Abstract
Background:
Percutaneous Zadek osteotomy (ZO) has emerged as a surgical treatment of insertional Achilles tendinopathy (IAT) over the last decade. Existing literature is limited regarding the comparison of this approach with the more established, open ZO technique. This systematic review aims to evaluate and compare the current data on open vs percutaneous ZO approaches to help set evidence-based guidelines.
Methods:
A systematic literature search was performed using the keywords (Zadek osteotomy) OR (Keck and Kelly osteotomy) OR (dorsal closing wedge calcaneal osteotomy) OR (Haglund Deformity) OR (Haglund Syndrome) OR (Insertional Achilles Tendinopathy) and MeSH terms Osteotomy, Calcaneus, Syndrome, Insertional, Achilles tendon, and Tendinopathy. Our search included the following databases: PubMed, Embase, and the Cochrane Library. The PRISMA protocol and the Cochrane Handbook guidelines were followed. All studies included were published from 2009 to 2024 and included the use of open or percutaneous approaches of ZO for the treatment of IAT with at least a 12-month follow-up. The MINORS score criteria were used to evaluate the strength and quality of studies.
Results:
A total of 17 studies were reviewed, including 611 subjects and 625 ZO procedures. Of these procedures, 81 (11%) subjects had a percutaneous and 544 (89%) subjects had an open ZO. The mean follow-up time was 16.1 months for patients treated with percutaneous ZO and 36.1 months for patients treated with open ZO. Both open and percutaneous studies included in this review showed postoperative improvements in AOFAS, FFI, VISA-A, and VAS scores in patients with IAT. The reported complication rate was 5.8% among patients treated with percutaneous ZO and 10.2% among patients treated with open ZO.
Conclusion:
Percutaneous ZO is an emerging approach with substantially fewer documented cases compared with the open ZO. Both percutaneous and open ZO appear to be relatively effective treatments for insertional Achilles tendinopathy with Haglund’s deformity. The lower complication rates reported for percutaneous ZO is encouraging. Further investigation with more subjects undergoing percutaneous ZO is clearly needed.
Keywords: Haglund’s deformity, insertional Achilles tendinopathy, Haglund’s deformity, minimally invasive surgery, MIS, percutaneous, systematic review, Zadek osteotomy
Introduction
Approximately 6% of the population reports Achilles tendon pain in their lifetime. Of these patients, around one-third are diagnosed with insertional Achilles tendinopathy (IAT).17,19,21 IAT is a degenerative process of the Achilles tendon; it is an overuse condition characterized by degenerative, cumulative tissue microtrauma that presents at the tendon’s insertion onto the calcaneal tuberosity. 39 Additionally, metabolic disorders such as diabetes mellitus, hypercholesterolemia, thyroid disorders, and obesity can predispose a patient for IAT. 29 Patients with IAT commonly present with increased tendon thickness and posterior heel pain.20,27 IAT often coexists with retrocalcaneal bursitis and Haglund’s deformity (a posterosuperior bony grown of the calcaneus), comprising the Haglund’s syndrome triad. 32 Primary treatment of IAT is nonoperative; management includes eccentric Achilles-strengthening exercise, nonsteroidal anti-inflammatories, orthotics, and shoe wear modification. 46 However, 20% to 40% of patients will fail to improve with these more conservative treatment strategies. 25 Nonoperative interventions include physical therapy, anti-inflammatory medications, and shoe wear modification. If patients continue to have persistent pain and activity limitation despite 3-6 months of nonoperative intervention, surgery may be indicated. 42 For patients with IAT who wish to return to a specific physical activity, surgery followed by early postoperative weightbearing and functional rehabilitation may be recommended so as to expedite new tendon formation and superior functional outcomes. 36
A dorsal closing wedge calcaneal osteotomy for the treatment of IAT was first described by Isadore Zadek in 1939 and was later popularized by Keck and Kelly in 1965.18,44 The Zadek osteotomy (ZO) relieves symptoms of IAT by shortening the calcaneus and altering the orientation of the Achilles tendon to ultimately reduce impingement between the Achilles tendon and the calcaneus.4,28
ZO was first described as an open surgery; similar to other open foot and ankle surgeries, this technique has been associated with complications such as nerve injuries and wound healing issues.7,12 -14,18,22,37,38,44,45 However, in light of new, minimally invasive surgery (MIS) techniques, the ZO can be completed percutaneously. The percutaneous ZO is chosen with the intention of decreasing risks of complications commonly observed with the open ZO, while also allowing for earlier weightbearing and recovery.16,28 Recent literature reviews have analyzed the clinical effectiveness of ZO; a general improvement in patient reported outcomes has been repetitively cited irrespective of percutaneous vs open ZO. Complication rates have ranged from 3.1% to 16.7%.1,3,32,42 However, to our knowledge, no prior review has analyzed and compared the clinical outcomes between percutaneous and open approaches for ZO. The aim of this systematic review was to better inform surgeons’ evidence-based guidelines, and patient expectations, when selecting between the percutaneous vs open ZO.1,3,32,42
Methods and Search Strategy
This systematic literature review included studies that were published from 2008 to 2023. The databases used were PubMed, Embase, and the Cochrane Library. The following items were searched: (Zadek osteotomy) OR (Keck and Kelly osteotomy) OR (dorsal closing wedge calcaneal osteotomy) OR (Haglund Deformity) OR (Haglund Syndrome) OR (Insertional Achilles Tendinopathy), and MeSH terms Osteotomy, Calcaneus, Syndrome, Insertional, Achilles tendon, and Tendinopathy, without a language filter. Initial screening of titles, abstracts, and full-text studies was performed. The Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) protocol and the Cochrane Handbook guidelines were followed.15,30 The Methodological Index for Non-Randomized Studies (MINORS) score criteria were used to evaluate the strength and quality of the studies. 35 Statistical analysis and meta-analysis were not performed because of the heterogeneity of the included studies.
