Abstract
Medial patellofemoral ligament (MPFL) reconstruction is a commonly performed procedure to reestablish the checkrein to the lateral patellar translation in patients with recurrent patellofemoral instability. Graft tensioning is one of the most critical aspects of the procedure. Most surgical methods for MPFL reconstruction involve tensioning and securing the graft on the femoral side. In this article, we describe a technique for patellar-sided tensioning of the graft using all-suture anchors, which provides the surgeon with the ability to finely control graft tension with two independent graft limbs, while preserving patellar bone stock.
Technique Video
Patellofemoral instability is a common injury among young athletes, accounting for 3% to 7% of all acute knee injuries.1 The medial patellofemoral ligament (MPFL) is a biomechanically important restraint to lateral patellar dislocation and provides 50% to 60% of the patellar stability during the first 30° of knee flexion.2 MPFL rupture occurs with almost all patellar dislocations, and the resultant patholaxity is a frequent contributor to recurrent dislocations, chondral injuries, and long-term functional limitations.3
Although nonoperative treatment of a first-time patellar dislocation is often successful, surgery is recommended for patients with recurrent instability or patients with persistent symptoms despite conservative treatment.4,5 Several reconstruction techniques have been described for the treatment of MPFL rupture.6, 7, 8 These techniques vary in the choice of graft, method of patellar and femoral fixation, as well as the side of graft tensioning.9, 10, 11 Excellent results with high patient-reported outcomes and low recurrence rates have been reported with a variety of techniques.12, 13, 14 As such, there is currently no consensus on the optimal method for MPFL reconstruction.
This article describes a minimally invasive approach to MPFL reconstruction using all-suture anchor fixation and tensioning on the patellar side. This technique allows fine adjustments to the intraoperative tension of the MFPL and minimizes the risk of patellar fracture.
Surgical Technique
Video 1 demonstrates our technique for MPFL reconstruction. The procedure begins by placing the patient supine on a regular operating table. A foot and lateral thigh post is used to help position the leg at 90° of knee flexion (Fig 1). A large fluoroscopic C-arm machine is positioned on the contralateral side.
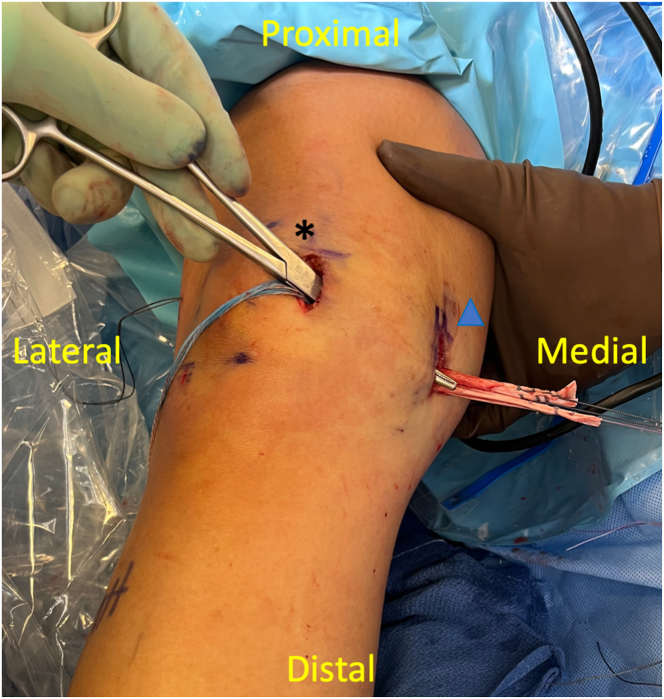
Fig 1.
Positioning of the right knee in the supine position on a regular operating room table with a foot (∗) and lateral thigh (triangle) post (underneath drapes). The C-arm fluoroscope is placed on the patient's contralateral side.
A standard anterolateral portal is made to assess chondral damage and loose bodies. During this time, an assistant can prepare a semitendinosus allograft by whipstitching both ends of the graft with a #2 nonabsorbable suture. The graft is doubled over and sized to a diameter of 7 mm. A minimum doubled graft length of 9 cm is recommended to ensure that the graft can reach from the proximal superomedial patella to Schöttle's point on the femur. The graft is then covered in a wet gauze sponge to prevent desiccation.
