Abstract
Introduction
Robotic-arm-assisted unicompartmental knee arthroplasty (UKA) is an excellent solution for patients suffering from single-compartment knee arthritis. While outcomes tend to be favorable for UKAs, revision operations, commonly due to component malpositioning and malalignment resulting in accelerated wear, are a major concern. Intraoperative technologies, such as robotic assistance, can help better ensure that implants are positioned based on a patient's specific anatomy and mechanical physiology. However, long-term survivorship and patient-reported satisfaction with robotic-assisted UKAs are limited. Therefore, the purpose of this study was to assess the 10-year outcomes of patients who underwent robotic-arm-assisted unicompartmental knee arthroplasty. Specifically, we evaluated: 1) 10-year survivorships; 2) patient satisfaction scores; and 3) re-operations.
Methods
From a single surgeon and single institution, 185 patients who had a mean age of 65 years (range, 39 to 92) and a mean body mass index of 31.6 (range, 22.4 to 39) at a mean of 10 years follow-up were evaluated (range, 9 to 11). For all patients, the same robotic-assistive device was utilized intraoperatively, and all patients underwent standardized physical therapy and received standardized pain control management. Then 10-year survivorships with Kaplan-Meir curves, patient satisfaction evaluations with a 5-point Likert scale, and re-operations were assessed as primary outcomes.
Results
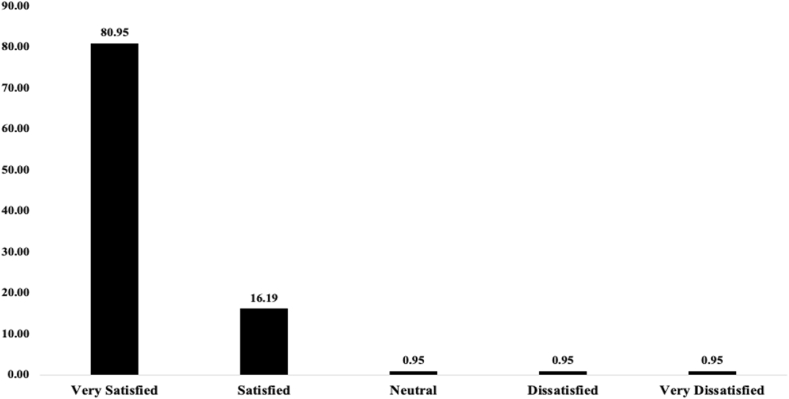
Overall implant survivorship was 99%, with only two patients requiring revision surgery. There was one patient who was converted to a total knee arthroplasty, while the other patient underwent polyethylene exchange at 5 weeks for an acute infection with successful implant retention. Overall, 97% of the patients were satisfied with their postoperative outcomes, with 81% of patients reporting being very satisfied. There were two other patients who required arthroscopic intervention: one to remove a cement loose body, the other to remove adhered scar from the fat pad and the anterior cruciate ligament.
Conclusion
This study is one of the first to provide longer-term (mean 10-year) survivorship and patient-reported satisfaction outcomes for robotic-assisted UKA patients. These data show strong support for utilizing this surgical technique, as nearly all patients maintained their original prostheses and reported being satisfied after a mean of 10 years. Therefore, based on these results, we recommend the use of robotic assistance when performing UKAs.
Keywords: Robotic-assisted, Unicompartmental knee arthroplasty, 10-year outcomes, Patient satisfaction, Implant survivorship, Revision surgery
1. Introduction
Unicompartmental knee arthroplasty is an excellent solution for patients suffering from debilitating arthritic pain isolated to a single compartment. Although not as robust as TKA, UKAs have shown good long-term survivorship, with some studies reporting 85% at a minimum of 10 years 1,2,3,4 Beyond long-term survivorship, UKAs are potentially associated with quicker postoperative recoveries, decreased blood losses, and lower rates of peri-prosthetic joint infections (PJIs) compared to total knee arthroplasty (TKA).5 Most notably, UKAs can preserve more normal knee kinematics by preserving both the anterior and posterior cruciate ligaments as compared to TKAs. Despite their advantages, UKAs commonly require revision due to aseptic loosening, progression of arthritis to other compartments of the knee, and component wear.6,7 A major contributing factor to the above reasons for revision is potential component malalignment, which can lead to contralateral compartment overloading, accelerated polyethylene wear, and gait imbalances.8 Therefore, optimal component alignment and placement for each unique patient is critical to ensuring longer-term survivorship and patient satisfaction (see Fig. 8).