Inclusion and Exclusion Criteria
Inclusion criteria allowed for any study published from 2009 to 2024 that involved the use of ZO for the use of IAT and/or Haglund’s deformity. Exclusion criteria included the following: pediatric studies or studies without minimum 12-month patient follow-up.
Data Collection and Abstraction
Two investigators independently evaluated titles, abstracts, and full text from the studies found in the search. The following data were extracted from each study: title, authors, journal of publication, year of publication, country, level of evidence, number of subjects, follow-up (minimum and mean), type(s) of osteotomy performed, number of procedures performed, mean age, sex, American Orthopaedic Foot & Ankle Society (AOFAS) score, Foot Function Index (FFI) score, Manchester-Oxford Foot Questionnaire (MOXFQ) score, visual analog scale (VAS) score, Victorian Institute of Sports Assessment–Achilles Questionnaire (VISA-A) score, satisfaction rate, Fowler-Phillip angles, Bohler angles, calcaneal pitch angles, calcaneal lengths, X/Y ratios, and complications. The MINORS score was used to evaluate the quality and bias of the 17 nonrandomized controlled trials (Table 1).30,35 The mean score among studies was 14.8, with a range of 12-18. These scores represent high-quality studies.
Table 1.
MINORS Scoring of Included Studies.
| Author | Aim | Inclusion | Prospective | Endpoint | Unbiased | Follow-up | Loss | Calculation | CG | G | Baseline | SA | Total Score | Zadek Osteotomy Type |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Choi and Suh 7 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 18 | Percutaneous |
| deMeireles et al 10 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Percutaneous |
| Mazura et al 26 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Percutaneous |
| Nordio et al 28 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Percutaneous |
| Choi and Suh 7 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 18 | Open |
| Friesenbichler et al 11 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Open |
| Ge et al 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 | Open |
| Georgiannos et al 14 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Open |
| López-Capdevila et al 22 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Open |
| Maffulli et al 23 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 18 | Open |
| Maffulli et al 24 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 | Open |
| Rutishauser et al 33 | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 12 | Open |
| Rutishauser et al 34 | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 14 | Open |
| Tourne et al 37 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 | Open |
| Tourné et al 38 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 | Open |
| Xu et al 43 | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 12 | Open |
| Zheng et al 45 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 13 | Open |
Abbreviations: CG = control groups; G, contemporary groups; MINORS, Methodological Index for Non-Randomized Studies; SA, statistical analyses.
Characteristics of the Systematic Review Search and Study Demographics
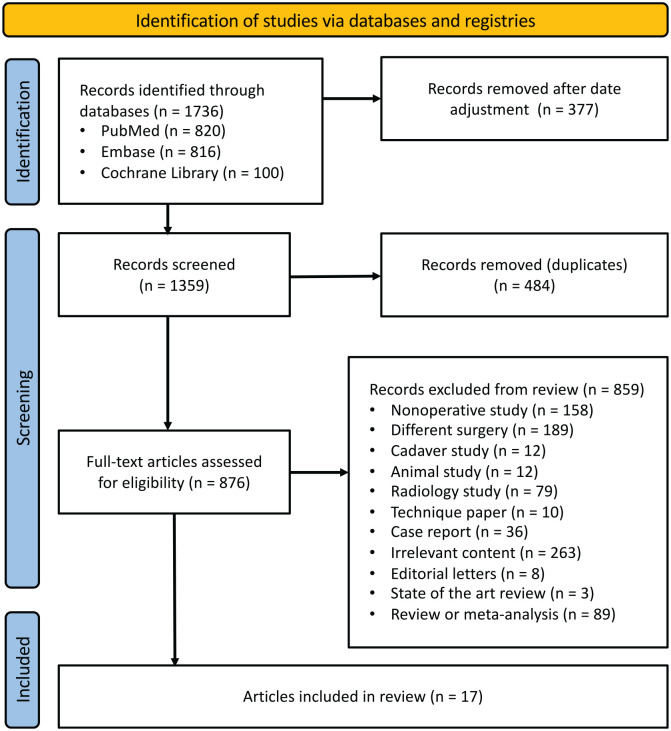
A total of 1736 studies were found after the primary database search (Figure 1). After adjusting for date criteria, 1359 studies were analyzed. A total of 17 studies were included in the current systematic review after passing screening criteria. Three studies were published abstracts and 14 of which were full-length publication.6,7,10 -12,14,22 -24,26,28,33,34,37,38,43,45 A total of 611 subjects and 625 procedures were found in these 17 studies; 81 procedures were percutaneous, and 544 procedures were open. The mean age of patients who underwent percutaneous ZO was 49.6 (range 37.4-57), and the mean age of the patients who endured open ZO was 47.65 (range 32.5-54.7). Mean follow-up time was 16.1 months (range 12.0-20.3 months) and 36.1 months (range 12.0-86.5 months) for patients who underwent percutaneous ZO and open ZO, respectively. Three studies were excluded from this mean calculation as only ranges were provided. Among the studies, the level of evidence ranged from II to IV. In the percutaneous group, there was 1 level IV study and 3 level III studies. In the open group, there were 2 level II, 8 level III, and 3 level IV studies. Characteristics and demographics of the studies are listed in Table 2.
Figure 1.
PRISMA flow diagram, overview of search strategy and selection criteria.
Table 2.
