. Targeting Pd-1 in cancer: biological insights with a focus on breast cancer. Crit Rev Oncol Hematol. (2019) 142:35–43. doi: 10.1016/j.critrevonc.2019.07.011 [DOI] [PubMed] [Google Scholar]
- 14. Zhang Y, Hou W, Lin H. Clinical research results and reflections on Tcm treatment of Malignant tumors. J Tradit Chin Med. (2014) 55:523–5. doi: 10.13288/j.11-2166/r.2014.06.021 [DOI] [Google Scholar]
- 15. Su HF, Shaker S, Kuang Y, Zhang M, Ye M, Qiao X. Phytochemistry and cardiovascular protective effects of Huang-Qi (Astragali Radix). Med Res Rev. (2021) 41:1999–2038. doi: 10.1002/med.21785 [DOI] [PubMed] [Google Scholar]
- 16. Zhang SY, Zhang J, Sun ZY, Chen XY, Xia TH, Yang SZ, et al. Effect of astragalus injection on the proliferation of hela cells in cervical cancer. Chin J Clin Pharmacol. (2020) 36:975–8. doi: 10.13699/j.cnki.1001-6821.2020.08.011 [DOI] [Google Scholar]
- 17. Li S, Sun Y, Huang J, Wang B, Gong Y, Fang Y, et al. Anti-tumor effects and mechanisms of astragalus membranaceus (Am) and its specific immunopotentiation: status and prospect. J Ethnopharmacol. (2020) 258:112797. doi: 10.1016/j.jep.2020.112797 [DOI] [PubMed] [Google Scholar]
- 18. Wu Y, Zhang X, Li Z, Yan H, Qin J, Li T. Formononetin inhibits human bladder cancer cell proliferation and invasiveness via regulation of Mir-21 and Pten. Food Funct. (2017) 8:1061–6. doi: 10.1039/C6FO01535B [DOI] [PubMed] [Google Scholar]
- 19. Zhang J, Liu L, Wang J, Ren B, Zhang L, Li W. Formononetin, an isoflavone from Astragalus membranaceus inhibits proliferation and metastasis of ovarian cancer cells. J Ethnopharmacol. (2018) 221:91–9. doi: 10.1016/j.jep.2018.04.014 [DOI] [PubMed] [Google Scholar]
- 20. Berezutsky MA, Durnova NA, Vlasova IA. [Experimental and clinical studies of mechanisms of the anti-aging effects of chemical compounds in astragalus membranaceus (Review).]. Adv Gerontol. (2019) 32:702–10. [PubMed] [Google Scholar]
- 21. Liu P, Zhao H, Luo Y. Anti-aging implications of Astragalus membranaceus (Huangqi): A well-known Chinese tonic. Aging Dis. (2017) 8:868–86. doi: 10.14336/ad.2017.0816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yu M, Shi J, Sheng M, Gao K, Zhang L, Liu L, et al. Astragalus inhibits epithelial-to-mesenchymal transition of peritoneal mesothelial cells by down-regulating B-catenin. Cell Physiol Biochem. (2018) 51:2794–813. doi: 10.1159/000495972 [DOI] [PubMed] [Google Scholar]
- 23. Huang P, Lu X, Yuan B, Liu T, Dai L, Liu Y, et al. Astragaloside iv alleviates E. Coli-caused peritonitis via upregulation of neutrophil influx to the site of infection. Int Immunopharmacol. (2016) 39:377–82. doi: 10.1016/j.intimp.2016.08.011 [DOI] [PubMed] [Google Scholar]
- 24. Liang Y, Zhang Q, Zhang L, Wang R, Xu X, Hu X. Astragalus membranaceus treatment protects Raw264.7 cells from influenza virus by regulating G1 phase and the Tlr3-mediated signaling pathway. Evid Based Complement Alternat Med. (2019) 2019:2971604. doi: 10.1155/2019/2971604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shang L, Qu Z, Sun L, Wang Y, Liu F, Wang S, et al. Astragaloside iv inhibits adenovirus replication and apoptosis in A549 cells in vitro . J Pharm Pharmacol. (2011) 63:688–94. doi: 10.1111/j.2042-7158.2011.01258.x [DOI] [PubMed] [Google Scholar]
- 26. Wen W, Chen J, Ding L, Luo X, Zheng X, Dai Q, et al. Astragaloside exerts anti-photoaging effects in Uvb-induced premature senescence of rat dermal fibroblasts through enhanced autophagy. Arch Biochem Biophys. (2018) 657:31–40. doi: 10.1016/j.abb.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 27. Tian QE, Li HD, Yan M, Cai HL, Tan QY, Zhang WY. Astragalus polysaccharides can regulate cytokine and P-glycoprotein expression in H22 tumor-bearing mice. World J Gastroenterol. (2012) 18:7079–86. doi: 10.3748/wjg.v18.i47.7079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li Y, Guo S, Zhu Y, Yan H, Qian DW, Wang HQ, et al. Comparative analysis of twenty-five compounds in different parts of Astragalus Membranaceus var. Mongholicus and Astragalus membranaceus by Uplc-Ms/Ms. J Pharm Anal. (2019) 9:392–9. doi: 10.1016/j.jpha.2019.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ma XQ, Shi Q, Duan JA, Dong TT, Tsim KW. Chemical analysis of Radix astragali (Huangqi) in China: A comparison with its adulterants and seasonal variations. J Agric Food Chem. (2002) 50:4861–6. doi: 10.1021/jf0202279 [DOI] [PubMed] [Google Scholar]
- 30. Guo Z, Lou Y, Kong M, Luo Q, Liu Z, Wu J. A systematic review of phytochemistry, pharmacology and pharmacokinetics on Astragali radix: implications for Astragali radix as a personalized medicine. Int J Mol Sci. (2019) 20:1463. doi: 10.3390/ijms20061463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fu J, Wang Z, Huang L, Zheng S, Wang D, Chen S, et al. Review of the botanical characteristics, phytochemistry, and pharmacology of Astragalus membranaceus (Huangqi). Phytother Res. (2014) 28:1275–83. doi: 10.1002/ptr.5188 [DOI] [PubMed] [Google Scholar]
- 32. Chang X, Chen X, Guo Y, Gong P, Pei S, Wang D, et al. Advances in chemical composition, extraction techniques, analytical methods, and biological activity of Astragali radix. Molecules. (2022) 27:1058. doi: 10.3390/molecules27031058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xie JH, Jin ML, Morris GA, Zha XQ, Chen HQ, Yi Y, et al. Advances on bioactive polysaccharides from medicinal plants. Crit Rev Food Sci Nutr. (2016) 56 Suppl 1:S60–84. doi: 10.1080/10408398.2015.1069255 [DOI] [PubMed] [Google Scholar]