Fig. 8.
Post-operative patient satisfaction.
To help surgeons achieve more optimal component positioning, a number of intraoperative technologies for this surgery have been developed. One particular technological advancement is using an assistive robotic arm. This device can help ensure appropriate knee balancing as well as component placement. The robotic device uses a preoperative computed tomography scan (CT scan) to assess pertinent bony landmarks, which are then registered in the operating room to provide real-time haptic feedback while sawing or burring bone. The controlled bony resection has been shown to result in decreased surrounding soft-tissue damage.9,10,11 While some studies have reported 3–5 year short-term to mid-term advantages of this technology in the setting of UKAs, less is known about the potential longer-term (10-year or longer) benefits.
Given the continued upswing in technology utilization in the operating room, specifically robotic assistance, it is imperative that we continue to evaluate patient outcomes in order to critique our current usage and build upon improved future surgical techniques. Therefore, the purpose of this study was to assess the mean 10-year outcomes of patients who underwent robotic-arm-assisted unicompartmental knee arthroplasty. Specifically, we evaluated: 1) 10-year survivorships; 2) patient satisfaction scores; and 3) re-operations.
2. Methods
2.1. Patient Selection
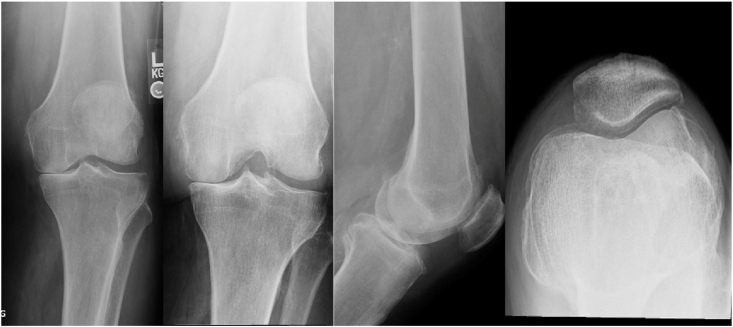
All patients who underwent robotic-assisted UKAs by a single surgeon at a single institution were evaluated. Patients were included if they met the following inclusion criteria: 1) age 30–90 years; 2) body mass index (BMI) < 40; 3) correctible varus alignment (<10° varus); 4) range of motion: 0 to 10–100°; 5) intact anterior cruciate ligament (ACL) as well as intact medial and lateral collateral ligaments; 6) non-inflammatory arthritis; 7) Grade 4 medial compartment wear on weight-bearing x-rays with subchondral sclerosis (see Fig. 1); 8) preserved lateral compartment joint space; 9) central tracking patella with no lateral patello-femoral degenerative changes; and 10) femur centrally positioned on the tibia on the lateral view. The final query yielded 185 patients, who had a mean age of 65 years (range, 39 to 92) and a mean body mass index (BMI) of 31.6 (range, 22.4 to 39.6) at a mean follow-up period of 10 years (range, 9 to 11).
Fig. 1.
Preoperative standing Antero-Posterior (AP), Postero-Anterior (PA), Lateral, and Sunrise view X-rays.
2.2. Surgical technique
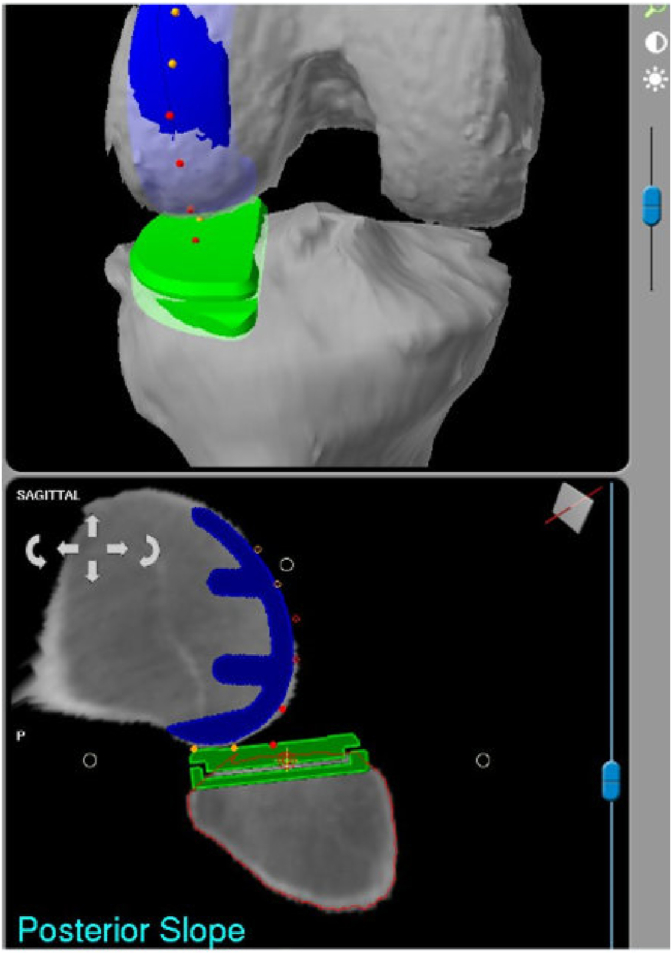