Demographics and Characteristics of Included Studies.
| Author | Country | Level of Evidence | Participants, n | Mean Age, y | Feet, n | Women, n | Follow-up, mo | Control Group | Zadek Osteotomy Type |
|---|---|---|---|---|---|---|---|---|---|
| Choi and Suh 7 | South Korea | III | 10 | 37.4 | 11 | 6 | 20.3 | Yes | Percutaneous |
| deMeireles et al 10 | USA | IV | 32 | 56.1 | 32 | NR | 16.1 | No | Percutaneous |
| Mazura et al 26 | Czech Republic | III | 12 | 47.8 | 12 | 6 | NR | No | Percutaneous |
| Nordio et al 28 | Italy | III | 26 | 57 | 26 | 14 | 12 | No | Percutaneous |
| Cengiz and Karaoglu 6 | Turkey | III | 20 | 45.8 | 20 | 14 | 72 | No | Open |
| Friesenbichler et al 11 | Switzerland | III | 16 | NR | 16 | NR | 12 | No | Open |
| Ge et al 12 | China | III | 12 | 32.8 | 12 | 3 | 86.5 | No | Open |
| Georgiannos et al 14 | Greece | IV | 52 | 32.5 | 64 | 30 | Range 36-60 | No | Open |
| López-Capdevila et al 22 | Spain | IV | 18 | 49 | 18 | 11 | 18.3 | No | Open |
| Maffulli et al 23 | Italy | IV | 28 | 54.7 | 28 | 15 | Range 24-30 | No | Open |
| Maffulli et al 24 | Ireland | II | 25 | 53.5 | 25 | 14 | Range 24-28 | No | Open |
| Rutishauser et al 33 | Switzerland | III | 126 | 49.7 | 126 | 58 | 24 | No | Open |
| Rutishauser et al 34 | Switzerland | III | 126 | 49.7 | 126 | 58 | 24 | No | Open |
| Tourne et al 37 | France | III | 50 | 54 | 50 | 15 | 84 | No | Open |
| Tourné et al 38 | France | II | 22 | 48.5 | 22 | 9 | 12 | No | Open |
| Xu et al 43 | Great Britain | III | 17 | 53 | 18 | 12 | 12 | No | Open |
| Zheng et al 45 | China | III | 19 | 48.6 | 19 | NR | 16.3 | No | Open |
Abbreviation: NR, not reported.
Results
Clinical Outcomes: AOFAS Score, VAS Score, Satisfaction Rate, and VISA-A Score
Preoperative and final follow-up AOFAS scores were reported in 7 studies that analyzed open ZO and no studies that analyzed percutaneous ZO. The mean AOFAS score among open ZO studies improved from 53.6 ± 6.7 (range 41.5-62.0) to 91.3 ± 4.7 (range 86.4-98.2). Statistically significant improvement was reported in 6 studies. Although Ge et al 12 did not document a P value, the improvement in AOFAS values observed in their study is comparable to the other open ZO studies that did document statistical significance. One percutaneous ZO study reported significant improvement in the FFI, which is analogous to the AOFAS score. 24 One open ZO study reported Manchester-Oxford Foot Questionnaire (MOXFQ) scores, which is also a measure comparable to AOFAS scores.5,9 Eight studies did not report AOFAS scores or equivalent index of change in function.
Preoperative and last follow-up visual analog scale (VAS) scores were reported in 2 percutaneous ZO studies and in 4 open ZO studies. The mean VAS scores in the percutaneous ZO studies improved from 9.0 ± 0.1 (range 8.9-9.0) to 2.3 ± 1.8 (range 1.0-3.6). The mean VAS score in the open ZO studies significantly improved from 20.4 ± 25.3 (range 6.3-58.2) to 7.5 ± 10.2 (range 0.9-22.7). Statistically significant improvement in VAS score was observed in all reporting studies (P < .01).
Preoperative and last follow-up VISA-A scores were reported in 1 percutaneous ZO study and 5 open ZO studies. The VISA-A score in the percutaneous ZO study improved from 36.8 to 88.0, which was statistically significant (P < .01). The VISA-A scores in the open ZO studies improved from a mean 45.0 ± 17.3 (range 25.8-65.9) to 87.4 ± 7.9 (range 76.5-98.2), all demonstrating statistically significant improvement (P < .01). There was also one study in the open ZO group, by Maffulli et al, that did not report preoperative VAS or VISA-A data. However, they did report scores at 1 month postoperation and again at 24 months postoperation. Maffulli et al 24 demonstrated a statistically significant improvement in VAS and VISA-A scores between patients at the 1-month and 24-month postoperative follow-ups (P < .0001). Additionally, 1 percutaneous ZO study reported a 92% satisfaction rate, whereas 5 open ZO studies reported a mean satisfaction rate of 86.1% ± 12.9% (range 67.4%-100%) (Table 3).
Table 3.
AOFAS, VAS, VISA-A, and Satisfaction Rate at Last Follow-up (Minimum 12 Months).
| Author | AOFAS | VAS | VISA-A |
Satisfaction Rate, % | Zadek Osteotomy Type | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | P | Pre | Post | P | Pre | Post | P | |||
| Choi and Suh 7 | NR | NR | NR | 8.9 | 3.6 | <.01 | 36.8 | 88.7 | <.01 | NR | Percutaneous |
| deMeireles et al 10 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Percutaneous |
| Mazura et al 26 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Percutaneous |
| Nordio et al 28 | FFI = 65 | FFI = 8 | <.01 | 9 | 1 | <.01 | NR | NR | NR | 92 | Percutaneous |
| Cengiz and Karaoglu 6 | 56.6 | 89.2 | <.01 | 8.6 | 4.1 | <.01 | NR | NR | NR | NR | Open |
| Friesenbichler et al 11 | NR | NR | NR | NR | NR | NR | NR | NR | NR | 80 | Open |
| Ge et al 12 | 52.0 | 98.2 | NR | NR | NR | NR | 37.1 | 98.2 | NR | NR | Open |
| Georgiannos et al 14 | 59.5 | 95.7 | <.01 | NR | NR | NR | 65.9 | 90.2 | <.01 | NR | Open |
| López-Capdevila et al 22 | 41.5 | 86.5 | <.01 | 8.3 | 2.2 | <.01 | 25.8 | 76.5 | <.01 | 100 | Open |
| Maffulli et al 23 | NR | NR | NR | NR | 32.0 | <.01 | NR | 83.0 | <.01 | NR | Open |
| Maffulli et al 24 | NR | NR | NR | 58.2 | 22.7 | <.01 | 35.8 | 86.8 | <.01 | NR | Open |
| Rutishauser et al 33 | NR | NR | NR | NR | NR | NR | NR | NR | NR | 88 | Open |
| Rutishauser et al 34 | NR | NR | NR | NR | NR | NR | NR | NR | NR | 67 | Open |
| Tourne et al 37 | 50.5 | 88.9 | <.05 | NR | NR | NR | 60.4 | 85.3 | <.05 | NR | Open |
| Tourné et al 38 | 62.0 | 94 | <.05 | NR | NR | NR | NR | NR | NR | NR | Open |
| Xu et al 43 | MOXFQ = 182 | MOXFQ = 74 | NR | NR | NR | NR | NR | NR | NR | NR | Open |
| Zheng et al 45 | 53.2 | 86.4 | <.01 | 6.3 | 0.9 | <.01 | NR | NR | NR | 95 | Open |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; FFI, Foot Function Index; MOXFQ, Manchester-Oxford Foot Questionnaire; VAS, visual analog scale; VISA-A, Victorian Institute of Sports Assessment–Achilles Questionnaire.