After the graft has been prepared, a 3-cm incision is made along the superomedial border of the patella. Dissection is carried along the bone down to the level of the capsule (Fig 2). The proximal half of the patella is prepared with a rongeur to remove any remaining soft tissue. A 1.6-mm Kirschner wire is inserted into the patella under lateral fluoroscopic guidance to ensure that the wire is located at the midpoint of the patella in the anteroposterior direction (Fig 3A). The drill guide for a 2.3-mm suture anchor is then placed over the wire. The wire is subsequently removed while holding the drill guide steady. A 2.3-mm, double-loaded, all-suture anchor (Iconix; Stryker, Kalamazoo, MI) is then inserted after drilling through the drill guide. A second all-suture anchor is then placed approximately 10 mm proximal to the first anchor (Fig 3B). The suture limbs from each anchor are clamped with a separate hemostat to keep the sutures from becoming intertwined.
Fig 2.
A 3-cm incision over the superomedial aspect of the patella (∗) is sharply made down to the knee capsule (triangle). A forceps is holding onto the medial patellofemoral ligament remnant and medial retinaculum (arrow).
Fig 3.
Patellar fixation of the 2.3-mm, all-suture anchors. (A) Anchor placement of the patella is confirmed under lateral fluoroscopic guidance. The first anchor (∗) should be placed in the superior half of the patella and in the center of the patella in the anteroposterior direction. (B) A second anchor (triangle) is deployed ∼1 cm proximal to the first anchor.
Next, a 2.4-mm Beath pin is then positioned at Schöttle's point on the medial femur with lateral fluoroscopic guidance (Fig 4). It is crucial that the pin is positioned on a true lateral fluoroscopic view where the posterior femoral condyles overlap, as slight malrotation will lead to graft malposition. The pin is then aimed slightly proximal and anterior and drilled out the lateral femoral cortex and skin. A 3-cm incision is then made centered around the Beath pin and carried down to bone. An acorn reamer with a diameter equal to the diameter of the graft (7 mm) is then inserted over the pin and drilled down to a depth of 25 mm. The graft is then folded in half over a no. 2 nonabsorbable passing suture. The free ends of this passing suture are placed in the Beath pin until the graft was ∼1 cm away from the pin (Fig 5A). This ensures that the passing suture ends do not get lost in the femoral tunnel. The pin is subsequently pulled out of the lateral thigh along with the passing suture. The passing suture ends are then pulled tight to bring the doubled-over graft into the blind femoral tunnel. With maximal tension placed on both suture ends, a polypropylene sheath followed by a 7-mm screw (Intrafix Advance PP Sheath and PEEK Screw; DePuy Mitek, Raynham, MA) is inserted into the anterior aspect of the femoral tunnel to fix the graft to the femur (Fig 5B). The passing suture is removed by pulling on one limb or by cutting it flush with the skin.
Fig 4.
Confirmation of the femoral insertion of the MPFL. A 2.4-mm Beath pin is placed on Schöttle's point using a true lateral fluoroscopic view of the femur.
Fig 5.
After a 7-mm cannulated reamer is used to drill a 25-mm femoral tunnel over the Beath pin. (A) The passing suture (triangle) of a doubled-over semitendinosus graft is placed into the Beath pin eyelet until the graft is ∼1 cm away from the pin. (B) Tension is applied to the passing suture (arrow), while an Intrafix Advance PP Sheath (∗) and PEEK screw (not shown) are inserted to secure the graft (DePuy Mitek, Raynham, MA).
At this point, a Kelly clamp is passed just superficial to the capsule from the patellar incision to the femoral incision (Fig 6). The clamp is opened to create a soft tissue tunnel. The sutures whipstitched to the ends of the graft are grasped, and the graft is passed through the soft tissue tunnel and out the patellar incision. The knee is then placed in 30° of flexion with a towel bump. An assistant can then hold the ends of the graft taut along the medial patellar border (Fig 7A). The patella should be held firmly in the center of the trochlear groove with neutral tilt. A free needle with a suture limb from the inferior anchor is used to pass 3 Krakow stitches through the graft at the level where the graft meets the anchor. It is critical not to pass these stitches too far from the anchor, as it could overtension or undertension the graft. The suture post of the corresponding color is then passed once through the graft. The other 2 suture limbs from the anchor are passed in a simple fashion through the same end of the graft. This process is repeated for the superior anchor suture limbs and the other end of the graft (Fig 7B). After all the sutures are passed, the post of the sutures used for the running Krakow from each anchor are pulled to reduce the graft to the patella at the desired tension. The 4 sets of sutures are then tied (Fig 8). Patellar stability is confirmed by having a firm endpoint to lateral translation of the patella at 30° of flexion and normal tracking through the entire range of motion. Excess graft is then trimmed.