A preoperative computed tomography (CT) scan was obtained for each patient, which was segmented and utilized to define the hip–knee–ankle center as well as the anatomic osseus dimensions of the knee. The surgeon virtually selected the appropriate implant size and position related to the patient's tibial plateau and femoral condyle. The sagittal slope was recreated (up to 8 degrees of flexion), and the coronal varus inclination was maintained (up to 2.5 degrees of varus). The tibia was evaluated to obtain cortical rim contact, maintain <5 mm of bone resection, avoid ACL undermining, and maintain the joint line. The femur was positioned to recreate the sagittal and coronal positioning of the femoral condyle.
The surgical procedure was performed with an incision on the medial aspect of the proximal patella, 2 cm below the tibial plateau. The knee was entered through the medial capsule without incising the vastus medialis oblique muscle. The patello-femoral joint, lateral compartment, and ACL were inspected.
Femoral and tibial diaphyseal unicortical pins were placed, and image-based navigation was utilized to register the axial alignment and the patient's anatomy to their CT scan. The robotic software validated the accuracy of the registration, and the surgeon removed any osteophytes impinging on the medial soft tissue.
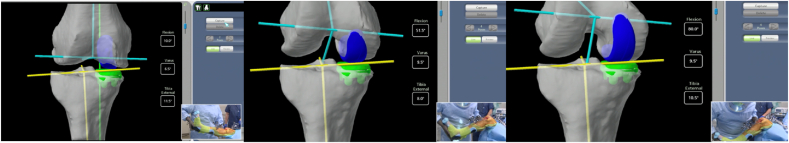
The knee was taken through full range of motion with varus and valgus stresses applied to assess gaps (see Fig. 2). Utilizing the robotic software, the implants were virtually adjusted to achieve a 1 mm gap across the bony interfaces. The tibia was never resected beyond 5 mm. Soft-tissue gap balance defined the depth of the femoral implant, and commonly, the tip of the femoral component was buried beneath the cartilage surface.
Fig. 2.
Varus and valgus stresses applied at 10, 50, and 90°.
The contact points were then evaluated to confirm the central articulation of the implants, and any adjustments were performed to achieve congruency through a full range of motion (see Fig. 3).
Fig. 3.
Red points confirm tibio-femoral congruency.
The robotic arm was registered, and the irrigated high-speed burr with haptic control was utilized to perform the bony resections for the implant volume on the femur and tibia. The surgeon visualized the cutting action in three different planes in real-time as the stereotactic interface constrained the surgeon to the field of bone preparation.
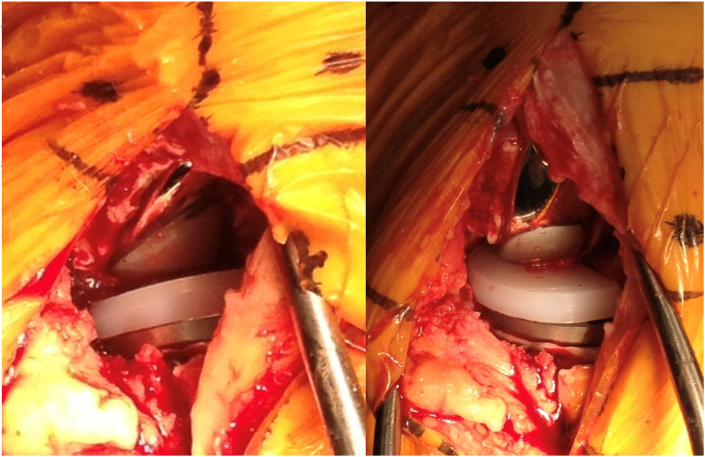
The medial meniscus was then resected, and any remaining osteophyte remnants were removed. The trial implants were seated, and the knee was clinically evaluated (see Fig. 4). The final coronal alignment was captured on the robotic software, and the kinematic tracking and laxity stresses were assessed. The final implants were cemented, and the final polyethylene insert was then locked into the tibial tray (see Fig. 5, Fig. 6). The wound was closed, and an aseptic dressing was applied (see Fig. 7).