Radiographic Outcomes
Preoperative and postoperative Fowler-Phillip (FP) angle was reported in 3 open ZO studies and 1 percutaneous ZO study. In the open ZO studies, there was a significant improvement in mean FP angle from 55.3 ± 2.9 (range 53.2-58.6) to 40.2 ± 6.1 (range 35.9-47.2) (P < .05). In the percutaneous ZO study, there was a significant improvement in mean FP angle from 52.7 ± 6.3 to 30.2 ± 6.0 (P < .001). Preoperative and postoperative Bohler angles were reported in 1 open and 1 percutaneous ZO study. In the open ZO study, there was a significant improvement in mean Bohler angle from 32.1 ± 3.3 to 43.6 ± 2.8 (P < .05). In the percutaneous ZO study, there was a significant improvement in mean Bohler angle from 37.4 ± 10.2 to 49.0 ± 7.2 (P < .001).
Preoperative and postoperative calcaneal pitch (CP) angles were reported in 6 open ZO studies and 1 percutaneous ZO study. In the open ZO studies, the mean CP angle decreased from 25.9 (range 23.1-29.0) to 22.9 (range 19.8-26.5); however, this difference was not significant. Similarly, 1 percutaneous ZO study by Choi and Suh reported an unchanged mean CP angle at follow-up (22.3 ± 6.7 to 23.1 ± 5.4, P > .05). 7 However, the percutaneous ZO study by Mazura et al 26 found the CP angle to be prominently impacted by ZO. This study demonstrated a horizontal ZO to allow for the greatest CP angle correction. Mazura et al 26 proposed a reduction in CP angle to correlate with reduced tension on the Achilles tendon.
Preoperative and postoperative mean calcaneal length was measured in 4 open ZO studies, which decreased from 86.3 ± 3.6 mm (range 83.0-91.0) to 81.3 ± 3.0 mm (range 79.0-85.3). Preoperative and postoperative X/Y ratio was reported in 2 open ZO studies. This ratio is used to help assess the abnormality of the shape of the calcaneus in Haglund’s syndrome. The mean X/Y ratio improved from 2.1 ± 0.1 (range 2.1-2.2) to 2.9 ± 0.1 (range 2.8-3.0).37,38 Both of these were reported to be significant improvements (P < .05) (Table 4).
Table 4.
Reported Changes in Preoperative vs Postoperative Fowler-Phillip, Bohler, Calcaneal Pitch, Calcaneal Length, and X/Y Ratio Measurements.
| Author | Fowler-Phillip Angle | Bohler Angle | Calcaneal Pitch Angle | Calcaneus (mm) | X/Y Ratio | Zadek Osteotomy Type |
|---|---|---|---|---|---|---|
| Choi and Suh 7 | Pre: 52.7 | Post: 30.2 | Pre: 37.4 | Post: 49.0 | Pre: 22.3 | Post: 23.1 | NR | NR | Percutaneous |
| deMeireles et al 10 | NR | NR | NR | NR | NR | Percutaneous |
| Mazura et al 26 | NR | NR | NR | NR | NR | Percutaneous |
| Nordio et al 28 | NR | NR | NR | NR | NR | Percutaneous |
| Cengiz and Karaoglu 6 | NR | NR | Pre: 23.1 | Post: 22.4 | NR | NR | Open |
| Friesenbichler et al 11 | NR | NR | NR | NR | NR | Open |
| Ge et al 12 | Pre: 54.0 | Post: 35.9 | Pre: 32.1 | Post: 43.6 | Pre: 25.5 | Post: 25.4 | NR | NR | Open |
| Georgiannos et al 14 | NR | NR | NR | Pre: 87 | Post: 82 | NR | Open |
| López-Capdevila et al 22 | Pre: 53.2 | Post: 37.4 | NR | Pre: 24.8 | Post: 23.8 | Pre: 91.0 | Post: 85.3 | NR | Open |
| Maffulli et al 23 | NR | NR | NR | Pre: 83.0 | Post: 79.0 | NR | Open |
| Maffulli et al 24 | NR | NR | NR | Pre: 84.1 | Post: 79.0 | NR | Open |
| Rutishauser et al 34 | NR | NR | NR | NR | NR | Open |
| Rutishauser et al 33 | NR | NR | NR | NR | NR | Open |
| Tourne et al 37 | NR | NR | Pre: 25.5 | Post: 20.0 | NR | Pre: 2.1 | Post: 3.0 | Open |
| Tourné et al 38 | NR | NR | Pre: 29.0 | Post: 19.8 | NR | Pre: 2.2 | Post: 2.8 | Open |
| Xu et al 43 | Pre: 58.6 | Post: 47.2 | NR | Pre: 27.8 | Post: 26.5 | NR | NR | Open |
| Zheng et al 45 | NR | NR | NR | NR | NR | Open |
Complications
The rate of complications was reported by all studies. The total rate of complications among all studies was 45 of 471 (9.6%). Of note, 3 studies were excluded from this calculation because of a lack of complication report. The rate of complications among the percutaneous ZO studies was 4 of 69 (5.8%), and the rate of complications among open the ZO studies was 41 of 402 (10.2%). Among the percutaneous group, there was 1 case of painful hardware (1.4%) and 3 cases of nonunion that resulted in revision surgery (4.3%). Among the open ZO cases, there was 1 case of painful hardware (0.2%), 1 case of delayed union (0.2%), 2 cases of transient sural neuritis (0.5%), 1 case of delayed wound healing (0.2%), 8 cases of superficial wound infection treated with oral antibiotics (2.0%), 2 cases of deep vein thrombosis (0.5%), 2 cases of transient dysesthesia (0.5%), 1 case of complex regional pain syndrome (0.2%), 3 cases of paresthesia (0.7%), and 1 case of hardware failure that resulted in revision surgery (0.2%). Of note, 1 study in the open group, by Rutishauser et al, 33 did not specify the nature of their complications and only documented them as postoperative adverse events. These events were still included in our overall complication calculations (Table 5).
