Abstract
Introduction and importance:
Right middle lobe syndrome (MLS) is a rare lung disorder primarily affecting children with a history of asthma or atopy. It encompasses a range of pathological and clinical conditions, from recurrent collapses of the middle lobe to bronchiectasis. In this study, the authors present a case series featuring four individuals with MLS associated with asthma, aiming to deepen our understanding of this uncommon condition.
Case presentation:
Four paediatric patients with right MLS exhibited symptoms of persistent cough, dyspnoea, and recurrent asthma exacerbations. Radiographic evaluations confirmed features consistent with right MLS, and bronchoscopy revealed mucus plugs and oedematous airways obstructing the right middle lobe bronchus. Treatment with bronchodilators, antibiotics, and corticosteroids led to symptom improvement and resolution of atelectasis.
Clinical discussion:
MLS is a rare condition characterized by chronic collapse of the right middle lobe and bronchiectasis. It is challenging to diagnose MLS, but computed tomography (CT) scans provide detailed lung images for confirmation. Treatment focuses on addressing the underlying cause, such as infections or mucus obstruction. Lobectomy may be considered in severe cases. This case series emphasizes the need for further research on MLS, as its rarity and characteristics remain unclear.
Conclusion:
These cases exhibited obstructive MLS with and without asthma. Accurate diagnosis is challenging, requiring imaging techniques. MLS has clinical implications, particularly in asthma patients. Future studies should focus on understanding the aetiology of non-obstructive MLS.
Keywords: asthma, case series, paediatric, right middle lobe syndrome, right middle lobe
Introduction
Highlights
Our case series sheds light on the association between asthma and right middle lobe syndrome (MLS), revealing the clinical significance of this relationship.
The successful treatment of obstructive MLS in our cases with bronchodilators, antibiotics, and corticosteroids resulted in significant improvement in symptoms.
Further research is necessary to better understand the rarity and characteristics of MLS, particularly the non-obstructive type.
Right middle lobe syndrome (MLS) is a rare lung disorder that has been poorly defined in the literature. It involves the right middle lobe and/or lingula and comprises a spectrum of pathological and clinical lesions stretching from recurrent collapses of the middle lobe of the lung or pneumonitis to bronchiectasis. This condition predominantly affects children and most commonly those with a history of asthma or atopy1. The epidemiology of MLS is not well understood, but it occurs in children and adults of both sexes, in both primary and tertiary care settings2. MLS is not commonly observed in asthma patients with an incidence of 5–10% of MLS in children hospitalized with acute asthma3,4.
MLS is a term attributed to a long-term atelectasis occurring when the middle lobe of the lung shrinks. The most common cause of MLS is the pressure on the bronchial airway caused by a tumour or enlarged lymph nodes resulting in obstruction and congestion5. Thus, this leads to chronic inflammation, bronchiectasis, recurrent pneumonia and scarring6. With this relative isolation of the middle lobe and poor collateral ventilation, the chance of reinflation decreases. This atelectasis thus causes alveolar hypoxia and pulmonary vasoconstriction resulting in intrapulmonary shunting7. MLS was initially described by Graham et al.2,8. It is widely recognized to involve two distinct pathophysiological mechanisms, obstructive and non-obstructive, leading to repeated collapses of the middle lobe1. The obstructive type includes an extrinsic compression of the right middle lobe such as tumours (one-fourth of the cases) or non-neoplastics compressions. It may also be due to an endotracheal lesion or peribronchial lymph nodes enlargement caused by granulomatous infections (histoplasmosis, sarcoidosis, or metastases). On the other hand, the non-obstructive type comprises the majority of MLS individuals. It happens with an intact right middle lobe bronchus or lingula of the left upper lobe in adults and children with recurrent pneumonia and is associated frequently with asthma, bronchitis and cystic fibrosis1.
Individuals with MLS commonly experience a combination of symptoms, including chest pain, persistent cough, copious sputum, hemoptysis, dyspnoea, and signs of recurrent pneumonia with chronic cough and sputum being the most common presenting symptom and hemoptysis the least common9.
To enhance our understanding of this rare ailment and since the paucity of the literature on the subject makes it challenging to diagnose and manage the condition, we present a case series comprising four cases that underscore the manifestation of right MLS associated with asthma.