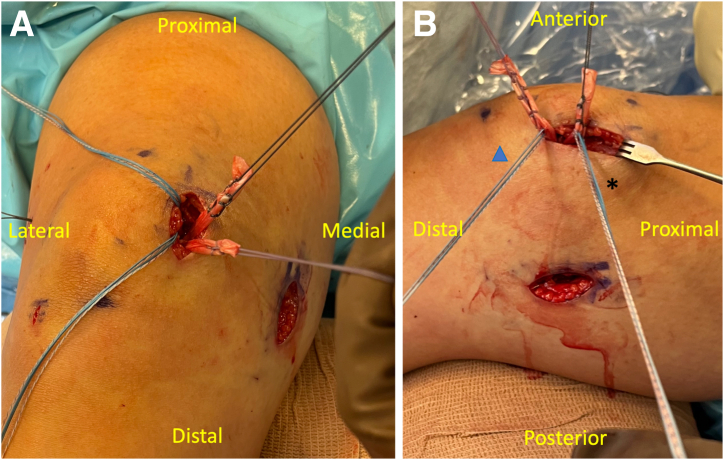
Fig 6.
A large Kelly clamp is passed from the patellar incision (∗) between capsule and medial retinaculum layers to grasp the semitendinosus graft from the femoral incision (triangle).
Fig 7.
(A) The graft limbs are held taut by an assistant next to the suture anchors. The knee is held in 30° flexion using a bump. (B) Sutures from the proximal anchor (∗) are passed through the superior graft limb using a free needle, while sutures from the distal anchor (triangle) are passed through the inferior graft limb.
Fig 8.
The graft is brought down to the patella and secured. Patellar stability was assessed by confirming a firm endpoint to lateral translation at 30° flexion and normal tracking through the entire range of motion. Excess graft was then trimmed (not shown).
Advantages and disadvantages (Table 1), as well as pearls and potential pitfalls (Table 2), of this technique are summarized.
Table 1.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
|
|
MPFL, medial patellofemoral ligament.
Postoperative Rehabilitation
After surgery, the patient is allowed to weight bear as tolerated with a hinged knee brace locked in extension. The brace can be unlocked from 0° to 40° flexion for range of motion exercises during the first 2 weeks. Subsequently, knee flexion can be increased by 10° each week with a goal of reaching 90° flexion by 6 weeks after surgery. At this phase, the knee brace and crutches are weaned. Range of motion is further increased to full extension and flexion between 6 to 12 weeks. After 3 months, the patient can advance to strengthening exercises and low-impact exercise. After 6 months, the patient can return to sport.
Discussion
Over the last decade, there have been multiple techniques described to reconstruct the MPFL. Most techniques utilize femoral-sided tensioning, in which the graft is secured on the femoral side with the use of an interference screw, button, or anchor.9,10,15 Determining the appropriate graft tension at the time of femoral fixation is difficult, as insertion of an interference screw or anchor can advance the graft into the tunnel and increase tension.16 Other techniques with adjustable loop button fixation allow for sequential tensioning of the femoral side of the graft, but is not reversible once the tension is applied.17 Femoral-sided tensioning is further complicated by the fact that both graft limbs are secured at the same time, limiting the surgeon's ability to make fine adjustments to graft tension with each individual limb.
