Abstract
Elephantiasis nostras verrucosa (ENV) is a rare complication of chronic lymphedema, leading to progressive cutaneous hypertrophy and disfigured lower extremities. We present an unusual case of a 79-year-old man with ENV, who had an episode of erysipelas treated and cured with antibiotics. The patient presented with progressive painless lymphedema of the lower limb years ago, complicated with skin changes. The biology and radiology test does not objective any causes. The compression therapy was proposed to the patient. ENV is characterized by lymphedema and skin anomaly. Management of ENV is often challenging, but a variety of successful medical and surgical treatment strategies have been reported.
Keywords: elephantiasis nostras verrucosa, lymphatic system, compression therapy
Introduction
Elephantiasis nostras verrucosa (ENV) is a rare complication of the chronic obstruction of the lymphatic system. Many causes, such as tumor obstruction, radiation trauma, hypothyroidism, chronic venous stasis, and some infections, except filariasis, can lead to the development of ENV.
We report a case of ENV and present a review of the literature to discuss the epidemiologic, diagnostic, therapeutic, and evolutionary aspects of this pathology.1) The few cases discussed had in common the elementary lesions in dermatological semiology such as nodules, hyperkeratosis, cobblestone appearance, and nonpitting edema. There are no guidelines for this pathology, some physicians treat their patients with contention and observe the improvement of their symptoms, others prefer wound care, and few staff members use surgical procedures. Concerning pathogenicity, the most common hypothesis is a vicious cycle of recurrent infection and swelling that causes inflammation of lymphatic vessels, which increases lymphatic stasis. Consequently, fibroblasts and collagen proliferate on the skin. Almost all of the organisms that cause these disorders are streptococcal infections, more than staphylococcal. The finding that some risk factors can increase this disease should prompt primary care health professionals to make the diagnosis earlier for a better result and to prevent this complication.
Case Report
A 79-year-old man presented to the emergency department with progressive swelling and heaviness of the lower limbs, which had evolved over the past four years. He did not complain of any other symptoms. His medical, surgical, travel, and family histories were unremarkable. He described this disease as not painful, but it had been bothering him a lot, to the point that he could not wear shoes or walk properly anymore. The patient mentioned that he had a soft tissue infection of the same limb treated with antibiotics a few years ago.
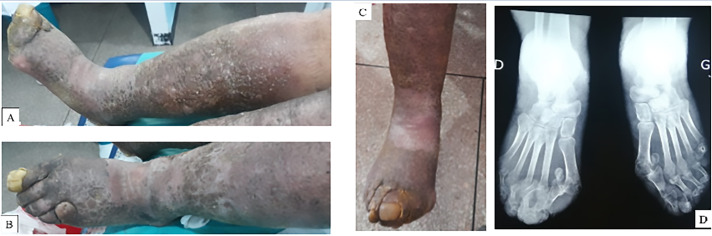
On physical examination, his lower extremities had a discrete edema localized on the feet, with lichenification of the entire limb. The skin was indurated and had cobblestone-like papulonodules and crusts (Figs. 1A and 1B). In addition, we observed a superficial ulcer on the medial side of the left leg, exactly on the supramalleolar area. Moreover, the bones of the toes of his both feet were deformed (Fig. 1C). Palpation of the lower limb pulses was impossible because of skin induration. His weight was 90 kg, and his height was 169 cm.
Fig. 1 (A) Crusts and cobblestone-like papulonodules on the right leg, (B) swelling and cobblestone-like papulonodules on the left leg, (C) deformation of the toes, and (D) X-ray showing bone architecture deformation.
Complete blood count (CBC), C-reactive protein and blood sugar levels, and liver and renal function tests were within the normal range. Lower extremity venous ultrasound ruled out the presence of deep and superficial vein thrombosis.
Feet X-ray revealed bone architecture deformation and subluxation at the metatarsophalangeal joint (Fig. 1D). Magnetic resonance imaging and radionuclide lymphoscintigraphy were prescribed but were not conducted because the patient does not have any health insurance. On the basis of this result, we eliminated all other organic pathology, and the final diagnosis was ENV.
