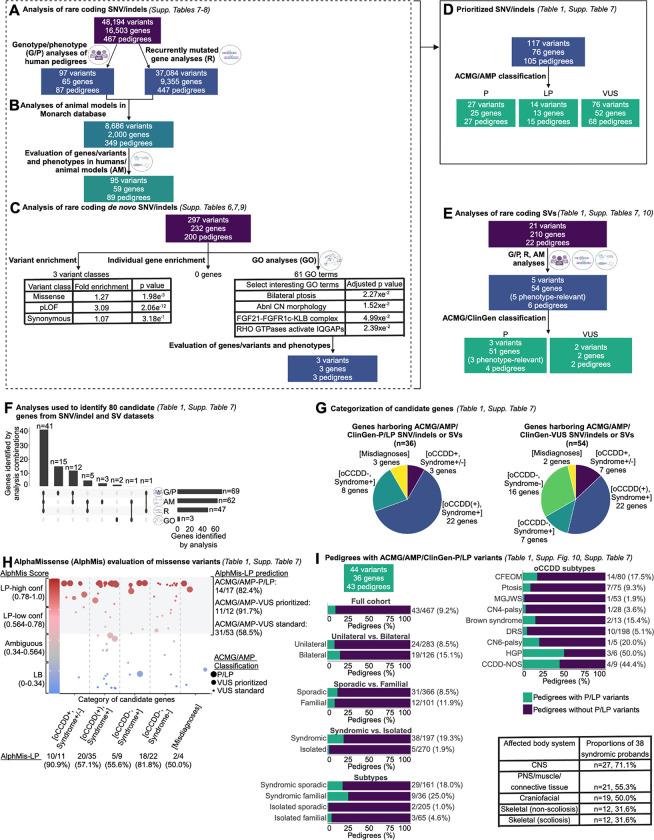
Figure 3. Workflow of genetic analyses.
A-C: Workflow for analyses of rare coding SNVs and indels. A: Pedigree-based genotype/phenotypes (G/P) analyses and recurrently mutated gene analyses. Rare coding SNVs/indels in all 467 pedigrees were identified and subjected to genotype/phenotype analyses as described (Supplementary Methods, “SNV/indel filtering and prioritization” and “Biological prioritization of SNVs/indels” sections). Genes that had SNVs/indels meeting the parameters defined in Supplementary Methods, “SNV/indel filtering and prioritization” and that were mutated in more than one pedigree were defined as recurrently mutated genes. Recurrently mutated genes were queried in all 467 pedigrees regardless of specific oCCDD diagnosis. B: Workflow for animal model analyses (“AM” analyses). Each of the 65 genes that harbored rare coding SNVs/indels derived from G/P analyses and the 9,355 genes identified from recurrently mutated gene (“R”) analyses (from ‘A’) were annotated for putatively relevant animal model phenotypes in the Monarch database, which yielded 2,000 genes with putatively oCCDD-relevant animal models. 59 candidate genes / 95 variants were prioritized from this analysis (defined in Supplementary Methods, “Animal model analyses” section). C: Workflow for statistical and gene ontology (GO) analyses of de novo variants (DNVs). Rare coding DNV SNV/indels were assessed for overall enrichment of various classes of DNVs (left) and enrichment of DNVs in individual genes (middle) through DenovolyzeR, and for enrichment of genes in specific pathways through GO analysis (right). Numbers of total and specific classes of enriched GO terms are displayed, along with select enriched GO terms of biological interest. Genes derived from the GO terms “FGF21-FGFR1c-KLB complex” and “RHO GTPases activate IQGAPs” were nominated for ACMG/AMP classification. D: ACMG/AMP classification. In total from the G/P, R, AM, and/or GO analyses of SNVs/indels in (A-C), 117 variants in 76 genes were prioritized and classified by the ACMG/AMP criteria. The gene/variant counts were derived from (A-C) minus redundant genes/variants. In total, only 76 distinct genes are represented among the three ACMG/AMP classification categories, as some genes had variants in more than one classification category. E: Rare coding SVs were prioritized using G/P, R, and AM analyses as described for SNV/indels, which led to the nomination of 5 SVs for classification by ACMG/ClinGen criteria. F: UpSet plot summarizing the combinations of analyses (G/P, AM, R, and GO) used to derive the 80 candidate genes whose variants were nominated for ACMG/AMP/ClinGen classification of SNV/indels (76 genes from D) or SVs (4 genes not overlapping with SNV/indels). Vertical bars denote numbers of candidate genes identified by each combination of analyses. Horizontal bars denote numbers of genes identified by each analysis type in total (numbers were obtained by adding genes with prioritized SNV/indels plus genes with prioritized SVs minus genes represented redundantly between the SNV/indel and SV classes; Supplementary Table 7). G: Classification of candidate genes harboring ACMG/AMP/ClinGen-P/LP SNV/indels and SVs (left chart), or ACMG/AMP/ClinGen-VUS SNV/indels and SVs (right chart). Among the 80 genes with P/LP or VUS variants (F), 10 were represented in both categories. Genes were stratified into five categories. Purple [oCCDD+,Syndrome+/−]: genes that were definitively associated with oCCDDs before this study and were genetically pre-screened in most probands. Blue [oCCDD(+),Syndrome+]: genes that had at least occasional prior oCCDD association but were typically part of specific monogenic