Fig. 4.
Final implant in full extension and flexion.
Fig. 5.
Postoperative AP and lateral views.
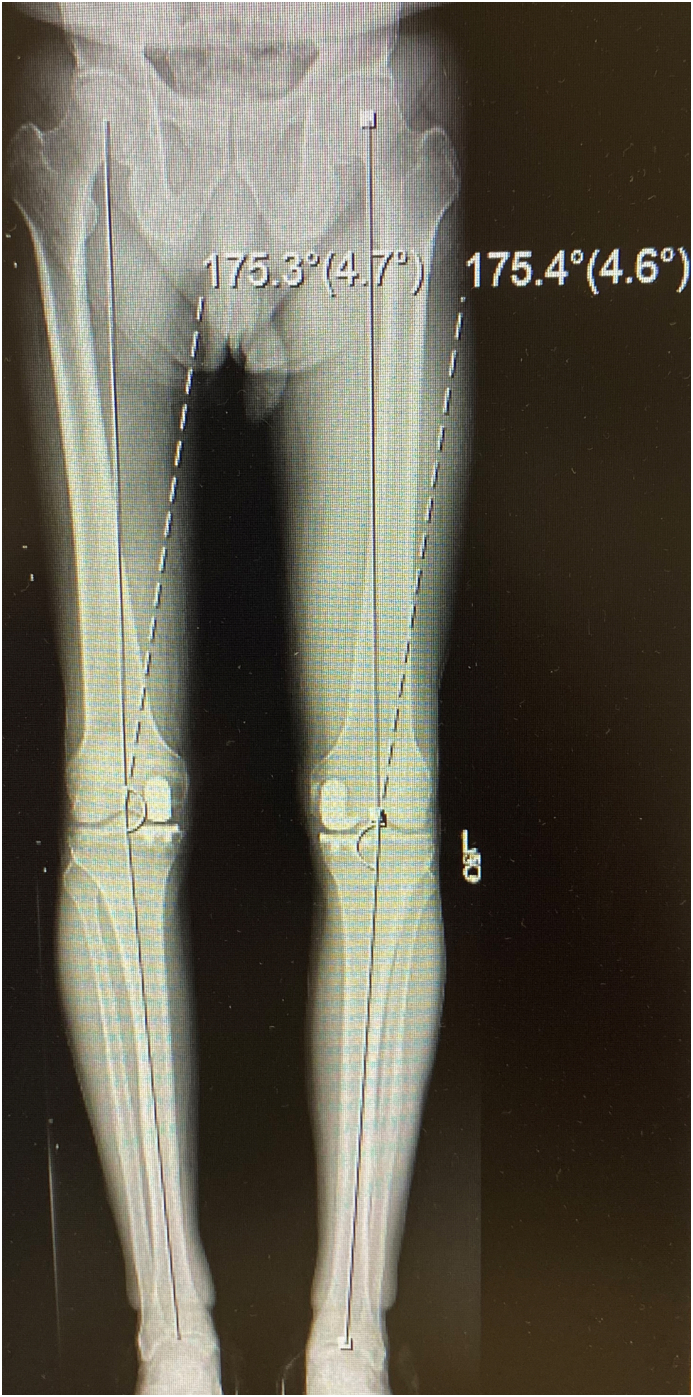
Fig. 6.
Postoperative full-length lower extremity x-ray showing appropriate limb alignment.
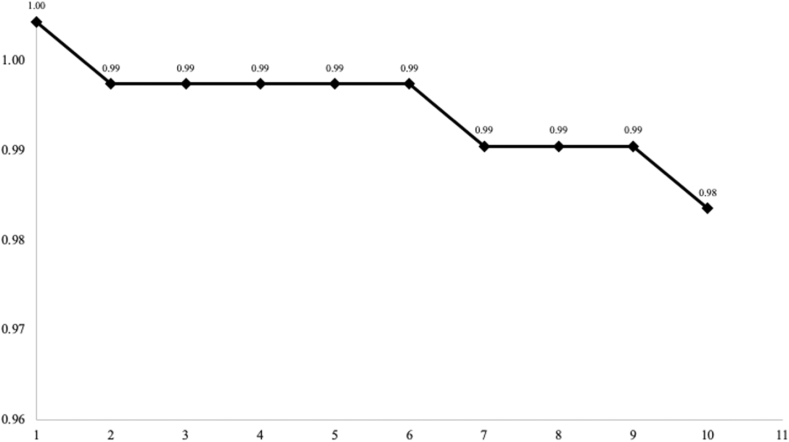
Fig. 7.