The work has been reported in line with the PROCESS criteria10.
Case presentation
Case 1
A 28-month-old male presented to the pulmonary clinic with a history of a productive cough that persisted for a week despite inhaler treatment. His past medical history was significant for eczema and asthma, and he was treated with inhaled corticosteroids and short-acting beta-agonists. The patient appeared alert and cooperative on clinical examination, and revealed a right sided expiratory wheeze with normal vital signs. Laboratory tests were unremarkable except for an elevated immunoglobulin E level. The patient’s weight and height were normal for his age. The sweat chloride test and skin test for tuberculosis were negative. A chest X-ray (Fig. 1) revealed a right basal infiltration with loss of cardiac silhouette, suggestive of right MLS. A chest computed tomography (CT) scan confirmed the presence of MLS and showed atelectasis of the right middle lobe (RML) and a trapezoidal opacity contiguous with the right cardiac border (Fig. 2). A bronchoscopy was performed, revealing a mucus plug in the right middle lobe bronchus, which was removed (Fig. 3). Bronchoalveolar lavage was performed and the cytological test and bacterial cultures were negative. Short-acting beta-agonists (albuterol) and antibiotics were initiated along with physical therapy. Two months after diagnosis, follow-up chest X-rays were normal (Fig. 4). The patient is currently receiving adjuvant treatment with bronchodilators and has shown an excellent response.
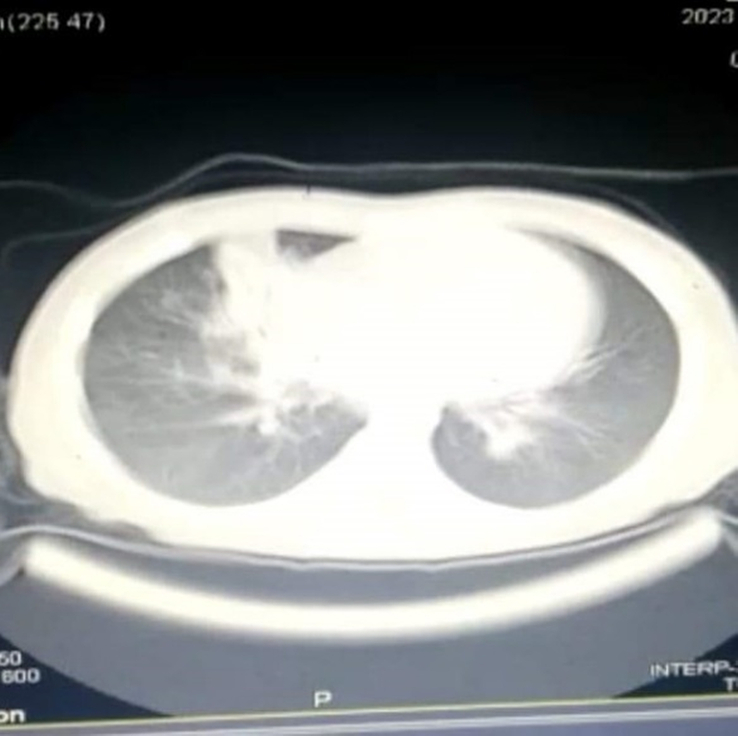
Figure 1.
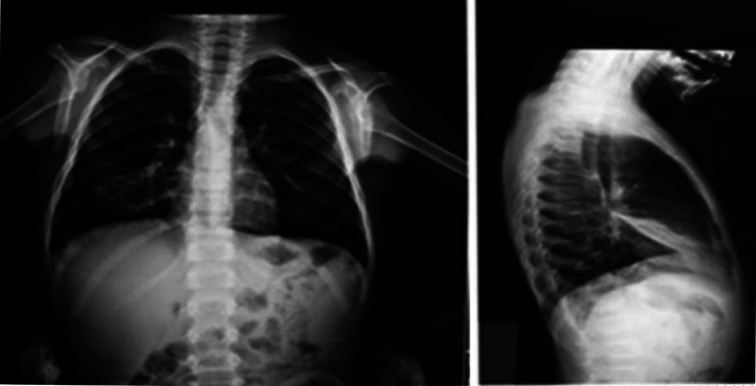
A chest X-ray showing a right basal infiltration with loss of cardiac silhouette.