syndromes and thus not pre-screened. Dark green [oCCDD−,Syndrome+]: genes that fit the syndromic component of each proband’s phenotype but that, to our knowledge, have no prior oCCDD association. Light green [oCCDD−,Syndrome−]: genes that, to our knowledge, had no reported association with either the oCCDD or non-CCDD phenotype of the probands who harbor them. Yellow [Misdiagnoses]: genes associated with alternative non-neurogenic/ non-CCDD etiologies and represent misdiagnoses or oCCDD phenocopies. H: AlphaMissense (AlphMis) could be used to assess 82 of the ACMG/AMP classified missense SNVs. X-axis: Numbers of missense variants and percent scored as AlphMis-LP in each of the five categories as defined in (G). Y-axis (left side): AlphMis scores on a scale of zero to one accompanied by the corresponding pathogenicity score (LB, Ambiguous, LP-low confidence, LP-high confidence). Scores are color-coded from blue (LB) to red (LP). Each dot on the plot represents a separate missense variant, and dot sizes correspond with ACMG/AMP classifications (large dots: ACMG/AMP-P/LP variants, medium dots: strongly prioritized ACMG/AMP-VUS, small dots: standardly prioritized ACMG/AMP-VUS). Strongly prioritized ACMG/AMP-VUS are the missense VUS denoted in Table 1; while these are formally classified as ACMG/AMP-VUS, we concluded that these variants have compelling biological and/or genotype/phenotype evidence and are most likely to be substantiated over time. Standardly prioritized ACMG/AMP-VUS are all additional missense ACMG/AMP-VUS denoted in Supplementary Table 7 that we prioritized but that currently have less supportive evidence than the strongly prioritized VUS. High-confidence and low-confidence AlphMis-LP variants are encompassed by the gray shaded region of the graph and compared to their independently obtained ACMG/AMP classifications (right side of the graph); numerical summaries are provided for each, for instance: 14/17 (82.4%) ACMG/AMP-P/LP variants were also scored as LP by AlphaMissense. I: Rates of ACMG/AMP/ClinGen-P/LP variants (SNVs, indels, and SVs) obtained for the full cohort (left) and individual subgroups (top right). Rates are given as the number of pedigrees within each group who had ACMG/AMP/ClinGen-P/LP variant(s) relative to the total number of pedigrees within that group. Green= pedigrees with ACMG/AMP/ClinGen-P/LP variant(s); Purple= pedigrees without ACMG/AMP/ClinGen-P/LP variant(s). Among 38 syndromic probands who had ACMG/AMP/ClinGen-P/LP variant(s), the most frequently affected body systems are shown (bottom right). For all relevant panels, accompanying supplementary figures and tables are denoted. Abbreviations: AM=animal model analyses, abnl=abnormal, ACMG=American College of Genetics and Genomics, AlphMis=AlphaMissense, AMP=Association for Molecular Pathology, CCDD=congenital cranial dysinnervation disorder, CCDD-NOS=CCDD not otherwise specified, CFEOM=congenital fibrosis of the extraocular muscles, ClinGen=Clinical Genome Resource, CN=cranial nerve, CN4-palsy=fourth nerve palsy, CN6-palsy=congenital sixth nerve palsy, CNS=central nervous system, conf=confidence, DRS=Duane retraction syndrome, GO=gene ontology analyses, G/P=genotype/phenotype analyses, HGP=horizontal gaze palsy, HPO=human phenotype ontology, indel=small insertion/deletion, LB=likely benign, LP=likely pathogenic, MGJWS=Marcus Gunn jaw-winking synkinesis, misc=miscellaneous, oCCDD=ocular congenital cranial dysinnervation disorder, P=pathogenic, pLOF=predicted loss of function (nonsense, splicing, or frameshift), PNS=peripheral nervous system, ptosis=congenital ptosis, R=recurrently mutated gene analyses, SNV=single nucleotide variant, SV=structural variant, VUS=variant of uncertain significance.