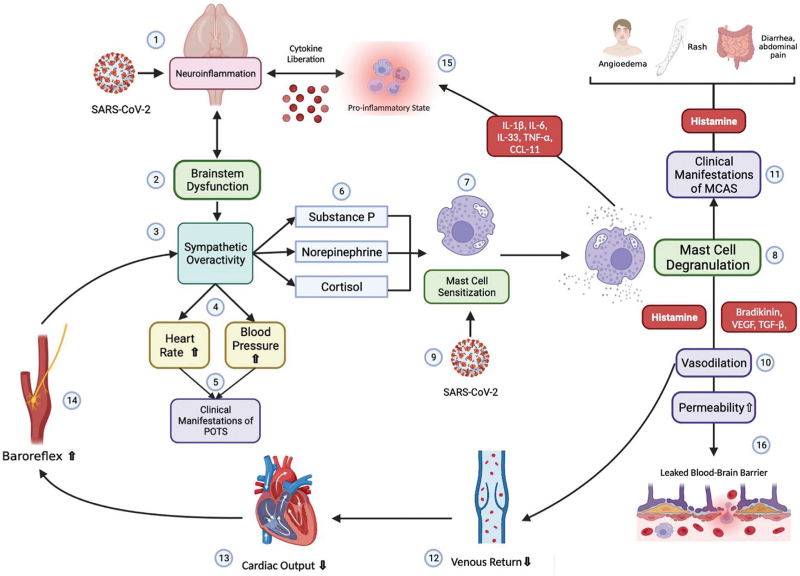
FIGURE 3.
Pathophysiology proposed modified from Shibao et al. The interaction of SARS-CoV-2 directly in the brainstem (1) could evoke an inflammatory response, causing brainstem dysfunction (2) manifested with sympathetic overactivity (3). Sympathetic activity will increase heart rate and blood pressure (4) giving place to clinical manifestations of POTS (5). Substance P, norepinephrine and cortisol will be released (6), sensitizing mast cells (7) and causing mast cell degranulation (8). In addition, direct interaction between SARS-CoV-2 and mast cells could enhance sensitization (9). Mast cell mediators (histamine, bradykinin, VEGF and TGF-β) will produce vasodilation (10) and clinical manifestations typical from MCAS (11). Vasodilation will provoke diminished venous return (12) and cardiac output (13), which will be sensed by the baroreceptors within the aorta and carotid artery, activating the baroreflex (14) resulting in more sympathetic activity (3). Mast cell mediators will potentiate a pro-inflammatory state (15) which along with augmented permeability, that can leak the blood–brain barrier (16), can perpetuate brainstem dysfunction (2).