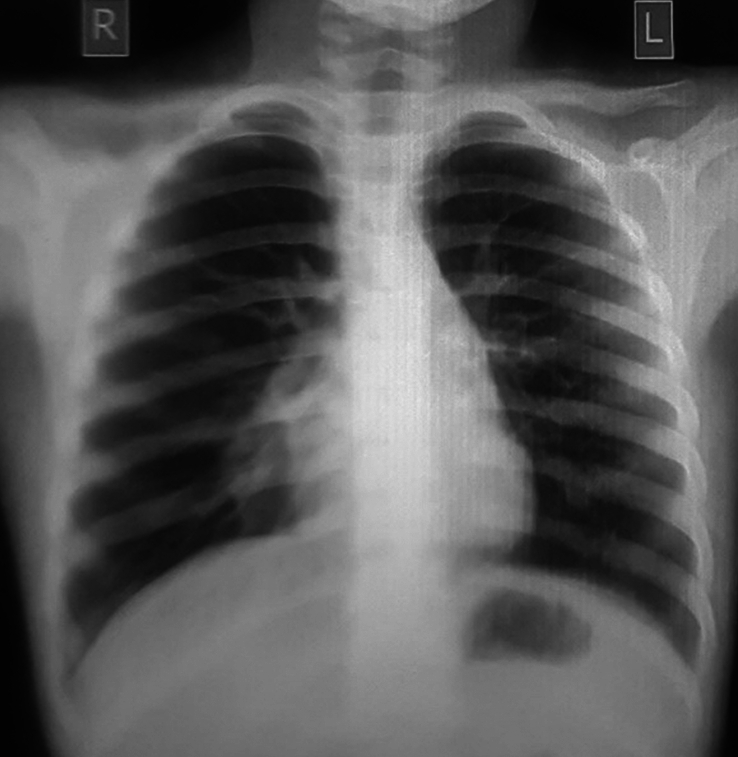
Figure 2.
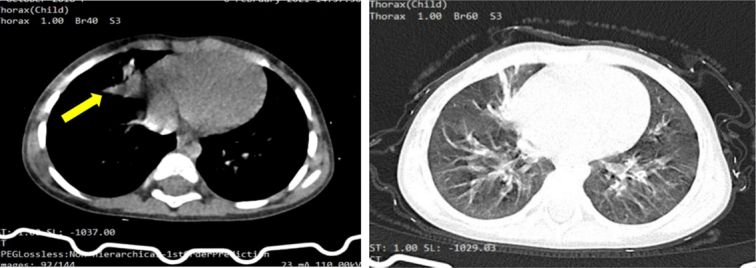
A computed tomography scan revealing atelectasis of the right middle lobe and a trapezoidal opacity contiguous with the right cardiac border.
Figure 3.
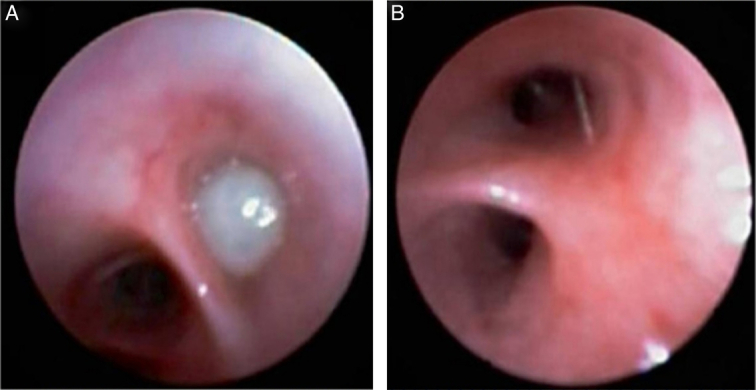
(A) A bronchoscopy revealed a mucus plug in the right middle lobe bronchus. (B) After removing the mucus plug.
Figure 4.