In contrast to these described techniques, our current method of patellar-sided tensioning allows the surgeon to finely calibrate the amount of tension by passing sutures into the graft at the desired level. This allows both limbs of the graft to be tensioned independently and adjusted on the basis of patellar tracking and lateral translation intraoperatively. We believe this method minimizes the technical errors of undertightening and overtightening the graft, which can lead to recurrent lateral patellar instability and the development of stiffness and patellofemoral arthrosis, respectively.18,19
In our review of the literature, there were previously described MPFL reconstruction techniques utilizing a patellar-sided tensioning method.11,20 However, the strategies for surgical exposure and graft fixation varied substantially from the technique presented here. In our current technique, the MPFL origin and insertion are exposed using small incisions, which improves cosmesis and limits the amount of soft tissue dissection. Moreover, femoral fixation was obtained using a sheath-and-screw construct, which has been demonstrated to have higher yield strength and lower cyclical displacement for soft tissue graft fixation compared to the interference screws used in the other techniques.21 Finally, our use of 2.3-mm all-suture anchors obtains strong initial fixation and preserves bone stock, which may potentially minimize the risk of patellar fractures. Satalich et al. described a patellar-sided tensioning technique that utilizes 4.75-mm knotless SwiveLock anchors (Arthrex, Naples, FL) for patellar fixation.20 In a recent systematic review of MPFL patellar fixation techniques, no patellar fractures were observed when sockets were less than 4 mm.22
In conclusion, we present a minimally invasive MPFL reconstruction technique with patellar-sided tensioning. This simplified technique improves surgeon flexibility by allowing for fine adjustments to the tension of each graft limb. Further biomechanical and clinical studies are warranted to evaluate the outcomes of MPFL reconstruction with patellar-sided tensioning compared to femoral-sided tensioning.
Disclosures
The authors report the following potential conflicts of interest or sources of funding: A.Z. reports consulting fees from Stryker Corporation and DePuy Mitek, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
1:21 – 1:31: The procedure begins with diagnostic knee arthroscopy. This is a view of the medial patella through the anterolateral portal. We see here the absence of a medial patellofemoral ligament (MPFL) attachment on the medial patella.
1:32 – 1:45: A 3-cm longitudinal incision was made over the superior medial patella. As shown here, dissection was carried along bone down to the level of the capsule. A forceps is holding onto the MPFL remnant.
1:46 – 1:57: A 1.6-mm Kirschner wire (K-wire) was inserted into the patella under lateral fluoroscopic guidance to ensure that the wire is located at the midpoint of the patella in the anteroposterior direction.
1:58 – 2:12: A 2.3-mm, double-loaded, all-suture anchor was inserted into the patella at the location of the K-wire. A second 2.3-mm, all-suture anchor was then placed ∼10 mm proximal to the first anchor using lateral fluoroscopic guidance.
2:13 – 2:25: A 2.4-mm Beath pin was then placed under lateral fluoroscopic guidance at Schottle's point. The pin is then aimed slightly proximally and anteriorly and drilled out the lateral femoral cortex and skin.
2:26 – 2:38: After making a 3-cm incision over the Beath pin, an acorn reamer equal to the diameter of the graft is inserted 25 mm. A doubled-over semitendinosus graft is passed into the femoral tunnel.
2:39 – 2:45: A polypropylene sheath is inserted into the femoral tunnel with the passing sutures held under tension.
2:46 – 2:50: A polyether ether ketone (PEEK) screw is subsequently inserted into the polypropylene sheath.
2:51 – 3:00: A Kelly clamp is passed just superficial to capsule from the patellar incision to the femoral incision. The graft is passed through the soft tissue tunnel and out the patellar incision.
3:01 – 3:44: The knee is then placed in 30° of flexion with a towel bump. An assistant can then hold the ends of the graft taut along the medial patellar border. The patella should be held firmly in the center of the trochlear groove with neutral tilt. A free needle with a suture limb from the inferior anchor is used to pass 3 Krakow stitches through the graft at the level where the graft meets the anchor. It is critical not to pass these stitches too far from the anchor, as it could overtension or undertension the graft. The suture post of the corresponding color is then passed once through the graft. The other 2 suture limbs from the anchor are passed in a simple fashion through the same graft end. This process is repeated for the superior anchor suture limbs and the other end of the graft.
3:45 – 3:54: The posts of the sutures used for the running Krakow from each anchor are pulled tight to reduce the graft to the patella at the desired tension. The 4 sets of sutures are then tied.
3:55 – 4:11: Patellar stability is confirmed by having a firm endpoint to lateral translation of the patella at 30° of flexion and normal tracking through the entire range of motion.
4:12 – 4:16: At follow-up, the patient had resolution of knee pain and patellar instability.