The patient was managed with compression therapy and a sterile dressing for his ulcer. In addition, we educated him and encouraged him to increase ambulation, elevate his legs, and reduce his body weight. However, his symptoms did not substantially improve because of poor treatment compliance. He was given an appointment, but the patient did not come back to his next appointments.
Discussion
ENV is a rare complication of the chronic obstruction of the lymphatic system, often as a result of an untreated chronic nonfilarial infection. This disease causes abnormal enlargement and deformation of the lower limb, resulting in severe disability and social stigma.
There are only a few reports of ENV worldwide. In Table 1, we summarize the literature on ENV of the lower legs not related to tropical elephantiasis.
Table 1 The differential diagnosis of ENV.
| Diagnosis | Presentation |
|---|---|
| Lymphatic filariasis | Bacterial infection, tropical region. Lymphedema, hydrocele, hyperkeratosis, nodule, and papillomatous hyperplasia. Stemmer sign. Intertrigo, ulcers. |
| Lipedema | Accumulation of fat. In the low part of body, sparing the feet. Bilateral, symmetrical. Negative Stemmer sign. No epidermal changes. |
| Lipodermatosclerosis | Venous stasis. Hyperpigmentation. Proximal leg edema and distal swelling. Inverted bottle appearance. |
| Papular mucinosis | Waxy papules and plaques. Slightly reddish or skin-colored, dome-shaped, or flat papule. |
| Pretibial myxedema | Thyroid dermopathy. Plaques on the anterior tibia and dorsum of the feet. Pink or purple-brown papules or nodules, nonpitting edema. |
| Stewart–Treves syndrome | Angiosarcoma. Purple-red papule. Complications: edema, ulceration, infection, hemorrhage. |
The pathophysiology of ENV is still not clear, but it was observed that the chronic accumulation of the lymph and protein-rich interstitial fluid in the tissues increases the volume of the limb and causes tissue deformations. Many cases develop lymphangitis due to fibroblast proliferation, which causes the fibrosis of the dermis and subcutaneous tissues, which decreases the local immune system. As the infection-associated inflammation leads to the fibrosis of the lymphatic system, lymphedema progresses.2)
Many etiologies can cause chronic lymphatic obstruction, such as tumor obstruction of lymph nodes, trauma, radiation, infection, and chronic venous stasis. Some risk factors are determined, such as obesity, type 2 diabetes, a history of infection, and a low socio-cultural level.
In 1969, Castellani3) described and classified elephantiasis into four subtypes:
1) Elephantiasis tropica—due to filariasis.
2) Elephantiasis nostras—due to infection.
3) Elephantiasis symptomatica—due to mycotic, syphilitic, tuberculoid, neoplastic, or traumatic causes of lymphatic obstruction.
4) Elephantiasis congenita—associated with inherited disorders such as Milroy’s disease.
The diagnosis of ENV is based on the history of the patient, physical examination, and characteristic skin findings: hyperkeratosis, dermal fibrosis, and nodules that have a cobblestone appearance. The skin may develop a malodorous smell due to chronic colonization by bacteria and fungi. On the basis of the clinical findings only, the characteristic physical signs found in ENV are limb swelling, lichenification, and indurated cobblestone-like papulonodules, a sign of Kaposi–Stemmer.4)
The differential diagnosis of ENV must be eliminated, as lipedema, lipodermatosclerosis, papular mucinosis, papillomatosis cutis carcinoides, pretibial myxedema, Stewart–Treves syndrome (Table 1).
Complementary exams like standard blood test or venous ultrasound can help in determining the cause of chronic lymphatic obstruction. Some physicians conduct skin biopsy to search for architectural anomalies, and others conduct lymphoscintigraphy to evaluate the lymphatic system. In our case, there was no history of familial and filarial lymphedema. Recurrent infections reported by the patient could be the only cause of this complication, including the risk factor that he had. Currently, there are no analyses used to assess the significance of different factors that could cause or increase this clinical situation.
There are no consensus and no guideline for treating ENV. Early diagnosis may yield satisfying results and may make the treatment less difficult.