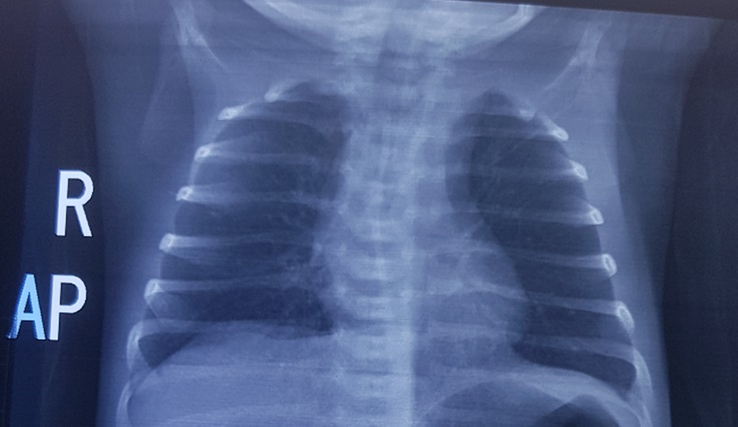
A normal follow-up chest X-rays.
Case 2
A 19-month-old female presented to the pulmonary clinic with mild dyspnoea, substernal traction, and a productive cough of purulent sputum intermittently for 2 weeks. Her past medical history was significant for two frequent pneumonias managed in the hospital. No fever was noticed during these events. On physical examination, there was diffuse mild wheezing. The patient’s height and weight were normal for her age. Laboratory tests were normal. A chest X-ray showed a right basal infiltration clouding the right edge of the heart (Fig. 5), suggestive of right MLS. A CT scan confirmed the presence of MLS and revealed atelectasis of the superior segment of the RML (Fig. 6). Treatment with inhaled corticosteroids and short-acting beta-agonists (albuterol) did not improve the clinical symptoms or radiographic evidence of atelectasis. Bronchoscopy was performed, and the airways were normal, except for the superior segment of the RML, where the airway was oedematous with a partially blocking thick plug. The secretions were suctioned and BAL was performed. The cytological test and bacterial cultures were negative. A post-procedure chest X-ray revealed the absence of RML atelectasis. Bronchodilators (albuterol) and antibiotics were started with physical therapy. After 3 months, the symptoms resolved, and the chest X-ray returned to normal (Fig. 7).
Figure 5.

A chest X-ray showed a right basal infiltration clouding the right edge of the heart.
Figure 6.
A computed tomography scan revealed atelectasis of the superior segment of the right middle lobe.
Figure 7.

A normal chest X-ray on follow-up.
Case 3
A 10-year-old male with a history of asthma diagnosed at the age of 4 years and treated with inhaled corticosteroids and albuterol presented with recurrent and uncontrolled asthma associated with persistent cough and sputum production for 2 weeks. Physical examination revealed the patient was alert with normal vital signs. Chest auscultation revealed diffuse mild wheezing and fine crackles without retraction. The patient’s height and weight were normal for their age. Laboratory tests and pulmonary function tests (PFTs) were normal. A chest X-ray (Fig. 8) revealed triangular atelectasis clouding the right edge of the heart suggesting right MLS. In addition, a CT scan (Fig. 9) revealed atelectasis of the RML confirming thus the diagnosis. Bronchoscopy revealed a mucus plug obstructing the RML bronchus which was removed. Treatment with bronchodilators, antibiotics, and corticosteroids was well-tolerated and follow-up PFT and chest X-ray images (Fig. 10) demonstrated complete disappearance of the atelectasis 2 months after diagnosis.
Figure 8.
A chest X-ray revealed triangular atelectasis clouding the right edge of the heart.
Figure 9.
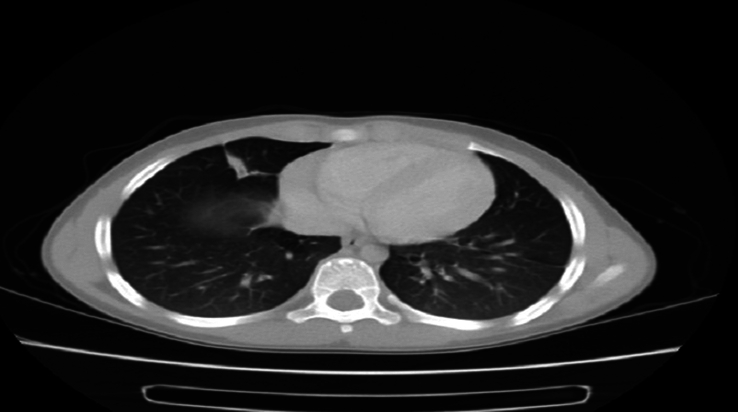
A computed tomography scan revealed atelectasis of the right middle lobe.
