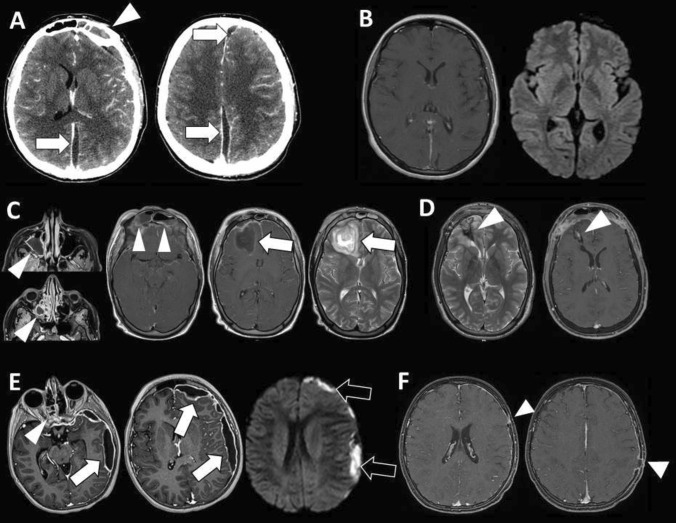
Fig. 2.
Case #1: left interhemispheric subdural empyema (A, arrows) complicating frontal sinusitis (A, arrowhead). The empyema was drained by two paramedian burr holes and the sinusitis by ENT toilette. S. intermedius was identified as responsible germ. Systemic antibiotic therapy cured the infection as confirmed by follow-up MR (B). Case #2: frontal abscess (C, arrow) complicating extensive sinusitis of the maxillary sinus, ethmoid cells, and frontal sinus (C, arrowheads). The lesion was surgical excised through bifrontal craniotomy with cranialization of the frontal sinus. Aspergillus fumigatus and Aspergillus niger were identified as responsible germs. Antimycotic treatment cured the infection with residual gliosis and minimal enhancement on follow-up MR (D, arrowheads). Case #3: sinusitis of the ethmoid cells (E, arrowhead) with left hemispheric subdural empyema (E, arrows) showing restriction on diffusion weighted image (E, black arrows). The empyema was drained by two burr holes and cured with wide spectrum systemic antibiotic therapy. Follow-up MR show the signs of the previous burr holes (F, arrowheads) with minimal residual dural enhancement on the left side