Compression therapy is the main treatment with the best results because it reduces capillary filtration, minimizes the accumulation of fluid, and improves lymphatic transport capacity.
Extremity amputation may be indicated if there is severe limb deformation or infection.
The recommendations for reducing the swelling of lymphedema–elephantiasis are4) the following:
1) Limb elevation
2) Manual lymphatic drainage
3) Pneumatic compression devices
4) Multilayer lymphedema bandaging
5) Compression garments
6) Exercise.
The other treatments that can be used in ENV are skin debridement and managing the underlying disease. In the literature, they related the following to managing ENV:
1) Hyperkeratosis is treated locally using 5% salicylic ointment.
2) Antifungal drugs are applied locally in cases of fungal infection but for a short time.
Damstra et al.5) described 28 patients with primary lymphedema and ENV. Almost all had episodes of erysipelas. They treated them with surgery and strict use of compression garments and toecaps.
For surgery management, some surgery proposes different techniques. Coriddi et al.6) used lymph nodes transplanted on 15 patients with secondary lymphedema, which improved their symptomatology.
Kibadi et al.7) managed a female patient suffering from elephantiasis of an ulcerated leg with fascio-lymphangiectomy and preservation of the skin, combined with compression therapy. The result was satisfactory, and the patient can use shoes and can move normally.
Motegi et al.8) treated their patients with lymphaticovenular anastomosis; one of the presented with ENV of the lower leg. They reported a remarkable improvement in skin lesions and a reduction of lymphedema.
Turhan et al.9) reported a patient with ENV complicated by chronic tibial osteomyelitis because of the severe infection of the soft tissues surrounding the tibia, and after evaluating all treatment modalities, they decided to amputate the leg.
In Table 2, we summarize the main features of the cases reported in the literature.
Table 2 Features of elephantiasis nostras verrucosa reported in the literature.
| References | Age/ Gender | Physical exam | Medical history | Biology test | Radiology test | Treatment | Evolution |
|---|---|---|---|---|---|---|---|
| Samanci NS, Poturoglu S. Elephantiasis nostras verrucosa. The Indian Journal of Medical Research 2017 June | 41 YO M | - Pain, Bad smell - Deformity - Bilateral swelling on the lower limbs - Edema, plaques - Lichenification - Indurated cobblestone-like papulonodules | - No family history - Diabetes type 2 - Nephropathy - Morbid obesity - Hypertension - Congestive heart failure - Received antibiotic therapy | - Blood test: normal - Sedimentation: 117 mm/h | Lymphoscintigraphy: occlusion of lymphatic channels | - Antibiotic - Furosemide - Elevate legs - Reduce body weight - Resection of the hypertrophied areas | Was lost |
| Mansur AT et al. A case of elephantiasis nostras verrucosa treated successfully by a new type of compressive garment. Dermatol Ther. 2020 | 69 YO M | - Edema, Lymphorrhea - Dusky red color - Multiple verrucous - Brownish-red papulonodules with cobblestone-like - Scattered superficial | - No family history - Diabetes type 2 - Deep venous thrombosis of the right leg | - Blood cell count, thyroid function test, blood biochemistry: Normal - C-reactive protein: 15.07 mg/l | - Venous color-doppler sonography of the right lower extremity: Thrombosis, and subcutaneous edema left lower extremity | -Topical keratolytic -Two-layer bandage twice a week then four-layer bandage then low-stretch compression garment | Verrucous papulonodules regressed almost totally Reduction in edema |