Table 5.
Complications per Study.
| Author | Painful Hardware | Nonunion | Delayed Union | Transient Neuritis | Delayed Wound Healing | Wound Infection | DVT | Transient Dysesthesia | Complex Regional Pain Syndrome | Paresthesia | Hardware Failure | Complication Rate, % | Zadek Osteotomy Type |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Choi and Suh 7 | 0 | 1 a | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9.1 | Percutaneous |
| deMeireles et al 10 | 0 | 1 a | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3.1 | Percutaneous |
| Mazura et al 26 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Percutaneous |
| Nordio et al 28 | 1 | 1 a | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7.7 | Percutaneous |
| Cengiz and Karaoglu 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Open |
| Friesenbichler et al 11 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Open |
| Ge et al 12 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8.3 | Open |
| Georgiannos et al 14 | 0 | 0 | 0 | 0 | 0 | 4 | 2 | 0 | 0 | 1 | 1 a | 12.5 | Open |
| López-Capdevila et al 22 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 16.7 | Open |
| Maffulli et al 23 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 10.7 | Open |
| Maffulli et al 24 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 12 | Open |
| Rutishauser et al 33 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 15.1 | Open |
| Rutishauser et al 34 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | Open |
| Tourne et al 37 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 6 | Open |
| Tourné et al 38 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Open |
| Xu et al 43 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Open |
| Zheng et al 45 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.3 | Open |
Abbreviations: DVT, deep vein thrombosis; NR, not reported.
Patients underwent revision surgery.
Discussion
To our knowledge, this systematic review is the largest and most complete to specifically examine and compare percutaneous ZO vs open ZO for the treatment of insertional Achilles tendinopathy. A total of 17 studies were included in this review, 3 of which were prospective and 14 of which were retrospective. Of note, 3 studies included in this review are published abstracts and presented limited data. The current systematic review demonstrated both percutaneous ZO and open ZO to be safe and effective treatments of IAT.
All patients included in studies within this review were aged ≥18 years and had at least 3-6 months of documented, failed nonoperative management before undergoing surgery. Inclusion criteria for all studies included patients with IAT and Haglund’s deformity. Of note, 1 study by Tourné et al 38 included a radiographic X/Y ratio of <2.5 in their inclusion criteria. No other specific radiographic data were collected as inclusion criteria. Along with patients who have refractory symptoms of IAT, surgery is also commonly recommended for competitive athletes because of the higher risk of recurring injury.14,21 Additionally, worse clinical and functional outcomes have been associated with strictly nonoperative treatment of IAT in athletes. 2 ZO has allowed for better outcomes and an early return to activity in these patients in comparison to other operative and nonoperative techniques for the treatment of IAT in atheltes. 14
Recently, there has been an increase in the use of minimally invasive (MIS) techniques to treat common foot and ankle pathologies; accordingly, the percutaneous ZO has been utilized more frequently for the treatment of IAT.7,10,16,26,28,40 Broadly, the advantages of MIS include reduced cutaneous complications, decreased need for analgesics, shorter operation duration, fewer deep infections, faster recovery, lower health care costs, and improvement of pain and patient-reported outcomes.2,7,8,31,40,41 More specifically, the percutaneous ZO has demonstrated promising results while minimizing wound healing complications and decreasing recovery time.7,40
Nevertheless, the percutaneous ZO is a relatively new approach with limited data on patient outcomes. The current systematic review provides the most up-to-date information on percutaneous and open ZO outcomes. Our results demonstrated that both percutaneous ZO and open ZO significantly improve AOFAS, FFI, VISA-A, and VAS scores at minimum 12 months’ postoperative follow-up. Improvement in VISA-A and VAS scores appear similar between percutaneous ZO and open ZO cases. Of note, radiologic outcomes such as Fowler-Phillip angle, Bohler angle, and calcaneal pitch angle were collected in very few studies. This limited our ability to accurately compare radiologic outcomes in percutaneous ZO vs open ZO techniques.
Previous reviews have also analyzed the complication rate of ZO for the treatment of IAT. Poutoglidou et al 32 found an overall complication rate of 9.48% for ZO, but grouped percutaneous and open procedures together in this analysis. Black et al 3 also grouped all percutaneous and open ZO cases together, and found a complication rate of 10%. When factoring all studies in our review together, our results supported the data of previous studies; we found an overall complication rate of 9.6%. However, when stratifying based on approach type, our results showed that the open approach to ZO had a complication rate of 10.2%, whereas the percutaneous approach had a reduced complication rate of 5.8%. This was further supported by a review by Agostinho De Lima Gomes et al, 1 which noted a 6.3% complication rate of percutaneous surgery for the treatment of Haglund’s deformity.