- 34. Fan XH, Li K, Yang YD, Li HF, Li XQ, Qin XM. Research progress on structural characterization of astragalus polysaccharides. J Shanxi Univ Tradit Chin Med. (2022) 23:260–7. doi: 10.19763/j.cnki.2096-7403.2022.03.22 [DOI] [Google Scholar]
- 35. Liao J, Li C, Huang J, Liu W, Chen H, Liao S, et al. Structure characterization of honey-processed astragalus polysaccharides and its anti-inflammatory activity in vitro . Molecules. (2018) 23:168. doi: 10.3390/molecules23010168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dong N, Li X, Xue C, Zhang L, Wang C, Xu X, et al. Astragalus polysaccharides alleviates Lps-induced inflammation via the Nf-Kb/Mapk signaling pathway. J Cell Physiol. (2020) 235:5525–40. doi: 10.1002/jcp.29452 [DOI] [PubMed] [Google Scholar]
- 37. Meng Q, Du X, Wang H, Gu H, Zhan J, Zhou Z. Astragalus polysaccharides inhibits cell growth and pro-inflammatory response in Il-1β-stimulated fibroblast-like synoviocytes by enhancement of autophagy via Pi3k/Akt/Mtor inhibition. Apoptosis. (2017) 22:1138–46. doi: 10.1007/s10495-017-1387-x [DOI] [PubMed] [Google Scholar]
- 38. Liu QY, Yao YM, Yu Y, Dong N, Sheng ZY. Astragalus polysaccharides attenuate postburn sepsis via inhibiting negative immunoregulation of Cd4+ Cd25(High) T cells. PloS One. (2011) 6:e19811. doi: 10.1371/journal.pone.0019811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Li J, Bao Y, Lam W, Li W, Lu F, Zhu X, et al. Immunoregulatory and anti-tumor effects of polysaccharopeptide and astragalus polysaccharides on tumor-bearing mice. Immunopharmacol Immunotoxicol. (2008) 30:771–82. doi: 10.1080/08923970802279183 [DOI] [PubMed] [Google Scholar]
- 40. Zhang R, Xu L, An X, Sui X, Lin S. Astragalus Polysaccharides Attenuate Pulmonary fibrosis by Inhibiting the Epithelial-Mesenchymal transition and Nf-Kb Pathway Activation. Int J Mol Med. (2020) 46:331–9. doi: 10.3892/ijmm.2020.4574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu Y, Liu F, Yang Y, Li D, Lv J, Ou Y, et al. Astragalus polysaccharide ameliorates ionizing radiation-induced oxidative stress in mice. Int J Biol Macromol. (2014) 68:209–14. doi: 10.1016/j.ijbiomac.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 42. Li Q, Wang D, Bai D, Cai C, Li J, Yan C, et al. Photoprotective effect of Astragalus membranaceus polysaccharide on Uva-induced damage in Hacat cells. PloS One. (2020) 15:e0235515. doi: 10.1371/journal.pone.0235515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang Y, Chen SY, Yang ZM. Effect of astragalus polysaccharide on sweet taste receptor pathway in intestine of rat model induced by high-sugar and high-fat diet. Chin J Exp Tradit Med Form. (2019) 25:64–8. doi: 10.13422/j.cnki.syfjx.20191037 [DOI] [Google Scholar]
- 44. Chen W, Xia YP, Chen WJ, Yu MH, Li YM, Ye HY. Improvement of myocardial glycolipid metabolic disorder in diabetic hamster with astragalus polysaccharides treatment. Mol Biol Rep. (2012) 39:7609–15. doi: 10.1007/s11033-012-1595-y [DOI] [PubMed] [Google Scholar]
- 45. Chen W, Li YM, Yu MH. Astragalus polysaccharides inhibited diabetic cardiomyopathy in hamsters depending on suppression of heart chymase activation. J Diabetes Complications. (2010) 24:199–208. doi: 10.1016/j.jdiacomp.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 46. Zhang R, Qin X, Zhang T, Li Q, Zhang J, Zhao J. Astragalus polysaccharide improves insulin sensitivity via Ampk activation in 3t3-L1 adipocytes. Molecules. (2018) 23:2711. doi: 10.3390/molecules23102711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lai X, Xia W, Wei J, Ding X. Therapeutic effect of astragalus polysaccharides on hepatocellular carcinoma H22-bearing mice. Dose Response. (2017) 15:1559325816685182. doi: 10.1177/1559325816685182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhao L, Tan S, Zhang H, Liu P, Tan YZ, Li JC, et al. Astragalus polysaccharides exerts anti-infective activity by inducing human cathelicidin antimicrobial peptide Il-37 in respiratory epithelial cells. Phytother Res. (2018) 32:1521–9. doi: 10.1002/ptr.6080 [DOI] [PubMed] [Google Scholar]
- 49. Aglietti RA, Dueber EC. Recent insights into the molecular mechanisms underlying pyroptosis and gasdermin family functions. Trends Immunol. (2017) 38:261–71. doi: 10.1016/j.it.2017.01.003 [DOI] [PubMed] [Google Scholar]
- 50. Chui AJ, Okondo MC, Rao SD, Gai K, Griswold AR, Johnson DC, et al. N-terminal degradation activates the Nlrp1b inflammasome. Science. (2019) 364:82–5. doi: 10.1126/science.aau1208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chen XP. Status of anti-tumor research based on nonapoptotic programmed death. Chin J Pharmacol Toxicity. (2019) 33:896–7. [Google Scholar]
- 52. Warren CFA, Wong-Brown MW, Bowden NA. Bcl-2 family isoforms in apoptosis and cancer. Cell Death Dis. (2019) 10:177. doi: 10.1038/s41419-019-1407-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zhang L, Lu Z, Zhao X. Targeting Bcl-2 for cancer therapy. Biochim Biophys Acta Rev Cancer. (2021) 1876:188569. doi: 10.1016/j.bbcan.2021.188569 [DOI] [PubMed] [Google Scholar]
