FIGURE 4.
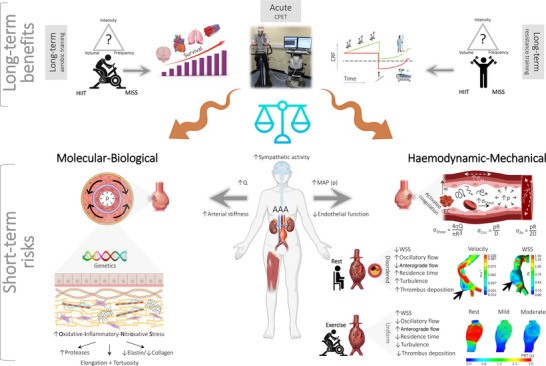
Vascular mechanobiological forces associated with exercise and risk of abdominal aortic aneurysm (AAA) rupture. Long‐term exercise is performed by AAA patients during the course of surgical prehabilitation and typically takes the form of submaximal to (supra)maximal high‐intensity interval training (HIIT). An acute incremental exercise trial to volitional exhaustion is also performed during cardiopulmonary exercise testing (CPET) to assess perioperative risk (Rose et al., 2022). Long‐term benefits: Long‐term moderate‐intensity continuous training (MICT) employing aerobic and/or resistance exercise is generally considered safe and well tolerated, assuming mean arterial pressure (mean aterial pressure (MAP) or pressure (p)) is controlled (see Section 6 Clinical Recommendations), with the capacity to elevate cardiorespiratory fitness (CRF) and improve peri‐operative outcome, including long‐term survival (Haque et al., 2022). Submaximal training in patients with occult small AAAs (3.0–5.5 cm) in the absence of aortic dissection/leak is advocated by respected authorities including, albeit not exclusively limited to, the American Heart Association/American College of Cardiology (Hirsch et al., 2006), Society for Vascular Surgery Practice Guidelines for AAA (Chaikof et al., 2009), Perioperative Exercise Testing and Training Society (Levett et al., 2018) and the American College of Sports Medicine. The American College of Sports Medicine advocates MICT for 20−40 min per session, 3−4 days per week, with an emphasis on duration rather than intensity (Myers, 2009). Short‐term risks: In contrast, concerns have been raised that acute, high(er)‐intensity exercise (notably CPET and potentially HIIT) could potentially tip the balance and precipitate AAA expansion and rupture, which is a catastrophic complication with untreated mortality approaching 100% (Myers et al., 2012; Perissiou et al., 2022). This is primarily attributable to the marked elevation in systemic pressurization combined with complex changes in aortic blood flow topology involving viscous and inertial forces that can adversely impact wall integrity by compounding existing molecular–biological (left) and haemodynamic–mechanical (right) risk factors. Note the complex flow–pressure–strain–shear stress phenotype, including the fundamental equations that govern mechanobiological forces to which endothelial cells in the AAA are exposed (right side). Blood flow (Q) in the healthy aorta is primarily unidirectional, laminar anterograde, with high wall shear stress (WSS). In the AAA, flow transitions to a more atherprone phenotype defined by turbulence, increased oscillatory shear stress (OSS) and lower WSS (Tanweer et al., 2014), accelerating oxidative–inflammatory–nitrosative stress (OXINOS)‐mediated structural degeneration of the adventitial wall, diametric expansion and mechanical rupture. Images inset right (modified from Boniforti et al., 2022) include patient‐specific computer tomography images of AAAs, highlighting regions of slow recirculation (longitudinal section) and low WSS (luminal surface) that coincided with the focal region of rupture (black arrows). Flow topology changes substantially with acute exercise owing to altered flow rate waveforms and elevations in Reynolds/Womersley numbers, with WSS increasing >6‐fold in the healthy aorta during moderate‐intensity exercise (50% elevation in heart rate) (Tang et al., 2006). Although calculation of the tensile stresses on the AAA wall and knowledge of corresponding stress failures are technically challenging, emergent evidence, using a combination of patient‐specific imaging and computational fluid dynamic modelling, suggests that acute exercise is atheroprotective owing to higher, more uniform mixing combined with an elevation in WSS and reciprocal reductions in OSS and particle residence time (PRT in mid‐diastole; see inset images modified from Suh et al., 2011) that normalize disordered (basal) flow mechanics (Arzani et al., 2014; Suh et al., 2011; Taylor et al., 1999). Abbreviations: D, diameter; R, radius; η, viscosity; σAx, axial stress; σCirc, circumferential stress.