The limitations of this systematic review include the lack of randomized controlled trials that met our inclusion criteria. Additionally, because of the heterogenicity of the data presented by each individual study, meta-analysis was not possible and the broad results presented must be considered in light of that. Similarly, there were only 4 studies that included percutaneous ZO for IAT with only 81 total procedures, compared with the 13 studies that included open ZO with a total of 544 procedures. Although this difference can be attributed to the relatively novelty of the percutaneous ZO, it reduces the generalizability of these comparisons. Furthermore, follow-up time was longer for the open ZO compared to the percutaneous ZO studies, which may have impacted complication rates or outcomes.
Most studies included in this review had small sample sizes; only 3 of the included studies contained >50 patients, 2 of which were conference abstracts. This restriction has the potential to limit the power of each study. Additionally, the AOFAS forefoot score is a nonvalidated outcome measure; however, it is commonly used and deemed helpful in most studies. Finally, 3 of the studies included in the review were published abstracts and offered limited information, particularly regarding complication rate. Despite these limitations, this is the most complete and up-to-date review regarding available literature on the percutaneous and open ZO for the treatment of IAT.
Percutaneous ZO is an emerging technique in orthopaedic foot and ankle surgery. Positive outcomes reported with the percutaneous ZO thus far, as reflected in the current review, may encourage surgeons to consider adopting this approach for some patients. In the comparatively small number of percutaneous ZO procedures represented in the literature, reduced complication rates with similar functional and pain score improvement have been reported when compared to the reports for open approaches.
Conclusion
Both percutaneous and open ZO appear to be relatively effective treatments of insertional Achilles tendinopathy with Haglund’s deformity. Both techniques demonstrate significant postoperative improvement in function and pain. The percutaneous ZO was represented in substantially fewer peer-reviewed articles compared to the open approach at the time we conducted this review, which decreased our ability to accurately compare the 2 surgical cohorts given the 8-fold difference in size of subjects. The lower complication rates reported for percutaneous ZO is encouraging. Further investigation with more subjects undergoing percutaneous ZO is clearly needed.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114241241320 for Percutaneous vs Open Zadek Osteotomy for Treatment of Insertional Achilles Tendinopathy and Haglund’s Deformity: A Systematic Review by Yianni Bakaes, SarahRose Hall, J. Benjamin Jackson, A. Holly Johnson, Oliver N. Schipper, Ettore Vulcano, Jonathan R. M. Kaplan and Tyler A. Gonzalez in Foot & Ankle Orthopaedics
Footnotes
Ethical Approval: Ethical approval was not sought because this is a systematic review.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: A. Holly Johnson, MD, reports royalties or licenses from Novastep and Treace. Oliver Schipper, MD, reports royalties or licenses and consulting fees from Treace Medical Concepts, Vilex, Exactech, and Enovis. Ettore Vulcano, MD, reports royalties or licenses and consulting fees from Treace Medical Concepts and Vilex; consulting fees from Surgebright, and Novastep. Jonathan R.M. Kaplan, MD, reports royalties or licenses and consulting fees from Surgical Fusion Technologies, Enovis, Treace Medical Concepts, Vilex; consulting fees from Artelon, Edge Surgical, Exactech, and Surgebright. Tyler A. Gonzalez, MD, MBA, reports royalties or liceses and consulting fees from Treace Medical Concepts, Surgical Fusion Technologies, Vilex; consulting fees from Stryker, Surgebright and Enovis. Disclosure forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: SarahRose Hall, BA,  https://orcid.org/0000-0002-4026-3118
https://orcid.org/0000-0002-4026-3118
J. Benjamin Jackson III, MD, MBA,  https://orcid.org/0000-0002-9444-087X
https://orcid.org/0000-0002-9444-087X
Oliver N. Schipper, MD,  https://orcid.org/0000-0003-1248-640X
https://orcid.org/0000-0003-1248-640X
Jonathan R. M. Kaplan, MD,  https://orcid.org/0000-0002-0821-7939
https://orcid.org/0000-0002-0821-7939
Tyler A. Gonzalez, MD, MBA,  https://orcid.org/0000-0002-3210-8097
https://orcid.org/0000-0002-3210-8097
References
- 1. Agostinho De Lima Gomes M, Monteiro GF, Neto JFA. Percutaneous surgery in the treatment of Haglund syndrome. J Foot Ankle. 2020;14(3):285-292. doi: 10.30795/jfootankle.2020.v14.1192 [DOI] [Google Scholar]
- 2. Biz C, Cerchiaro M, Belluzzi E, Bragazzi NL, De Guttry G, Ruggieri P. Long term clinical-functional and ultrasound outcomes in recreational athletes after Achilles tendon rupture: Ma and Griffith versus Tenolig. Medicina (Kaunas). 2021;57(10):1073. doi: 10.3390/medicina57101073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Black AT, So E, Combs A, Logan D. The Zadek osteotomy for surgical management of insertional Achilles tendinopathy: a systematic review. Foot Ankle Spec. 2023;16(4):437-445. doi: 10.1177/19386400231162411 [DOI] [PubMed] [Google Scholar]
- 4. Boffeli TJ, Peterson MC. The Keck and Kelly Wedge calcaneal osteotomy for Haglund’s deformity: a technique for reproducible results. J Foot Ankle Surg. 2012;51(3):398-401. doi: 10.1053/j.jfas.2012.03.002 [DOI] [PubMed] [Google Scholar]