| Santiago L. et al. A Case of exuberant elephantiasis nostras verrucosa. Acta Med Port. 2017 May | 76 YO W | - Heard failure - Chronic venous insufficiency - Secondary lymphedema associated to bilateral cellulitis | - Nonpitting edema - Foul-smelling mossy plaques - Cobblestone-like nodules in both legs | Skin biopsy: Hyperkeratosis of the epidermis with underlying dilated lymphatics | Venous doppler studies: No evidence of deep vein thrombosis | - Leg elevation - Diuretics - Compression - Topical keratolytic - Debridement | Great |
| Duckworth AL et al. Elephantiasis nostras verrucosa or “mossy foot lesions” in lymphedema praecox: report of a case. J Am Podiatr Med Assoc. 2008 Jan–Feb | 32 YO W | - Malodor, no pain - Minor discomfort with certain shoes - Lymphedema - Non pitting edema, no open lesions, no signs of infection on the legs- Lichenification, papules and nodules | Cesarean section | Skin biopsy: Verrucous, hyperkeratosis, papillomatosis Dermis: fibrotic between numerous dilated lymphatic | |||
| Lee EY, Sia CH Visual Dermatology: Elephantiasis Nostras Verrucosa. J Cutan Med Surg. 2021 Mar-Apr | 46 YO M | - Non pitting edema - Hyperkeratosis - Lichenified crusted papillomatous plaques - Cobblestone nodules | Chronic lymphedema - Recurrent cellulitis | Blood filariasis microscopy and serology negative | Scintigraphy: Partial lymphatic obstruction | ||
| Hagen TL. Elephantiasis nostras verrucosa [Elephantiasis nostras verrucosa]. Ugeskr Laeger. 2015 Dec | 76 YO W | - Fever - Hyperkeratotic skin - Hyperpigmentation - Cobblestone nodules - Ulcer, malodor | - Obesity - Chronic venous stasis | C-reactive protein 504 nmol/L | Venous doppler studies: No evidence of deep vein thrombosis, no abscess | - Bath of permanganate of potassium - Debridement - Antibiotic | Bonne evolution |
| Luciano et al. Elephantiasis nostras verrucosa. Journal of Hospital Medicine, 2009, vol. 4, no 7 | 79 YO W | - Afebrile, no adenopathy - Bilateral lower extremity edema - Hyperpigmented - Cobble-stoned - Hyperkeratotic skin - Verrucous nodules on the inner thighs | - Heart failure - Morbid obesity - Chronic lymphedema - Deep vein thrombosis with inferior vena cava filter placement | - Compression stocking - Topical emollients | |||
| Hernandez et al. Elefantiasis verrucosa nostra. Atención Primaria, 2019, vol. 51, no 8, p. 521 | 73 YO M | - Bilateral swelling on the lower limbs - Edema - Papules confluentes - Cobblestones nodules - Sign for Kaposi–Stemmer | - Obesity - Hypertension - Diabetes type 2 - Hypercholesterolemia - Bilateral pulmonary thromboembolism | ||||
| Shah M. et al. Images in clinical medicine. Elephantiasis nostras verrucosa. N Engl J Med. 2014 Jun | 49 YO W | - Extensive areas of redness - Weeping sores on her legs - Hyperkeratosis, ulcer - Papillomatous plaques - Loosely adherent crust - Cobblestone-like nodules | - Morbid obesity - Hypertension - Chronic venous stasis - Lymphedema | Venous doppler studies: No evidence of deep vein thrombosis | - Wound care - Antimicrobial therapy | Improved | |
| Freitas A. et al. Elephantiasis nostras verrucosa secondary to recurrent erysipelas. BMJ Case Rep. 2017 Aug | 79 YO M | - Edema, exophytic - Nausea, Prostration, Fever - Lesions of a mossy and verrucose appearance - Agglomerated lesions | - Several episodes of erysipelas - Chronic venous insufficiency - Diabetes type 2 | - Furosemide - Heparin - Antibiotic | |||
| Hadi Y. et al. Elephantiasis nostras verrucosa: an atypical presentation following intrapelvic lymphoma. Dermatol Online J. 2019 Dec | 72 YO M | - Verrucous - Weeping cysts - Nodules of the bilateral legs - No ulcers | - Edema, Ulceration - Intrapelvi lymphoma, Intrapelvic non hodgkin follicular B cell lymphoma status post-remission with chemotherapy - Hypogammaglobulinemia - Morbid obesity | - Thyroid stimulating hormone: Normal - Serum IgG: Decreased - kidney and liver : Normal | - Echocardiogram: no heart failure - Venous deplex reflux studies displayed superficial cystic lesions consistent with lymphatic ectasia bilaterally and evidence of superficial venous reflux with involving the greated saphenous vein in the right lower leg | - Compressive - Lymphatic pump at home | |