References
- 1.Mitchell J., Magnussen R.A., Collins C.L., et al. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am J Sports Med. 2015;43:1676–1682. doi: 10.1177/0363546515577786. [DOI] [PubMed] [Google Scholar]
- 2.Philippot R., Boyer B., Testa R., Farizon F., Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20:331–336. doi: 10.1007/s00167-011-1598-6. [DOI] [PubMed] [Google Scholar]
- 3.Shatrov J., Vialla T., Sappey-Marinier E., et al. At 10-year minimum follow-up, one-third of patients have patellofemoral arthritis after isolated medial patellofemoral ligament reconstruction using gracilis tendon autograft. Arthroscopy. 2023;39:349–357. doi: 10.1016/j.arthro.2022.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Mistry J.B., Bonner K.F., Gwam C.U., Thomas M., Etcheson J.I., Delanois R.E. Management of injuries to the medial patellofemoral ligament: A review. J Knee Surg. 2018;31:439–447. doi: 10.1055/s-0037-1604142. [DOI] [PubMed] [Google Scholar]
- 5.Magnussen R.A., Verlage M., Stock E., et al. Primary patellar dislocations without surgical stabilization or recurrence: How well are these patients really doing? Knee Surg Sports Traumatol Arthrosc. 2017;25:2352–2356. doi: 10.1007/s00167-015-3716-3. [DOI] [PubMed] [Google Scholar]
- 6.Hohn E., Pandya N.K. Does the utilization of allograft tissue in medial patellofemoral ligament reconstruction in pediatric and adolescent patients restore patellar stability? Clin Orthop Relat Res. 2017;475:1563–1569. doi: 10.1007/s11999-016-5060-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camanho G.L., Bitar A.C., Hernandez A.J., Olivi R. Medial patellofemoral ligament reconstruction: A novel technique using the patellar ligament. Arthroscopy. 2007;23:108 e101–104. doi: 10.1016/j.arthro.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Carmont M.R., Maffulli N. Medial patellofemoral ligament reconstruction: A new technique. BMC Musculoskelet Disord. 2007;8:22. doi: 10.1186/1471-2474-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ishibashi Y., Kimura Y., Sasaki E., Sasaki S., Yamamoto Y., Tsuda E. Medial patellofemoral ligament reconstruction using FiberTape and knotless SwiveLock anchors. Arthrosc Tech. 2020;9:e1197–e1202. doi: 10.1016/j.eats.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monllau J.C., Erquicia J.I., Ibanez M., et al. Reconstruction of the medial patellofemoral ligament. Arthrosc Tech. 2017;6:e1471–e1476. doi: 10.1016/j.eats.2017.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duke A.J., Dai A., Botros D., et al. A patella-sided tensioning technique for medial patellofemoral ligament reconstruction. Arthrosc Tech. 2023;12:e483–e489. doi: 10.1016/j.eats.2022.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee D.Y., Park Y.J., Song S.Y., Hwang S.C., Park J.S., Kang D.G. Which technique is better for treating patellar dislocation? A systematic review and meta-analysis. Arthroscopy. 2018;34:3082–3093 e3081. doi: 10.1016/j.arthro.2018.06.052. [DOI] [PubMed] [Google Scholar]
- 13.McNeilan R.J., Everhart J.S., Mescher P.K., Abouljoud M., Magnussen R.A., Flanigan D.C. Graft choice in isolated medial patellofemoral ligament reconstruction: A systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy. 2018;34:1340–1354. doi: 10.1016/j.arthro.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 14.Liu Z., Yi Q., He L., et al. Comparing nonoperative treatment, MPFL repair, and MPFL reconstruction for patients with patellar dislocation: A systematic review and network meta-analysis. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211026624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luczak S.B., Stelzer J.W., Fitzsimmons K.P., Pace J.L. Medial patellofemoral ligament reconstruction and lateral retinacular lengthening from a lateral approach. Arthrosc Tech. 2021;10:e987–e994. doi: 10.1016/j.eats.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith M.K., Werner B.C., Diduch D.R. Avoiding complications with MPFL reconstruction. Curr Rev Musculoskelet Med. 2018;11:241–252. doi: 10.1007/s12178-018-9479-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mochizuki Y., Kaneko T., Kawahara K., Toyoda S., Ikegami H., Musha Y. A 2-year follow-up of isolated medial patellofemoral ligament reconstruction by using soft suture anchor and adjustable cortical fixation system. J Orthop. 2019;16:356–360. doi: 10.1016/j.jor.2019.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beck P., Brown N.A., Greis P.E., Burks R.T. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557–1563. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 19.Jackson G.R., Tuthill T., Gopinatth V., et al. Complication rates after medial patellofemoral ligament reconstruction range from 0% to 32% with 0% to 11% recurrent instability: A systematic review. Arthroscopy. 2023;39:1345–1356. doi: 10.1016/j.arthro.2023.01.098. [DOI] [PubMed] [Google Scholar]