- 54. Fitzsimmons L, Cartlidge R, Chang C, Sejic N, Galbraith LCA, Suraweera CD, et al. Ebv Bcl-2 homologue Bhrf1 drives chemoresistance and lymphomagenesis by inhibiting multiple cellular pro-apoptotic proteins. Cell Death Differ. (2020) 27:1554–68. doi: 10.1038/s41418-019-0435-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jeng PS, Inoue-Yamauchi A, Hsieh JJ, Cheng EH. Bh3-dependent and independent activation of Bax and Bak in mitochondrial apoptosis. Curr Opin Physiol. (2018) 3:71–81. doi: 10.1016/j.cophys.2018.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Huang WH, Liao WR, Sun RX. Astragalus polysaccharide induces the apoptosis of human hepatocellular carcinoma cells by decreasing the expression of Notch1. Int J Mol Med. (2016) 38:551–7. doi: 10.3892/ijmm.2016.2632 [DOI] [PubMed] [Google Scholar]
- 57. Lv J, Zhu PF, Liu YM, Zeng QL, Yu ZJ. Astragalus polysaccharides downregulates apoptosis in Hepg2 cell through Wnt/B-catenin signaling pathway. Chin Tradit Herbal Drug. (2018) 49:5155–60. doi: 10.7501/j.issn.0253-2670.2018.21.029 [DOI] [Google Scholar]
- 58. Xie RD, Sun SB, He JX, Dong JN, Long F. Effect of astragalus polysaccharide on growth and tumor-related apoptosis protein of human breast cancer Mda-Mb-231 transplanted tumor in nude mice. Chin J Exp Tradit Med Form. (2019) 25:37–43. doi: 10.13422/j.cnki.syfjx.20191622 [DOI] [Google Scholar]
- 59. Stavast CJ, Erkeland SJ. The non-canonical aspects of micrornas: many roads to gene regulation. Cells. (2019) 8:1465. doi: 10.3390/cells8111465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Saliminejad K, Khorram Khorshid HR, Soleymani Fard S, Ghaffari SH. An overview of micrornas: biology, functions, therapeutics, and analysis methods. J Cell Physiol. (2019) 234:5451–65. doi: 10.1002/jcp.27486 [DOI] [PubMed] [Google Scholar]
- 61. Guo T, Zhang Y, Qu X, Che X, Li C, Fan Y, et al. Mir-200a enhances trail-induced apoptosis in gastric cancer cells by targeting A20. Cell Biol Int. (2018) 42:506–14. doi: 10.1002/cbin.10924 [DOI] [PubMed] [Google Scholar]
- 62. Lv J, Guo T, Qu X, Che X, Li C, Wang S, et al. Pd-L1 under regulation of Mir-429 influences the sensitivity of gastric cancer cells to trail by binding of Egfr. Front Oncol. (2020) 10:1067. doi: 10.3389/fonc.2020.01067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Xu K, Han B, Bai Y, Ma XY, Ji ZN, Xiong Y, et al. Mir-451a suppressing Bap31 can inhibit proliferation and increase apoptosis through inducing er stress in colorectal cancer. Cell Death Dis. (2019) 10:152. doi: 10.1038/s41419-019-1403-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ding L, Zhang S, Xu M, Zhang R, Sui P, Yang Q. Microrna-27a contributes to the Malignant behavior of gastric cancer cells by directly targeting Ph domain and leucine-rich repeat protein phosphatase 2. J Exp Clin Cancer Res. (2017) 36:45. doi: 10.1186/s13046-017-0516-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Luo W, Zhang D, Ma S, Wang C, Zhang Q, Wang H, et al. Mir-27a is highly expressed in H1650 cancer stem cells and regulates proliferation, migration, and invasion. J Cancer Res Ther. (2018) 14:S1004–s11. doi: 10.4103/0973-1482.199450 [DOI] [PubMed] [Google Scholar]
- 66. Maghsudlu M, Farashahi Yazd E, Amiriani T. Increased expression of Mir-27a and Mir-24-2 in esophageal squamous cell carcinoma. J Gastrointest Cancer. (2020) 51:227–33. doi: 10.1007/s12029-019-00232-x [DOI] [PubMed] [Google Scholar]
- 67. Guo Y, Zhang Z, Wang Z, Liu G, Liu Y, Wang H. Astragalus polysaccharides inhibit ovarian cancer cell growth via microrna-27a/Fbxw7 signaling pathway. Biosci Rep. (2020) 40:BSR20193396. doi: 10.1042/bsr20193396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Moradi S, Kamal A, Aboulkheyr Es H, Farhadi F, Ebrahimi M, Chitsaz H, et al. Pan-cancer analysis of microrna expression profiles highlights micrornas enriched in normal body cells as effective suppressors of multiple tumor types: A study based on Tcga database. PloS One. (2022) 17:e0267291. doi: 10.1371/journal.pone.0267291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kojima S, Chiyomaru T, Kawakami K, Yoshino H, Enokida H, Nohata N, et al. Tumour suppressors Mir-1 and Mir-133a target the oncogenic function of purine nucleoside phosphorylase (Pnp) in prostate cancer. Br J Cancer. (2012) 106:405–13. doi: 10.1038/bjc.2011.462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Li W, Chen A, Xiong L, Chen T, Tao F, Lu Y, et al. Mir-133a acts as a tumor suppressor in colorectal cancer by targeting Eif4a1. Tumour Biol. (2017) 39:1010428317698389. doi: 10.1177/1010428317698389 [DOI] [PubMed] [Google Scholar]
- 71. Chu Y, Fang Y, Chi J, Li J, Zhang D, Zou Y, et al. Astragalus Polysaccharides Decrease Proliferation, Migration, and Invasion but Increase Apoptosis of Human Osteosarcoma Cells by up-Regulation of Microrna-133a. Braz J Med Biol Res. (2018) 51:e7665. doi: 10.1590/1414-431x20187665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Riedl SJ, Salvesen GS. The apoptosome: signalling platform of cell death. Nat Rev Mol Cell Biol. (2007) 8:405–13. doi: 10.1038/nrm2153 [DOI] [PubMed] [Google Scholar]
- 73. MacKenzie SH, Clark AC. Targeting cell death in tumors by activating caspases. Curr Cancer Drug Targets. (2008) 8:98–109. doi: 10.2174/156800908783769391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Koren E, Fuchs Y. Modes of regulated cell death in cancer. Cancer Discovery. (2021) 11:245–65. doi: 10.1158/2159-8290.Cd-20-0789 [DOI] [PubMed] [Google Scholar]