Figure 10.

A normal chest X-ray after treatment and follow-up.
Case 4
A 5-year-old male presented to the clinic due to persistent cough and dyspnoea for the last 3 months. He was first hospitalized for asthma at the age of 4 years and treated with inhaled corticosteroids and albuterol. He presented back then with frequent pneumonias which were managed in the hospital three times with a good response to treatment. On admission, the patient was alert, and chest auscultation revealed severe diffuse wheezing, prolonged expiration, and slight intercostal retraction. The patient’s height and weight were normal. Laboratory tests and PFTs were normal. A chest X-ray (Fig. 11) revealed triangular atelectasis clouding the right edge of the heart suggesting right MLS. A CT scan was not performed due to technical problems in the hospital. Bronchoscopy was performed showing a red and oedematous bronchus, and BAL was performed. The cytological test and bacterial cultures were negative. The patient was treated with bronchodilators and antibiotics and received physical therapy with good improvement. Follow-up chest x-ray (Fig. 12) and PFT 2 months after diagnosis were normal. The patient is currently receiving asthmatic treatment with an excellent response.
Figure 11.

A chest X-ray revealed triangular atelectasis clouding the right edge of the heart.
Figure 12.

The follow-up chest X-ray, showed the good improvement.
Discussion
MLS is a relatively uncommon condition that affects the right middle lobe and/or left lingula of the lung. It is characterized by chronic collapse of the middle lobe and bronchiectasis, a condition where the airways in the lungs become damaged and widened11. The RML and lingula are particularly susceptible to this syndrome due to poor collateral ventilation caused by their anatomical features, including the relatively narrow and long RML bronchus, sharp take-off angle, deep fissures with scanty parenchymal bridges, and poor development of the pores of Kohn and canals of Lambert7. Despite its clinical significance, there is limited epidemiological data on MLS, and only a few case series and nationwide studies have been conducted on the condition. Previous studies have indicated a higher female to male ratio in MLS patients, with women tending to present at a later age than men12,13. While some patients have several anatomical factors making the middle lobe susceptible to collapse14–17, others have mucus hypersecretion worsening thus the condition. This is frequent in children having asthma, cystic fibrosis or ciliary dyskinesia which in all cases cause airway inflammation, periciliary fluid outflow obstruction, and lowered action of surfactants raising the likelihood of bronchial collapse18,19. However, in this case series, we present three cases of male and one female, highlighting the need for more studies to draw definitive conclusions regarding the rarity and characteristics of this syndrome.
MLS is typically divided into two categories: obstructive and non-obstructive. The obstructive type is characterized by a blockage in the airway, while the non-obstructive type involves a clear right middle bronchus20. In our four cases, all patients exhibited the obstructive type, with mucus obstructing the bronchus. Cases 1, 3, and 4 were associated with asthma, while case 2 had a history of bronchiolitis, which is a major risk factor for developing asthma later in life21. Asthma with recurrent MLS may represent a clinically significant phenotype, as these children are at a greater risk of severe asthma and exacerbations. MLS is not commonly observed in asthma patients as the incidence reported by previous studies ranges between 5 and 10%3,4. The etiologies lying behind obstructed MLS include enlarged peribronchial lymph nodes, cardiovascular anomalies, inspissated mucus as in our four cases, and aspirated foreign bodies, particularly in children. On the other hand, the aetiology of the non-obstructive form is not fully understood, but inefficient collateral ventilation, infection, and inflammation in the middle lobe or lingula, along with bronchiectasis, are thought to play a role1,20.
Symptoms of MLS syndrome usually develop gradually. As reported in previous studies, main symptoms include chronic cough, purulent sputum production, unintentional weight loss, fever, lethargy, hemoptysis, chest pain, and night sweats20. In our cases, all of them presented with a productive cough, case 2 was associated with dyspnoea and substernal traction, and case 4 was associated with dyspnoea and frequent pneumonias. The severity of MLS in children can vary greatly, ranging from mild atelectasis and scarring that do not cause significant problems to severe bronchiectasis that requires surgical removal22.