- 20.Satalich J., Barber C., O'Connell R. Medial patellofemoral ligament reconstruction: A surgical technique to dynamically control graft tension. Arthrosc Tech. 2022;11:e2309–e2318. doi: 10.1016/j.eats.2022.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kousa P., Jarvinen T.L., Vihavainen M., Kannus P., Jarvinen M. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: Tibial site. Am J Sports Med. 2003;31:182–188. doi: 10.1177/03635465030310020501. [DOI] [PubMed] [Google Scholar]
- 22.Desai V.S., Tagliero A.J., Parkes C.W., et al. Systematic review of medial patellofemoral ligament reconstruction techniques: Comparison of patellar bone socket and cortical surface fixation techniques. Arthroscopy. 2019;35:1618–1628. doi: 10.1016/j.arthro.2018.10.150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1:21 – 1:31: The procedure begins with diagnostic knee arthroscopy. This is a view of the medial patella through the anterolateral portal. We see here the absence of a medial patellofemoral ligament (MPFL) attachment on the medial patella.
1:32 – 1:45: A 3-cm longitudinal incision was made over the superior medial patella. As shown here, dissection was carried along bone down to the level of the capsule. A forceps is holding onto the MPFL remnant.
1:46 – 1:57: A 1.6-mm Kirschner wire (K-wire) was inserted into the patella under lateral fluoroscopic guidance to ensure that the wire is located at the midpoint of the patella in the anteroposterior direction.
1:58 – 2:12: A 2.3-mm, double-loaded, all-suture anchor was inserted into the patella at the location of the K-wire. A second 2.3-mm, all-suture anchor was then placed ∼10 mm proximal to the first anchor using lateral fluoroscopic guidance.
2:13 – 2:25: A 2.4-mm Beath pin was then placed under lateral fluoroscopic guidance at Schottle's point. The pin is then aimed slightly proximally and anteriorly and drilled out the lateral femoral cortex and skin.
2:26 – 2:38: After making a 3-cm incision over the Beath pin, an acorn reamer equal to the diameter of the graft is inserted 25 mm. A doubled-over semitendinosus graft is passed into the femoral tunnel.
2:39 – 2:45: A polypropylene sheath is inserted into the femoral tunnel with the passing sutures held under tension.
2:46 – 2:50: A polyether ether ketone (PEEK) screw is subsequently inserted into the polypropylene sheath.
2:51 – 3:00: A Kelly clamp is passed just superficial to capsule from the patellar incision to the femoral incision. The graft is passed through the soft tissue tunnel and out the patellar incision.
3:01 – 3:44: The knee is then placed in 30° of flexion with a towel bump. An assistant can then hold the ends of the graft taut along the medial patellar border. The patella should be held firmly in the center of the trochlear groove with neutral tilt. A free needle with a suture limb from the inferior anchor is used to pass 3 Krakow stitches through the graft at the level where the graft meets the anchor. It is critical not to pass these stitches too far from the anchor, as it could overtension or undertension the graft. The suture post of the corresponding color is then passed once through the graft. The other 2 suture limbs from the anchor are passed in a simple fashion through the same graft end. This process is repeated for the superior anchor suture limbs and the other end of the graft.
3:45 – 3:54: The posts of the sutures used for the running Krakow from each anchor are pulled tight to reduce the graft to the patella at the desired tension. The 4 sets of sutures are then tied.
3:55 – 4:11: Patellar stability is confirmed by having a firm endpoint to lateral translation of the patella at 30° of flexion and normal tracking through the entire range of motion.
4:12 – 4:16: At follow-up, the patient had resolution of knee pain and patellar instability.