- 75. Li H, Fan J, Zhao Y, Yang J, Xu H, Manthari RK, et al. Calcium alleviates fluoride-induced kidney damage via Fas/Fasl, Tnfr/Tnf, Dr5/trail pathways in rats. Ecotoxicol Environ Saf. (2021) 226:112851. doi: 10.1016/j.ecoenv.2021.112851 [DOI] [PubMed] [Google Scholar]
- 76. Müllauer L, Mosberger I, Grusch M, Rudas M, Chott A. Fas ligand is expressed in normal breast epithelial cells and is frequently up-regulated in breast cancer. J Pathol. (2000) 190:20–30. doi: 10.1002/(ISSN)1096-9896 [DOI] [PubMed] [Google Scholar]
- 77. Shimoyama M, Kanda T, Liu L, Koyama Y, Suda T, Sakai Y, et al. Expression of fas ligand is an early event in colorectal carcinogenesis. J Surg Oncol. (2001) 76:63–8; discussion 9. doi: [DOI] [PubMed] [Google Scholar]
- 78. Li CJ, Shen GH. Mechanism of astragalus polysaccharides promote colon cancer stem cell apoptosis byinducing autophagy. Chin J Tradit Chin Med Pharm. (2022) 37:2274–9. [Google Scholar]
- 79. Zhang C, Liu J, Xu D, Zhang T, Hu W, Feng Z. Gain-of-function mutant P53 in cancer progression and therapy. J Mol Cell Biol. (2020) 12:674–87. doi: 10.1093/jmcb/mjaa040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Zhang X, Qi Z, Yin H, Yang G. Interaction between P53 and Ras signaling controls cisplatin resistance via Hdac4- and Hif-1α-mediated regulation of apoptosis and autophagy. Theranostics. (2019) 9:1096–114. doi: 10.7150/thno.29673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Pan F, Lin X, Hao L, Wang T, Song H, Wang R. The critical role of ferroptosis in hepatocellular carcinoma. Front Cell Dev Biol. (2022) 10:882571. doi: 10.3389/fcell.2022.882571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Liebl MC, Hofmann TG. The role of P53 signaling in colorectal cancer. Cancers (Basel). (2021) 13:2125. doi: 10.3390/cancers13092125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Liu J, Zhang C, Wang X, Hu W, Feng Z. Tumor suppressor P53 cross-talks with trim family proteins. Genes Dis. (2021) 8:463–74. doi: 10.1016/j.gendis.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Zhang JX, Han YP, Bai C, Li Q. Notch1/3 and P53/P21 are a potential therapeutic target for Aps-induced apoptosis in non-small cell lung carcinoma cell lines. Int J Clin Exp Med. (2015) 8:12539–47. [PMC free article] [PubMed] [Google Scholar]
- 85. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. (2011) 144:646–74. doi: 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 86. Sun Y, Liu Y, Ma X, Hu H. The influence of cell cycle regulation on chemotherapy. Int J Mol Sci. (2021) 22:6923. doi: 10.3390/ijms22136923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Bonacci T, Emanuele MJ. Dissenting degradation: deubiquitinases in cell cycle and cancer. Semin Cancer Biol. (2020) 67:145–58. doi: 10.1016/j.semcancer.2020.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Liu HW, Chen QR, Xiong H, Zhu Y, Zuo L. Astragalus polysaccharides inhabits proliferation, migration and invasion of bladder cancer Umuc3 cells by regulating the Jak2/Stat3 signaling pathway. J Shanxi Med Univ. (2023) 11):1442–8. doi: 10.13753/j.issn.1007-6611.2023.11.002 [DOI] [Google Scholar]
- 89. Yu J, Dong XD, Jiao JS, Ji HY, Liu AJ. Antitumor and immunoregulatory activities of a novel polysaccharide from Astragalus membranaceus on S180 tumor-bearing mice. Int J Biol Macromol. (2021) 189:930–8. doi: 10.1016/j.ijbiomac.2021.08.099 [DOI] [PubMed] [Google Scholar]
- 90. Du F, Dong LJ. Mechanism of astragalus polysaccharide in inhibiting proliferation of human hepatocellular carcinoma cells. West China J Pharm Sci. (2020) 35:402–6. doi: 10.13375/j.cnki.wcjps.2020.04.012 [DOI] [Google Scholar]
- 91. Yan LJ, Hong T, Luo JH, Cao XM, Liu W, Gao Y, et al. Effect of Astragali radix polysaccharides on proliferation and apoptosis of human colon cancer cell line Sw620. Chin J Exp Tradit Med Form. (2017) 23:97–101. doi: 10.13422/j.cnki.syfjx.2017220097 [DOI] [Google Scholar]
- 92. Shehzad A, Lee YS. Molecular mechanisms of curcumin action: signal transduction. Biofactors. (2013) 39:27–36. doi: 10.1002/biof.1065 [DOI] [PubMed] [Google Scholar]
- 93. Xin P, Xu X, Deng C, Liu S, Wang Y, Zhou X, et al. The role of Jak/Stat signaling pathway and its inhibitors in diseases. Int Immunopharmacol. (2020) 80:106210. doi: 10.1016/j.intimp.2020.106210 [DOI] [PubMed] [Google Scholar]
- 94. Tong G, Wang X, Chen S, Jin Y. Astragalus polysaccharide inhibits the development of urothelial carcinoma by activating Ampk signaling to induce Benc1-Xct complex formation. Aging (Albany NY). (2023) 15:9438–52. doi: 10.18632/aging.205007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Guo S, Ma B, Jiang X, Li X, Jia Y. Astragalus polysaccharides inhibits tumorigenesis and lipid metabolism through Mir-138-5p/Sirt1/Srebp1 pathway in prostate cancer. Front Pharmacol. (2020) 11:598. doi: 10.3389/fphar.2020.00598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Li YQ. Regulation mechanism of astragalus polysaccharides on proliferation, migration and invasion of cervical cancer cells through Jak-Stat signaling pathway. MCH Care China. (2021) 36:1633–6. doi: 10.19829/j.zgfybj.issn.1001-4411.2021.07.054 [DOI] [Google Scholar]
