Figure 1. Social determinants of health (SDOH) in atrial fibrillation (AF), cross-cutting themes.
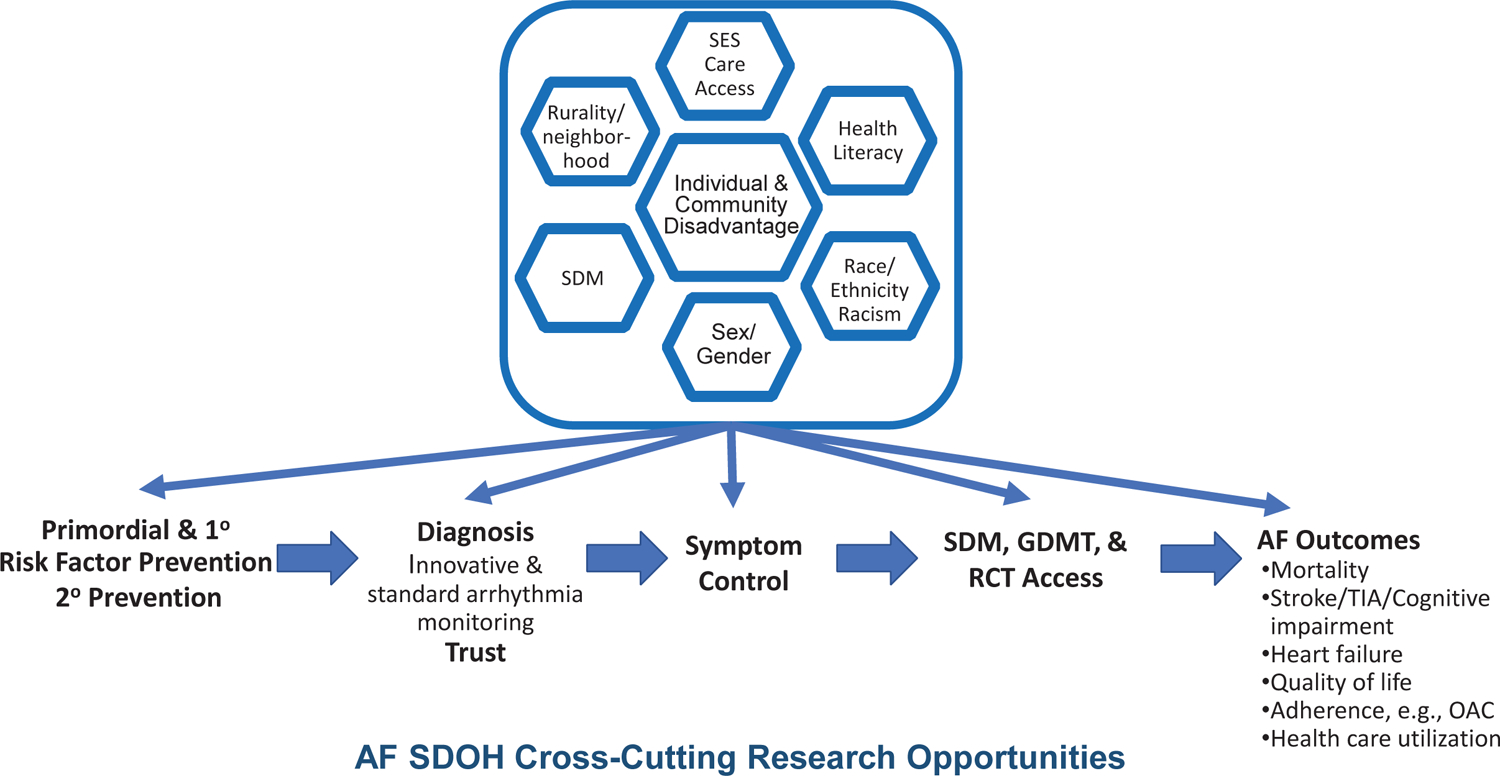
Individuals and communities accumulate disadvantages across the life course. Systemically disadvantaged SDOH are displayed in the top half of the figure, including: (1) socioeconomic status (SES) and access to care; (2) health literacy; (3) race, ethnicity, and racism; (4) sex and gender; (5) shared decision-making (SDM) in systemically disadvantaged populations; and (6) place (e.g., rurality, neighborhood, and community). The disadvantages accrue throughout the life course of individuals developing AF from the primordial emergence of risk factors, to primary prevention of risk factors, to secondary prevention of established heart failure and myocardial infarction. Disadvantages manifest from inequities in diagnosis, awareness, and symptoms. Inequities also emerge in receipt of guideline-directed medical therapies (GDMT) and access to randomized controlled trials (RCT), which lack diversity, yet inform GDMT. Each step along the lifecourse of AF contributes to inequities in AF outcomes, including stroke, cognitive decline, heart failure, myocardial infarction, chronic kidney disease, quality of life, health care utilization, and mortality. See also table in eSupplement.