- 5. Budiman-Mak E, Conrad KJ, Mazza J, Stuck RM. A review of the Foot Function Index and the Foot Function Index - Revised. J Foot Ankle Res. 2013;6(1):1-37. doi: 10.1186/1757-1146-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cengiz B, Karaoglu S. Clinical results of the Keck and Kelly Wedge osteotomy approach in Haglund’s deformity: minimum 3-year follow-up. Foot Ankle Surg. 2022;28(2):269-275. doi: 10.1016/j.fas.2021.10.006 [DOI] [PubMed] [Google Scholar]
- 7. Choi JY, Suh JS. A novel technique of minimally invasive calcaneal osteotomy for intractable insertional Achilles tendinopathy associated with Haglund deformity. Foot Ankle Orthop. 2022;7(4):2473011421S0061. doi: 10.1177/2473011421S00618 [DOI] [PubMed] [Google Scholar]
- 8. Cusumano A, Martinelli N, Bianchi A, Bertelli A, Marangon A, Sansone V. Transtendinous approach calcaneoplasty versus endoscopic calcaneoplasty for Haglund’s disease. Int Orthop. 2021;45(1):225-231. doi: 10.1007/S00264-020-04761-0 [DOI] [PubMed] [Google Scholar]
- 9. Dawson J, Boller I, Doll H, et al. Responsiveness of the Manchester-Oxford foot questionnaire (MOXFQ) compared with AOFAS, SF-36 and EQ-5D assessments following foot or ankle surgery. J Bone Joint Surg Br. 2012;94-B(2):215-221. doi: 10.1302/0301-620X.94B2.27634 [DOI] [PubMed] [Google Scholar]
- 10. deMeireles AJ, Guzman JZ, Nordio A, Chan J, Okewunmi J, Vulcano E. Complications after percutaneous osteotomies of the calcaneus. Foot Ankle Orthop. 2022;7(3):24730114221119731. doi: 10.1177/24730114221119731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Friesenbichler B, Rutishauser T, Monn S, et al. Ankle muscle strength and gait symmetry after dorsal closing wedge calcaneal osteotomy for Haglund exostosis. Swiss Medical Weekly. Published 2023. Accessed January 11, 2024. https://www.embase.com/records?subaction=viewrecord&id=L642088609 [DOI] [PubMed]
- 12. Ge Z, Ma L, Tang H, et al. Comparison of dorsal closing wedge calcaneal osteotomy versus posterosuperior prominence resection for the treatment of Haglund syndrome. J Orthop Surg Res. 2020;15(1):168. doi: 10.1186/s13018-020-01687-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Georgiannos D, Kitridis D, Bisbinas I. Dorsal closing wedge calcaneal osteotomy for the treatment of insertional Achilles tendinopathy: a technical tip to optimize its results and reduce complications. Foot Ankle Surg. 2018;24(2):115-118. doi: 10.1016/J.FAS.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 14. Georgiannos D, Lampridis V, Vasiliadis A, Bisbinas I. Treatment of insertional Achilles pathology with dorsal Wedge calcaneal osteotomy in athletes. Foot Ankle Int. 2016;38(4):381-387. doi: 10.1177/1071100716681139 [DOI] [PubMed] [Google Scholar]
- 15. Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. Wiley; 2019:1-694. doi: 10.1002/9781119536604 [DOI] [Google Scholar]
- 16. Kaplan J, Hall S, Schipper O, Vulcano E, Jackson B, Gonzalez T. Percutaneous Zadek osteotomy for insertional Achilles tendinopathy and Haglund’s deformity: a technique tip. Foot Ankle Int. 2023;44(9):931-935. [DOI] [PubMed] [Google Scholar]
- 17. Karjalainen PT, Soila K, Aronen HJ, et al. MR imaging of overuse injuries of the Achilles tendon. AJR Am J Roentgenol. 2000;175(1):251-260. doi: 10.2214/ajr.175.1.1750251 [DOI] [PubMed] [Google Scholar]
- 18. Keck S, Kelly P. Bursitis of the posterior part of the heel: evaluation of surgical treatment of eighteen patients. J Bone Joint Surg Am. 1965;47(2):267-273. Accessed March 28, 2023. https://journals.lww.com/jbjsjournal/Abstract/1965/47020/Bursitis_of_the_Posterior_Part_of_the_Heel_.3.aspx [PubMed] [Google Scholar]
- 19. Khan KM, Forster BB, Robinson J, et al. Are ultrasound and magnetic resonance imaging of value in assessment of Achilles tendon disorders? A two year prospective study. Br J Sports Med. 2003;37(2):149-153. doi: 10.1136/BJSM.37.2.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Klauser AS, Miyamoto H, Tamegger M, et al. Achilles tendon assessed with sonoelastography: histologic agreement. Radiology. 2013;267(3):837-842. doi: 10.1148/radiol.13121936 [DOI] [PubMed] [Google Scholar]
- 21. Kujala UM, Sarna S, Kaprio J. Cumulative incidence of Achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med. 2005;15(3):133-135. doi: 10.1097/01.jsm.0000165347.55638.23 [DOI] [PubMed] [Google Scholar]
- 22. López-Capdevila L, Santamaria Fumas A, Dominguez Sevilla A, et al. Dorsal wedge calcaneal osteotomy as surgical treatment for insertional Achilles tendinopathy. Rev Esp Cir Traumatol (Engl Ed). 2020;64(1):22-27. doi: 10.1016/j.recot.2019.09.004 [DOI] [PubMed] [Google Scholar]
- 23. Maffulli N, D’Addona A, Gougoulias N, Oliva F, Maffulli GD. Dorsally based closing wedge osteotomy of the calcaneus for insertional Achilles tendinopathy. Orthop J Sports Med. 2020;8(3):2325967120907985. doi: 10.1177/2325967120907985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Maffulli N, Gougoulias N, D’Addona A, Oliva F, Maffulli GD. Modified Zadek osteotomy without excision of the intratendinous calcific deposit is effective for the surgical treatment of calcific insertional Achilles tendinopathy. Surgeon. 2021;19(6):e344-e352. doi: 10.1016/j.surge.2020.08.018 [DOI] [PubMed] [Google Scholar]
- 25. Maffulli N, Saxena A, Wagner E, Torre G. Achilles insertional tendinopathy: state of the art. J ISAKOS. 2019;4(1):48-57. doi: 10.1136/JISAKOS-2017-000144 [DOI] [Google Scholar]