- 97. Wu CY, Ke Y, Zeng YF, Zhang YW, Yu HJ. Anticancer activity of astragalus polysaccharide in human non-small cell lung cancer cells. Cancer Cell Int. (2017) 17:115. doi: 10.1186/s12935-017-0487-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Paul CD, Mistriotis P, Konstantopoulos K. Cancer cell motility: lessons from migration in confined spaces. Nat Rev Cancer. (2017) 17:131–40. doi: 10.1038/nrc.2016.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Taki M, Abiko K, Ukita M, Murakami R, Yamanoi K, Yamaguchi K, et al. Tumor immune microenvironment during epithelial-mesenchymal transition. Clin Cancer Res. (2021) 27:4669–79. doi: 10.1158/1078-0432.Ccr-20-4459 [DOI] [PubMed] [Google Scholar]
- 100. Kalluri R. Emt: when epithelial cells decide to become mesenchymal-like cells. J Clin Invest. (2009) 119:1417–9. doi: 10.1172/jci39675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Yang S, Sun S, Xu W, Yu B, Wang G, Wang H. Astragalus polysaccharide inhibits breast cancer cell migration and invasion by regulating epithelial−Mesenchymal transition via the Wnt/B−Catenin signaling pathway. Mol Med Rep. (2020) 21:1819–32. doi: 10.3892/mmr.2020.10983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Conroy H, Mawhinney L, Donnelly SC. Inflammation and cancer: macrophage migration inhibitory factor (Mif)–the potential missing link. Qjm. (2010) 103:831–6. doi: 10.1093/qjmed/hcq148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Hertelendy J, Reumuth G, Simons D, Stoppe C, Kim BS, Stromps JP, et al. Macrophage migration inhibitory factor - a favorable marker in inflammatory diseases? Curr Med Chem. (2018) 25:601–5. doi: 10.2174/0929867324666170714114200 [DOI] [PubMed] [Google Scholar]
- 104. Guda MR, Rashid MA, Asuthkar S, Jalasutram A, Caniglia JL, Tsung AJ, et al. Pleiotropic role of macrophage migration inhibitory factor in cancer. Am J Cancer Res. (2019) 9:2760–73. [PMC free article] [PubMed] [Google Scholar]
- 105. Funamizu N, Hu C, Lacy C, Schetter A, Zhang G, He P, et al. Macrophage migration inhibitory factor induces epithelial to mesenchymal transition, enhances tumor aggressiveness and predicts clinical outcome in resected pancreatic ductal adenocarcinoma. Int J Cancer. (2013) 132:785–94. doi: 10.1002/ijc.27736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Guo X, Xu S, Gao X, Wang J, Xue H, Chen Z, et al. Macrophage migration inhibitory factor promotes vasculogenic mimicry formation induced by hypoxia via Cxcr4/Akt/Emt pathway in human glioblastoma cells. Oncotarget. (2017) 8:80358–72. doi: 10.18632/oncotarget.18673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Liao CH, Yong CY, Lai GM, Chow JM, Cheng CF, Fang CL, et al. Astragalus polysaccharide (Pg2) suppresses macrophage migration inhibitory factor and aggressiveness of lung adenocarcinoma cells. Am J Chin Med. (2020) 48:1491–509. doi: 10.1142/s0192415x20500731 [DOI] [PubMed] [Google Scholar]
- 108. Calin GA, Croce CM. Microrna-cancer connection: the beginning of a new tale. Cancer Res. (2006) 66:7390–4. doi: 10.1158/0008-5472.Can-06-0800 [DOI] [PubMed] [Google Scholar]
- 109. Tao X, Zhang X, Feng F. Astragalus polysaccharide suppresses cell proliferation and invasion by up-regulation of Mir-195-5p in non-small cell lung cancer. Biol Pharm Bull. (2022) 45:553–60. doi: 10.1248/bpb.b21-00634 [DOI] [PubMed] [Google Scholar]
- 110. Zhang XX, Li WH, Chen XM, Liu QM. Study of astragalus polysaccharide inhibits the proliferation, invasion and migration of prostate cancer Du145 cells by up regulating Mir-133a. Chin J Clin Pharmacol. (2023) 39:395–9. doi: 10.13699/j.cnki.1001-6821.2023.03.021 [DOI] [Google Scholar]
- 111. Lawrence R, Watters M, Davies CR, Pantel K, Lu YJ. Circulating tumour cells for early detection of clinically relevant cancer. Nat Rev Clin Oncol. (2023) 20:487–500. doi: 10.1038/s41571-023-00781-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Feng X, Shi XMY. Correlations of recurrence of gastric cancer in patients after radical surgery with serum gastrointestinal hormones, vascular endothelial growth factors and serum anti-helicobacter pylori Igg antibody. J buon. (2020) 25:1476–81. [PubMed] [Google Scholar]
- 113. Liabeuf D, Oshima M, Stange DE, Sigal M. Stem cells, helicobacter pylori, and mutational landscape: utility of preclinical models to understand carcinogenesis and to direct management of gastric cancer. Gastroenterology. (2022) 162:1067–87. doi: 10.1053/j.gastro.2021.12.252 [DOI] [PubMed] [Google Scholar]
- 114. Zhang Y, Brekken RA. Direct and indirect regulation of the tumor immune microenvironment by Vegf. J Leukoc Biol. (2022) 111:1269–86. doi: 10.1002/JLB.5RU0222-082R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Zhao L, Zhong Y, Liang J, Gao H, Tang N. Effect of astragalus polysaccharide on the expression of Vegf and Egfr in mice with Lewis transplantable lung cancer. J Coll Physicians Surg Pak. (2019) 29:392–4. doi: 10.29271/jcpsp.2019.04.392 [DOI] [PubMed] [Google Scholar]
- 116. Tang YW, Li YT. Effects of astragalus polysaccharides on in vitro cell metastasis of Sgc7901 induced by non-contact co-cultured huvecs cells. Chin Tradit Pat Med. (2020) 42:887–92. doi: 10.3969/j.issn.1001-1528.2020.04.012 [DOI] [Google Scholar]