Diagnosing MLS syndrome can be challenging. A postero-anterior and lateral plain chest X-ray may be the initial imaging study performed, but it may not be sufficient for a definitive diagnosis. In our fourth case, the chest X-ray showed a triangular atelectasis clouding the right edge of the heart, suggesting the disease, and bronchoscopy was subsequently performed. CT scan is often used to confirm the diagnosis of MLS syndrome, as it provides more detailed images of the lungs, which was done in our first three cases7.
The treatment of MLS syndrome is directed towards addressing the underlying cause. In cases where an infection is the cause, antibiotics may be prescribed to treat the infection effectively. Bronchodilators may also be used to help open up the airways and improve breathing. Postural drainage, a technique that involves positioning the body to facilitate mucus drainage from the lungs, may be recommended to help clear the airways7,23. Lobectomy of the right middle lobe has been identified as a viable therapeutic option for patients with MLS24. In our case series, medical treatment was initially attempted to alleviate symptoms before considering surgery, and bronchoscopy played a vital role as an important diagnostic and treatment procedure being an important diagnostic tool with a low complication rate in children8,25.
Conclusion
In conclusion, MLS is a relatively rare condition characterized by chronic collapse of the middle lobe and bronchiectasis. The right middle lobe and left lingula are particularly susceptible to this syndrome due to poor collateral ventilation resulting from their anatomical features. There is limited epidemiological data on MLS, and further studies are needed to fully understand the rarity and characteristics of this syndrome. MLS can be categorized into obstructive and non-obstructive types. In our cases, all patients exhibited the obstructive type and in association with asthma, with mucus obstructing the bronchus. Asthma with recurrent MLS is clinically significant, increasing the risk of severe symptoms and exacerbations. The aetiology of non-obstructive MLS remains unclear, emphasizing the importance of future research in this area. Diagnosing MLS can be challenging, and imaging techniques such as chest X-rays and CT scans are instrumental in confirming the diagnosis.
Ethics approval
Ethics approval was not required for this case report at our institution Faculty of Medicine at Damascus University, Damascus, Syria.
Consent
Informed consent was obtained from all patients’ legally authorized representatives. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
Not applicable.
Author contribution
E.S. is the first author, contributed to drafting, reviewing and editing. A.A.N. contributed to drafting, reviewing, and editing, and corresponding. H.H. contributed to drafting, reviewing, and editing, and bibliography. A.J. contributed to drafting, reviewing and editing. A.J. contributed to drafting, reviewing and editing. Z.N. contributed to drafting, reviewing and editing. S.A. contributed to reviewing, editing, and supervising All authors read and approved the final manuscript.
Conflicts of interest disclosure
The authors declare that they have no competing interests.
Research registration unique identifying number (UIN)
This study is a case report, so we can't make the registration it as a trial.
Guarantor
Sawssan Ali.
Data availability statement
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Eman Shhada, Email: eman91shhada2511@gmail.com.
Ali Alakbar Nahle, Email: Ali.AlAkbar.Nahle2001@gmail.com.
Hussein Hamdar, Email: Hussein_hamdar14@hotmail.com.
Alaa Jlailati, Email: alaajl155@gmail.com.
Ali Jawad, Email: dr.alijwd@gmail.com.
Zeinab Nahle, Email: zeinab.nahle@lau.edu.
Sawssan Ali, Email: Dr.sawssanali@gmail.com.