| Pérez-Rodrigez IM et al. Elephantiasis nostras verrucosa as a manifestation of morbid obesity. BMJ Case Rep. 2014 Nov | 48 YO M | - Edema - Hyperpigmentation - Hyperkeratosis - Verrucous aspect | - Morbid obesity - Atrial fibrillation - Abdominoplasty | Skin biopsy: - Hyperkeratosis, Papollomatosis - Proliferation, Dermal fibrosis - Dilatation of blood vessels and lymphatics | Died days after admission from heart complications and sepsis | ||
| Yang YS et al. A case of elephantiasis nostras verrucosa. Ann Dermatol. 2009 Aug | 67 YO M | - Hard papules and plaques on both feet - Confluent brownish verrucous papules and plaques with a moss-covered appearance surrounding the peripheries of both feet | - Habit of drinking rawdeer blood - Hospitalized several times for recurrent cellulitis of both feet - Type 2 diabetes | - Mildly elevated erythrocyte sedimentation rate - Glucose 193 mg/dl - Test for microfilaria resulted in negative findings | - Lower extremity computed tomographic angiography: Varicose veins with early venous drainage at both feet and ankles - Skin biopsy: Hyperkeratosis and pseudoepitheliomatous hyperplasia channels | - Oral etretinate - Topical salicylic acid | - Little improvement after 3 months - Patient refuse any interventions of the venous problem - Lost to follow-up |
| Nwabudike L.C. et al. An integrative therapeutic approach to elephantiasis nostras verrucosa: A case report. Exp Ther Med. 2022 Apr | 72 YO W | - Erythema - Oozing excoriation of the legs with deep fold and creases | - Pedal edema - No history of infections, cardiac, renal, thyroid or hepatic disease | - Anemia - Renal impairment - Hypoalbuminemia | - Furosemide - Apocynum cannabinum | Decrease of the limb diameter Lost to follow-up | |
| Lo Schiavo A. et al. Elephantiasis nostras verrucosa in a patient with obesity and chronic venous insufficiency. Int J Dermatol. 2013 Apr | 62 YO W | - Brown-colored nonpitting edema - Multiple nodular verrucous lesions Cobblestone-like | - No personal history of flariasis or familiar milroy’s disease - Obesity - Venous insufficiency | ||||
| IWao F. et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004 Jun | 42 YO M | - Verrucous Cobblestone-like lesions - Hyperkeratotic - Malodorous | - Paralysis poliomyelitis - Never suffered from filariasis - No family history of familial lymphedema (milroy’s disease) | Skin biopsy: Hyperkeratosis, acanthosis, fibrosis of the dermis, numerous dilated lymphatic capillaries | - Topical, Dermabrasion - Electrocoagulation - Antiobiotic - Elevated position - Compression stocking | Good | |
| Shimbo K. et al. Hybrid Treatment Combining Lymphaticovenous Anastomoses and the Oriental Herbal Medicine Bofutsushosan for Obesity-Associated Lower Leg Elephantiasis Nostras Verrucosa: A Case Report. Int J Low Extrem Wounds. 2021 Sep | 79 YO W | - Nonpitting edema of both lower legs - Multiple nodular verrucous lesions - Ulceration on the loft foot | - Orthopedic disease - Mobid obesity | - Laboratory test results were normal - Minimal elevation of C-reactive protein | - Ultrasonography and contrast-enhanced computed tomography of the lower extremity: Edema and non venous involvement - Skin biopsy: Hyperkeratosis, acanthosis | - Bofutsushosan - Lymphatico-venous anastomoses - Debridement - Compression stocking - Lost weight | Good |