- 117. Jin M, Zhao K, Huang Q, Shang P. Structural features and biological activities of the polysaccharides from Astragalus membranaceus. Int J Biol Macromol. (2014) 64:257–66. doi: 10.1016/j.ijbiomac.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 118. Rosenthal R, Günzel D, Finger C, Krug SM, Richter JF, Schulzke JD, et al. The effect of chitosan on transcellular and paracellular mechanisms in the intestinal epithelial barrier. Biomaterials. (2012) 33:2791–800. doi: 10.1016/j.biomaterials.2011.12.034 [DOI] [PubMed] [Google Scholar]
- 119. Parhi P, Mohanty C, Sahoo SK. Nanotechnology-based combinational drug delivery: an emerging approach for cancer therapy. Drug Discovery Today. (2012) 17:1044–52. doi: 10.1016/j.drudis.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 120. Li X, Yu C, Meng X, Hou Y, Cui Y, Zhu T, et al. Study of double-targeting nanoparticles loaded with Mcl-1 Sirna and dexamethasone for adjuvant-induced arthritis therapy. Eur J Pharm Biopharm. (2020) 154:136–43. doi: 10.1016/j.ejpb.2020.07.009 [DOI] [PubMed] [Google Scholar]
- 121. Mal J, Veneman WJ, Nancharaiah YV, van Hullebusch ED, Peijnenburg WJ, Vijver MG, et al. A comparison of fate and toxicity of selenite, biogenically, and chemically synthesized selenium nanoparticles to zebrafish (Danio rerio) embryogenesis. Nanotoxicology. (2017) 11:87–97. doi: 10.1080/17435390.2016.1275866 [DOI] [PubMed] [Google Scholar]
- 122. Zhang J, Wang X, Xu T. Elemental selenium at nano size (Nano-se) as a potential chemopreventive agent with reduced risk of selenium toxicity: comparison with se-methylselenocysteine in mice. Toxicol Sci. (2008) 101:22–31. doi: 10.1093/toxsci/kfm221 [DOI] [PubMed] [Google Scholar]
- 123. Estevez H, Garcia-Lidon JC, Luque-Garcia JL, Camara C. Effects of chitosan-stabilized selenium nanoparticles on cell proliferation, apoptosis and cell cycle pattern in Hepg2 cells: comparison with other selenospecies. Colloids Surf B Biointerf. (2014) 122:184–93. doi: 10.1016/j.colsurfb.2014.06.062 [DOI] [PubMed] [Google Scholar]
- 124. Zhao S, Yu Q, Pan J, Zhou Y, Cao C, Ouyang JM, et al. Redox-responsive mesoporous selenium delivery of doxorubicin targets Mcf-7 cells and synergistically enhances its anti-tumor activity. Acta Biomater. (2017) 54:294–306. doi: 10.1016/j.actbio.2017.02.042 [DOI] [PubMed] [Google Scholar]
- 125. Jia X, Liu Q, Zou S, Xu X, Zhang L. Construction of selenium nanoparticles/B-glucan composites for enhancement of the antitumor activity. Carbohydr Polym. (2015) 117:434–42. doi: 10.1016/j.carbpol.2014.09.088 [DOI] [PubMed] [Google Scholar]
- 126. Sonkusre P, Cameotra SS. Biogenic selenium nanoparticles induce Ros-mediated necroptosis in Pc-3 cancer cells through Tnf activation. J Nanobiotechnol. (2017) 15:43. doi: 10.1186/s12951-017-0276-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Ji H, Lou X, Jiao J, Li Y, Dai K, Jia X. Preliminary structural characterization of selenium nanoparticle composites modified by astragalus polysaccharide and the cytotoxicity mechanism on liver cancer cells. Molecules. (2023) 28:1561. doi: 10.3390/molecules28041561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Jiao J, Yu J, Ji H, Liu A. Synthesis of macromolecular astragalus polysaccharide-nano selenium complex and the inhibitory effects on Hepg2 cells. Int J Biol Macromol. (2022) 211:481–9. doi: 10.1016/j.ijbiomac.2022.05.095 [DOI] [PubMed] [Google Scholar]
- 129. Duan Z, Liang M, Yang C, Yan C, Wang L, Song J, et al. Selenium nanoparticles coupling with astragalus polysaccharides exert their cytotoxicities in Mcf-7 cells by inhibiting autophagy and promoting apoptosis. J Trace Elem Med Biol. (2022) 73:127006. doi: 10.1016/j.jtemb.2022.127006 [DOI] [PubMed] [Google Scholar]
- 130. Huang QL, Shi MX, Wang JR, Qu D, Liu YP, Chen Y. Preparation and polarization activity research of astragalus polysaccharide-superparamagnetic iron oxide nanocomposite. Acta Pharm Sin. (2023) 58:779–88. doi: 10.16438/j.0513-4870.2022-1059 [DOI] [Google Scholar]
- 131. Tan DS, Miller RE, Kaye SB. New perspectives on molecular targeted therapy in ovarian clear cell carcinoma. Br J Cancer. (2013) 108:1553–9. doi: 10.1038/bjc.2013.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Gong Q, Yu H, Ding G, Ma J, Wang Y, Cheng X. Suppression of stemness and enhancement of chemosensibility in the resistant melanoma were induced by astragalus polysaccharide through pd-L1 downregulation. Eur J Pharmacol. (2022) 916:174726. doi: 10.1016/j.ejphar.2021.174726 [DOI] [PubMed] [Google Scholar]
- 133. Liu Y, Chen LY. Effect of astragalus polysaccharide on cisplatin resistance of human lung cancer A549/Ddp cells and its mechanism. J Jilin Univ Med Edit. (2020) 46:1162–8 + 348. doi: 10.13481/j.1671-587x.20200609 [DOI] [Google Scholar]
- 134. Lu QZ, Luo YY, Wang X, Zhang LL, Chen SH. Astragalus polysaccharide regulates cisplat in resistance in colorectal cancer cells through Mir-10b-5p/Ag Pat3 molecular axis. J Shenyang Pharm Univ. (2022) 39:970–8. doi: 10.14066/j.cnki.cn21-1349/r.2020.0982 [DOI] [Google Scholar]
- 135. Yang YL, Lin ZW, He PT, Nie H, Yao QY, Zhang SY. Inhibitory effect of astragalus polysaccharide combined with cisplatin on cell cycle and migration of nasopharyngeal carcinoma cell lines. Biol Pharm Bull. (2021) 44:926–31. doi: 10.1248/bpb.b20-00959 [DOI] [PubMed] [Google Scholar]
- 136. Li C, Hong L, Liu C, Min J, Hu M, Guo W. Astragalus polysaccharides increase the sensitivity of Skov3 cells to cisplatin. Arch Gynecol Obstet. (2018) 297:381–6. doi: 10.1007/s00404-017-4580-9 [DOI] [PubMed] [Google Scholar]