References
- 1.Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: a review of clinicopathological features, diagnosis and treatment. Respiration 2012;84:80–86. [DOI] [PubMed] [Google Scholar]
- 2.Graham EA, Burford TH, Mayer JH. Middle lobe syndrome. Postgrad Med 1948;4:29–34. [DOI] [PubMed] [Google Scholar]
- 3.Eggleston PA, Ward BH, Pierson WE, et al. Radiographic abnormalities in acute asthma in children. Pediatrics 1974;54:442–449. [PubMed] [Google Scholar]
- 4.Luhr J. Atelectasis with asthma in children. Nord Med 1958;60:1198–1199. [PubMed] [Google Scholar]
- 5.Aryana WF, Saputra TT, Wibowo A. Middle lobe syndrome. Jurnal Kedokteran Universitas Lampung 2023;7:14–17. [Google Scholar]
- 6.Sehitogullari A, Sayir F, Cobanoglu U, et al. Surgical treatment of right middle lobe syndrome in children. Ann Thorac Med 2012;7:8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romagnoli V, Priftis KN, de Benedictis FM. Middle lobe syndrome in children today. Paediatr Respir Rev 2014;15:188–193. [DOI] [PubMed] [Google Scholar]
- 8.Livingston GL, Holinger LD, Luck SR. Right middle lobe syndrome in children. Jijopo 1987;13:11–23. [DOI] [PubMed] [Google Scholar]
- 9.Meteroğlu F, Şahin A, Eren T. Middle lobe syndrome: a retrospective analysis. Turkish J Thorac Cardiovasc. Surg 2013;21:718–722. [Google Scholar]
- 10.Mathew G, Sohrabi C, Franchi T, et al. Preferred Reporting Of Case Series in Surgery (PROCESS) 2023 guidelines. Int J Surg 2023;109:3760–3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaikhrezai K, Khorsandi M, Zamvar V. Middle lobe syndrome associated with major haemoptysis. J Cardiothorac Surg 2013;8:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwon KY, Myers JL, Swensen SJ, et al. Middle lobe syndrome: a clinicopathological study of 21 patients. Hum Pathol 1995;26:302–307. [DOI] [PubMed] [Google Scholar]
- 13.Einarsson JT, Einarsson JG, Isaksson H, et al. Middle lobe syndrome: a nationwide study on clinicopathological features and surgical treatment. Clin Respir J 2009;3:77–81. [DOI] [PubMed] [Google Scholar]
- 14.Paulson DL, Shaw RR. Chronic atelectasis and pneumonitis of the middle lobe. J Thorac Surg 1949;18:747–760. [PubMed] [Google Scholar]
- 15.Culiner MM. The right middle lobe syndrome, a non-obstructive complex. Dis Chest 1966;50:57–66. [DOI] [PubMed] [Google Scholar]
- 16.Ayed AK. Resection of the right middle lobe and lingula in children for middle lobe/lingula syndrome. Chest 2004;125:38–42. [DOI] [PubMed] [Google Scholar]
- 17.Inners CR, Terry PB, Traystman RJ, et al. Collateral ventilation and the middle lobe syndrome. Am Rev Respir Dis 1978;118:305–310. [DOI] [PubMed] [Google Scholar]
- 18.Springer C, Avital A, Noviski N, et al. Role of infection in the middle lobe syndrome in asthma. Arch Dis Child 1992;67:592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sekerel BE, Nakipoglu F. Middle lobe syndrome in children with asthma: review of 56 cases. J Asthma 2004;41:411–417. [DOI] [PubMed] [Google Scholar]
- 20.Rashid A, Nanjappa S, Greene JN. Infectious causes of right middle lobe syndrome Cancer Control. 2017;24:60–65. [DOI] [PubMed] [Google Scholar]
- 21.Beigelman A, Bacharier LB. The role of early life viral bronchiolitis in the inception of asthma. Curr Opin Allergy Clin Immunol. 2013;13:211–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soyer O, Ozen C, Cavkaytar O, et al. Right middle lobe atelectasis in children with asthma and prognostic factors. Allergol Int. 2016;65:253–258. [DOI] [PubMed] [Google Scholar]
- 23.Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on physiotherapy for critically ill patients. Intensive Care Med. 2008;34:1188–1199. [DOI] [PubMed] [Google Scholar]
- 24.Pejhan S, Salehi F, Niusha S, et al. Ten years’ experience in surgical treatment of right middle lobe syndrome. Ann Thorac Cardiovasc Surg 2015;21:354–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Büyükşahin HN, Emiralioğlu N, Tural DA, et al. The Importance of Flexible Bronchoscopy in Difficult-to-treat Asthma from a Pediatric Pulmonology Perspective. Turk Arch Pediatr 2022;57:310–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


