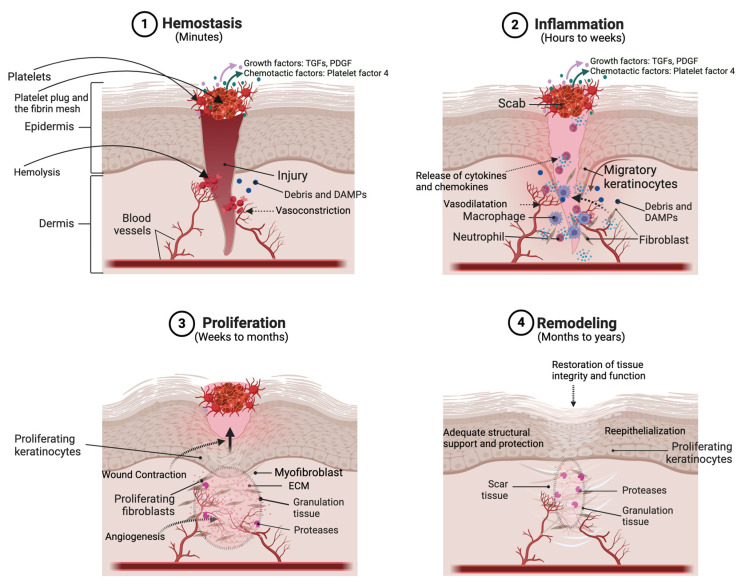
Figure 2.
Schematic illustrating the various phases of the wound healing process. A full-thickness injury to the skin wounds the epithelium and dermis, leading to bleeding from damaged dermal blood vessels. (1) In the first phase of wound healing, which occurs within minutes, bleeding is controlled and stopped (i.e., hemostasis is induced) via the formation of a scab composed of adhering platelets and a fibrin mesh. The injury can also result in the release of various growth factors [like transforming growth factors (TGFs) and platelet-derived growth factor (PDGF)] and chemotactic factors, as well as damage-associated molecular patterns (DAMPs). (2) In the inflammation phase, keratinocytes begin to migrate from the wound edge to re-epithelialize the wound. Also, innate immune cells (such as macrophages and neutrophils) are activated, often by microbial components entering the skin through the compromised barrier or DAMPs produced as a result of the injury, to secrete cytokines and chemokines. In addition, fibroblasts are recruited to begin synthesizing extracellular matrix (ECM) proteins. (3) In the proliferation phase, keratinocytes divide to restore the epidermal thickness and dermal fibroblasts/myofibroblasts proliferate and deposit extracellular matrix (ECM) proteins, forming granulation tissue, to regenerate the dermis. Endothelial cells promote new vessel formation (angiogenesis) to ensure adequate blood flow and nutrient supply. (4) During remodeling, collagen fibers mature and become more organized and cross-linked. Excess cells undergo apoptosis and ECM proteins are deposited and degraded in a balanced manner to restore proper tissue architecture and function. Created with Biorender.com.