- 137. Li M, Duan F, Pan Z, Liu X, Lu W, Liang C, et al. Astragalus polysaccharide promotes doxorubicin-induced apoptosis by reducing O-glcnacylation in hepatocellular carcinoma. Cells. (2023) 12:866. doi: 10.3390/cells12060866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Wei J, Li Y, Xu B, Yu J. Astragalus polysaccharides reverse gefitinib resistance by inhibiting mesenchymal transformation in lung adenocarcinoma cells. Am J Transl Res. (2020) 12:1640–57. [PMC free article] [PubMed] [Google Scholar]
- 139. Bao WR, Li ZP, Zhang QW, Li LF, Liu HB, Ma DL, et al. Astragalus polysaccharide rap selectively attenuates paclitaxel-induced cytotoxicity toward Raw 264.7 cells by reversing cell cycle arrest and apoptosis. Front Pharmacol. (2018) 9:1580. doi: 10.3389/fphar.2018.01580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Wu J, Wang J, Su Q, Ding W, Li T, Yu J, et al. Traditional Chinese medicine astragalus polysaccharide enhanced antitumor effects of the angiogenesis inhibitor apatinib in pancreatic cancer cells on proliferation, invasiveness, and apoptosis. Onco Targets Ther. (2018) 11:2685–98. doi: 10.2147/ott.S157129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Liu Y, Cao X. Characteristics and significance of the pre-metastatic niche. Cancer Cell. (2016) 30:668–81. doi: 10.1016/j.ccell.2016.09.011 [DOI] [PubMed] [Google Scholar]
- 142. Du X, Zhao B, Li J, Cao X, Diao M, Feng H, et al. Astragalus polysaccharides enhance immune responses of Hbv DNA vaccination via promoting the dendritic cell maturation and suppressing Treg frequency in mice. Int Immunopharmacol. (2012) 14:463–70. doi: 10.1016/j.intimp.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 143. Bamodu OA, Kuo KT, Wang CH, Huang WC, Wu ATH, Tsai JT, et al. Astragalus polysaccharides (Pg2) enhances the M1 polarization of macrophages, functional maturation of dendritic cells, and T cell-mediated anticancer immune responses in patients with lung cancer. Nutrients. (2019) 11:2264. doi: 10.3390/nu11102264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Wei W, Li ZP, Bian ZX, Han QB. Astragalus polysaccharide rap induces macrophage phenotype polarization to M1 via the notch signaling pathway. Molecules. (2019) 24:2016. doi: 10.3390/molecules24102016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Li C, Pan XY, Ma M, Zhao J, Zhao F, Lv YP. Astragalus polysacharin inhibits hepatocellular carcinoma-like phenotypes in a murine Hcc model through repression of M2 polarization of tumour-associated macrophages. Pharm Biol. (2021) 59:1533–9. doi: 10.1080/13880209.2021.1991384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Li W, Song K, Wang S, Zhang C, Zhuang M, Wang Y, et al. Anti-tumor potential of astragalus polysaccharides on breast cancer cell line mediated by macrophage activation. Mater Sci Eng C Mater Biol Appl. (2019) 98:685–95. doi: 10.1016/j.msec.2019.01.025 [DOI] [PubMed] [Google Scholar]
- 147. Ding G, Gong Q, Ma J, Liu X, Wang Y, Cheng X. Immunosuppressive activity is attenuated by astragalus polysaccharides through remodeling the gut microenvironment in melanoma mice. Cancer Sci. (2021) 112:4050–63. doi: 10.1111/cas.15078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Yu J, Ji H, Yang Z, Liu A. Relationship between structural properties and antitumor activity of astragalus polysaccharides extracted with different temperatures. Int J Biol Macromol. (2019) 124:469–77. doi: 10.1016/j.ijbiomac.2018.11.156 [DOI] [PubMed] [Google Scholar]
- 149. He L, Xu K, Niu L, Lin L. Astragalus polysaccharide (Aps) attenuated pd-L1-mediated immunosuppression via the Mir-133a-3p/Msn axis in Hcc. Pharm Biol. (2022) 60:1710–20. doi: 10.1080/13880209.2022.2112963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Chang HL, Kuo YH, Wu LH, Chang CM, Cheng KJ, Tyan YC, et al. The extracts of Astragalus membranaceus overcome tumor immune tolerance by inhibition of tumor programmed cell death protein ligand-1 expression. Int J Med Sci. (2020) 17:939–45. doi: 10.7150/ijms.42978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Mashima T, Seimiya H, Tsuruo T. De novo fatty-acid synthesis and related pathways as molecular targets for cancer therapy. Br J Cancer. (2009) 100:1369–72. doi: 10.1038/sj.bjc.6605007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Menendez JA, Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer. (2007) 7:763–77. doi: 10.1038/nrc2222 [DOI] [PubMed] [Google Scholar]
- 153. Merino Salvador M, Gómez de Cedrón M, Moreno Rubio J, Falagán Martínez S, Sánchez Martínez R, Casado E, et al. Lipid metabolism and lung cancer. Crit Rev Oncol Hematol. (2017) 112:31–40. doi: 10.1016/j.critrevonc.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 154. Zaidi N, Lupien L, Kuemmerle NB, Kinlaw WB, Swinnen JV, Smans K. Lipogenesis and lipolysis: the pathways exploited by the cancer cells to acquire fatty acids. Prog Lipid Res. (2013) 52:585–9. doi: 10.1016/j.plipres.2013.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Pope ED, 3rd, Kimbrough EO, Vemireddy LP, Surapaneni PK, Copland JA, 3rd, Mody K. Aberrant lipid metabolism as a therapeutic target in liver cancer. Expert Opin Ther Targets. (2019) 23:473–83. doi: 10.1080/14728222.2019.1615883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Cheng L, Zhu Y, Han H, Zhang Q, Cui K, Shen H, et al. Microrna-148a deficiency promotes hepatic lipid metabolism and hepatocarcinogenesis in mice. Cell Death Dis. (2017) 8:e2916. doi: 10.1038/cddis.2017.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Yi M, Li J, Chen S, Cai J, Ban Y, Peng Q, et al. Emerging role of lipid metabolism alterations in cancer stem cells. J Exp Clin Cancer Res. (2018) 37:118. doi: 10.1186/s13046-018-0784-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Xu H, Zhou S, Tang Q, Xia H, Bi F. Cholesterol metabolism: new functions and therapeutic approaches in cancer. Biochim Biophys Acta Rev Cancer. (2020) 1874:188394. doi: 10.1016/j.bbcan.2020.188394 [DOI] [PubMed] [Google Scholar]