| Han HH et al. Successful Surgical Treatment for Elephantiasis Nostras Verrucosa Using a New Designed Column Flap. Int J Low Extrem Wounds. 2015 Sep | 51 YO F | - Sign for Kaposi–Stemmer - Verrucous and cobblestone-like lesions | - Omental transposition with superficial lymphangectomy of right leg lymphangitis | Debridement | |||
| Khetarpal A. et al. Elephantiasis nostras verrucosa: a severe complication of lymphoedema. Br J Hosp Med (Lond). 2020 May | 59 YO M | - Hyperkeratotic - Verrucous lesions - Papollomatous plaques | - Compression bandaging - Emollient - Antifungal | Improvement of skin | |||
| Fredman R. et al. Elephantiasis nostras verrucosa. Eplasty. 2012 | 53 YO W | - Fever - Nonpitting - Malodorous - Hyperpigmentation - Cobblestone-like lesions | - Morbid obesity - Recurrent cellulitis - Erysipelas - osteomyelitis | ||||
| Simon L.J. et al. Elefantiasis verrucosa nostras en paciente afectado de trastorno depresivo mayor. SEMERGEN-Medicina de Familia, 2012, vol. 38, no 8, p. 526-529 | 40 YO M | - Venous insufficiency - Major depressive disorder | - Debridement - Conservative measures | ||||
| Damani Z. et al. Elephantiasic Pretibial Myxedema. J Cutan Med Surg. 2022 May–Jun | 68 YO M | - Febrile, hypotention, tachycardia - Swelling - Hyperpigmentation Keratotic papules and plaques - Malodorous | - Atrial fibrillation - Morbi obesity - Heart failure - Venous stasis dermatitis | - Diuretic |
M: man; W: woman; YO: years old
Conclusion
ENV is a rare pathology characterized by spectacular limb deformation as a consequence of chronic lymphatic obstruction. This condition must be recognized and treated early to avoid limb deformation and loss.
Informed Consent Statement
Consent was obtained from the patient for the publication of this report, including the use of images.
Disclosure Statement
The authors declare no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Author Contributions
Study conception: all authors
Data collection: all authors
Writing: all authors
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Liaw FY, Huang CF, Wu YC, et al. Elephantiasis nostras verrucosa: swelling with verrucose appearance of lower limbs. Can Fan Physician 2012; 58: e551-3. [PMC free article] [PubMed] [Google Scholar]
- 2).Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol 2008; 9: 141-6. [DOI] [PubMed] [Google Scholar]
- 3).Castellani A. Researches on elephantiasis nostras and Elephantiasis tropica with special regard to their initial stage of recurring lymphangitis (lymphangitis recurrens elephantogenica). J Trop Med Hyg 1969; 72: 89-97. [PubMed] [Google Scholar]
- 4).Grada AA, Phillips TJ. Lymphedema: pathophysiology and clinical manifestations. J Am Acad Dermatol 2017; 77: 1009-20. [DOI] [PubMed] [Google Scholar]
- 5).Damstra RJ, Dickinson-Blok JL, Voesten HG. Shaving technique and compression therapy for elephantiasis nostras verrucosa (Lymphostatic verrucosis) of forefeet and toes in end-stage primary lymphedema: a 5 year follow-up study in 28 patients and a review of the literature. J Clin Med 2020; 9: 3139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Coriddi M, Wee C, Meyerson J, et al. Vascularized jejunal mesenteric lymph node transfer: a novel surgical treatment for extremity lymphedema. J Am Coll Surg 2017; 225: 650-7. [DOI] [PubMed] [Google Scholar]
- 7).Kibadi K. Treatment of elephantiasis of the leg by fasciotomy and lymphangiectomy with skin preservation in a resource-limited setting: a case report and review. Med Sante Trop 2018; 28: 33-6. [DOI] [PubMed] [Google Scholar]
- 8).Motegi S, Tamura A, Okada E, et al. Successful treatment with lymphaticovenular anastomosis for secondary skin lesions of chronic lymphedema. Dermatology 2007; 215: 147-51. [DOI] [PubMed] [Google Scholar]
- 9).Turhan E, Ege A, Keser S, et al. Elephantiasis nostras verrucosa complicated with chronic tibial osteomyelitis. Arch Orthop Trauma Surg 2008; 128: 1183-6. [DOI] [PubMed] [Google Scholar]