- 26. Mazura M, Goldman T, Stanislav P, Kachlik D, Hromadka R. Calcaneal osteotomy due to insertional calcaneal tendinopathy: preoperative planning. J Orthop Surg Res. 2022;17(1):1-5. doi: 10.1186/S13018-022-03359-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Movin T, Gad A, Reinholt FP, Rolf C. Tendon pathology in long-standing achillodynia: biopsy findings in 40 patients. Acta Orthop Scand. 1997;68(2):170-175. doi: 10.3109/17453679709004002 [DOI] [PubMed] [Google Scholar]
- 28. Nordio A, Chan JJ, Guzman JZ, Hasija R, Vulcano E. Percutaneous Zadek osteotomy for the treatment of insertional Achilles tendinopathy. Foot Ankle Surg. 2020;26(7):818-821. doi: 10.1016/j.fas.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 29. Oliva F, Marsilio E, Asparago G, et al. Achilles tendon rupture and dysmetabolic diseases: a multicentric, epidemiologic study. J Clin Med. 2022;11(13):3698. doi: 10.3390/jcm11133698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pi Y, Hu Y, Guo Q, et al. Open versus endoscopic osteotomy of posterosuperior calcaneal tuberosity for Haglund syndrome: a retrospective cohort study. Orthop J Sports Med. 2021;9(4):23259671211001055. doi: 10.1177/23259671211001055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Poutoglidou F, Drummond I, Patel A, Malagelada F, Jeyaseelan L, Parker L. Clinical outcomes and complications of the Zadek calcaneal osteotomy in insertional Achilles tendinopathy: a systematic review and meta-analysis. Foot Ankle Surg. 2023;29(4):298-305. doi: 10.1016/j.fas.2023.04.007 [DOI] [PubMed] [Google Scholar]
- 33. Rutishauser T, Stephan A, Rippstein P, Stadelmann VA. Patient reported outcome measures after dorsal closing wedge calcaneal osteotomy and removal of Haglund exostosis via central tendon splitting approach in patients with Haglund exostosis associated heel pain. Swiss Medical Weekly. Published 2023. Accessed January 11, 2024. https://www.embase.com/records?subaction=viewrecord&id=L642088316
- 34. Rutishauser T, Stephan A, Rippstein P, Stadelmann VA. Patient reported outcomes after dorsal closing wedge calcaneal osteotomy in patients with Haglund exostosis associated heel pain (11176). Swiss Medical Weekly. Published 2022. Accessed January 11, 2024. https://www.embase.com/records?subaction=viewrecord&id=L639180209
- 35. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. doi: 10.1046/J.1445-2197.2003.02748.X [DOI] [PubMed] [Google Scholar]
- 36. Tarantino D, Palermi S, Sirico F, Corrado B. Achilles tendon rupture: mechanisms of injury, principles of rehabilitation and return to play. J Funct Morphol Kinesiol. 2020;5(4):95. doi: 10.3390/jfmk5040095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tourne Y, Baray AL, Barthelemy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: clinical results and a radiographic analysis to explain its efficacy. Foot Ankle Surg. 2022;28(1):79-87. doi: 10.1016/j.fas.2021.02.001 [DOI] [PubMed] [Google Scholar]
- 38. Tourné Y, Francony F, Barthélémy R, Karhao T, Moroney P. The Zadek calcaneal osteotomy in Haglund’s syndrome of the heel: its effects on the dorsiflexion of the ankle and correlations to clinical and functional scores. Foot Ankle Surg. 2022;28(6):789-794. doi: 10.1016/j.fas.2021.11.001 [DOI] [PubMed] [Google Scholar]
- 39. von Rickenbach KJ, Borgstrom H, Tenforde A, Borg-Stein J, McInnis KC. Achilles tendinopathy: evaluation, rehabilitation, and prevention. Curr Sports Med Rep. 2021;20(6):327-334. doi: 10.1249/JSR.0000000000000855 [DOI] [PubMed] [Google Scholar]
- 40. Wang CL, Chen PY, Yang KC, Wu HC, Wang CC. Ultrasound-guided minimally invasive surgical resection of retrocalcaneal bursitis: a preliminary comparison with traditional open surgery. J Foot Ankle Surg. 2019;58(5):855-860. doi: 10.1053/j.jfas.2018.12.023 [DOI] [PubMed] [Google Scholar]
- 41. Wendler DE, Stewart GW, Bailey EJ, Shofoluwe AI, Nwaibu U. Minimally invasive foot & ankle surgery: a review and a novel technique. Foot Ankle Orthop. 2022;7(4):2473011421S01001. doi: 10.1177/2473011421S01001 [DOI] [Google Scholar]
- 42. Wiegerinck JI, Kok AC, Van Dijk CN. Surgical treatment of chronic retrocalcaneal bursitis. Arthroscopy. 2012;28(2):283-293. doi: 10.1016/j.arthro.2011.09.019 [DOI] [PubMed] [Google Scholar]
- 43. Xu Y, Haider ZA, Karuppiah V, Dhar S. Zadek osteotomy, a good treatment option for refractory Haglund’s deformity. Cureus. 2023;15(5):e39497. doi: 10.7759/cureus.39497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zadek I. An operation for the cure of achillobursitis. Am J Surg. 1939;43:542-546. doi: 10.1016/S0002-9610(39)90877-9 [DOI] [Google Scholar]
- 45. Zheng W, Du J, Liang J, Zhang Y, Liang X, Zhao H. Zadek osteotomy for the treatment of Haglund’s syndrome. Preprint. Published online June 23, 2020. Research Square. doi: 10.21203/rs.3.rs-37115/v1 [DOI] [Google Scholar]
- 46. Zhi X, Liu X, Han J, et al. Nonoperative treatment of insertional Achilles tendinopathy: a systematic review. J Orthop Surg Res. 2021;16(1):1-12. doi: 10.1186/S13018-021-02370-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114241241320 for Percutaneous vs Open Zadek Osteotomy for Treatment of Insertional Achilles Tendinopathy and Haglund’s Deformity: A Systematic Review by Yianni Bakaes, SarahRose Hall, J. Benjamin Jackson, A. Holly Johnson, Oliver N. Schipper, Ettore Vulcano, Jonathan R. M. Kaplan and Tyler A. Gonzalez in Foot & Ankle Orthopaedics