- 159. Yarla N, Madka V, Rao C. Targeting triglyceride metabolism for colorectal cancer prevention and therapy. Curr Drug Targets. (2022) 23:628–35. doi: 10.2174/1389450122666210824150012 [DOI] [PubMed] [Google Scholar]
- 160. Wang JY, Yuan YY, Zhang K, Sun X, Bu X, Dong J, et al. Ndrg2 inhibits tumorigenesis of hepatocellular carcinoma by regulating metabolism of phospholipids and triglyceride: A metabonomic analysis. J South Med Univ. (2022) 42:1765–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Zhuang Q, Ye X, Shen S, Cheng J, Shi Y, Wu S, et al. Astragalus polysaccharides ameliorate diet-induced gallstone formation by modulating synthesis of bile acids and the gut microbiota. Front Pharmacol. (2021) 12:701003. doi: 10.3389/fphar.2021.701003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Cheng Y, Tang K, Wu S, Liu L, Qiang C, Lin X, et al. Astragalus polysaccharides lowers plasma cholesterol through mechanisms distinct from statins. PloS One. (2011) 6:e27437. doi: 10.1371/journal.pone.0027437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. He C, Klionsky DJ. Regulation mechanisms and signaling pathways of autophagy. Annu Rev Genet. (2009) 43:67–93. doi: 10.1146/annurev-genet-102808-114910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Klionsky DJ, Abdel-Aziz AK, Abdelfatah S, Abdellatif M, Abdoli A, Abel S, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition)(1). Autophagy. (2021) 17:1–382. doi: 10.1080/15548627.2020.1797280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Yoshii SR, Mizushima N. Monitoring and measuring autophagy. Int J Mol Sci. (2017) 18:1865. doi: 10.3390/ijms18091865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Li X, He S, Ma B. Autophagy and autophagy-related proteins in cancer. Mol Cancer. (2020) 19:12. doi: 10.1186/s12943-020-1138-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Li XF, Chen DP, Ouyang FZ, Chen MM, Wu Y, Kuang DM, et al. Increased autophagy sustains the survival and pro-tumourigenic effects of neutrophils in human hepatocellular carcinoma. J Hepatol. (2015) 62:131–9. doi: 10.1016/j.jhep.2014.08.023 [DOI] [PubMed] [Google Scholar]
- 168. Zhi Q, Zhang N, Feng GL, Sun WY, Zhao YY, Yang SF. Study on the mechanism of astragalus polysaccharides regulating autophagy of colorectal cancer cells based on Pi3k/Akt/Mtor signaling pathway. Tianjin Med J. (2023) 51:240–5. doi: 10.11958/20220463 [DOI] [Google Scholar]
- 169. Chang MZ, Zhang SY, Hao YJ, Zhang SL, Zhang XL. Astragalus polysaccharide inhibits the proliferation of esophageal cancer ec109 cells by inducing cell autophagy. Cent South Pharm. (2022) 20:856–62. doi: 10.7539/j.issn.1672-2981.2022.04.021 [DOI] [Google Scholar]
- 170. Tsao SM, Wu TC, Chen J, Chang F, Tsao T. Astragalus polysaccharide injection (Pg2) normalizes the neutrophil-to-lymphocyte ratio in patients with advanced lung cancer receiving immunotherapy. Integr Cancer Ther. (2021) 20:1534735421995256. doi: 10.1177/1534735421995256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Zhang Y, Jia YJ, Li XJ, Wang L, Du MN, Zhang XX. Clinical observation on astragalus polysaccharide injection combined with Cik cells treating Nsclc patients with qi deficiency syndrome. Chin Tradit Herbal Drug. (2018) 49:1647–51. doi: 10.7501/j.issn.0253-2670.2018.07.024 [DOI] [Google Scholar]
- 172. Liu DL, Gao FF, Wang MM, Li HT. Effects of astragalus polysaccharide injection combined with gefitinib on immune function, quality of life and toxicity of advanced lung cancer. Modern J Integr Tradit Chin West Med. (2018) 27:4049–51. doi: 10.3969/j.issn.1008-8849.2018.36.016 [DOI] [Google Scholar]
- 173. Zheng ZP, Yang WB, Li N, Bai YJ, Xing SY, Shao Q, et al. Clinical observation on injection of astragalus polysaccharides protecting marrow suppression of non-small-cell lung cancer after chemotherapy. Chin Tradit Herbal Drugs. (2013) 44:208–9. doi: 10.7501/j.issn.0253-2670.2013.02.018 [DOI] [Google Scholar]
- 174. Gildener-Leapman N, Ferris RL, Bauman JE. Promising systemic immunotherapies in head and neck squamous cell carcinoma. Oral Oncol. (2013) 49:1089–96. doi: 10.1016/j.oraloncology.2013.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Hsieh CH, Lin CY, Hsu CL, Fan KH, Huang SF, Liao CT, et al. Incorporation of astragalus polysaccharides injection during concurrent chemoradiotherapy in advanced pharyngeal or laryngeal squamous cell carcinoma: preliminary experience of a phase II double-blind, randomized trial. J Cancer Res Clin Oncol. (2020) 146:33–41. doi: 10.1007/s00432-019-03033-8 [DOI] [PMC free article] [PubMed] [Google Scholar]