Implant survivorship over 10 years.
2.3. Data analyses
The outcomes assessed in this study were: 1) 10-year survivorships; 2) patient satisfaction scores; and 3) re-operations. Survivorships were analyzed using Kaplan-Meier survivorship curves. Patient satisfaction scores were evaluated by asking patients how satisfied they were with their surgery, with answers stratified as “very satisfied,” “satisfied,” neutral,” “dissatisfied,” or “very dissatisfied.” Re-operations were measured by asking patients if they had any re-operations on the ipsilateral knee and, if so, how soon after the original index procedure.
3. Results
3.1. 10-Year survivorships
During the study period, overall implant survivorship was 99%. There were two patients out of the 185 who required surgery involving the removal or replacement of any component. Aseptic survivorship was 99.5% (1 out of 185) and septic survivorship was 99.5% (1 out of 185 patients). There was one patient who was converted to a total knee arthroplasty due to degeneration in the contralateral compartment at 5 years following the index procedure. The other patient required a polyethylene exchange due to an acute infection within 5 weeks following the initial surgery. Neither patient has required another procedure at the latest follow-up.
3.2. Patient satisfaction scores
Overall, 97% of the patients were at least satisfied with their postoperative outcomes, with 81% of patients reporting being very satisfied. Patients who were “neutral,” “dissatisfied,” or “very dissatisfied” with their procedure represented 3% of the overall study cohort.
3.3. Re-operations
Only two patients required re-operations without component exchange. Both operations were arthroscopies performed within 2 years of the index procedure. One patient required surgical intervention for the removal of a cement loose body. Another patient required arthroscopic scar debridement that formed between the fat pad and the ACL. Both patients have continued to do well at the most recent follow-up.
4. Discussion
Unicompartmental knee arthroplasty has a long-standing successful history for patients who have single-compartment knee arthritis. Although this surgery can be highly beneficial for patients, there is still a moderate revision rate, most commonly related to component malpositioning, which can lead to accelerated wear. Robotic assistance has helped optimize implant placement; however, long-term (10-year) outcome data is limited in the current literature. This study identified 99% overall, 99.5% aseptic, and 99.5% septic implant survivorship. There is one patient who is requiring revision surgery due to the progression of arthritis, and the other patient needed a revision due to an acute infection. Furthermore, over 97% of patients reported being satisfied, if not very satisfied, with their surgical outcomes. Therefore, based on these data, we believe that robotic assistance can potentially help achieve optimal UKA outcomes and thus recommend utilizing this technology in the operating room when possible.
Other studies have also found advantages when using robotic assistance for unicompartmental knee arthroplasty.12,13,14 In a study by Pearle et al., the authors found overall survivorship at a mean of 30 months (range, 22 to 52) to be 98.8% (95% confidence interval (CI): 97.8–99.3%).12 In their worst-case scenario analysis (considering patients who declined to participate as failures), survivorship was only reduced by 2.8–96.0% (95% CI: 94.7–97.0%). The authors also noted that 92% of patients were either satisfied (21%) or very satisfied (71%). In a mid-term survivorship analysis, Heckmann et al., identified 5-year all-cause re-operation survivorship to be 92.9% (95% CI: 84.5–96.7%) and conversion to TKA survivorship to be 100% (95% CI: 95.0 to 100).13 A robotic-assisted versus non-robotic-assisted comparison found robotic-assistance to be associated with a significantly lower overall revision rate compared to non-robotically assisted UKAs at 3 years (hazard ratio (HR) 0.58; p < 0.001).14 Revision for aseptic loosening was also lower for the robotic-assisted cohort compared to the non-robotic-assisted cohort (HR 0.34; p = 0.001).
Some studies have found lower survivorship rates than this current study or have found limited advantages to robotic assistance.15,16 In another longer-term outcomes study by Carlson et al., they found 85% survivorship at a minimum of 10 years (mean, 11.4 and range, 10.0 to 13.8).15 However, the implants utilized in the aforementioned study were different than the ones analyzed in the current study, and the surgical technique varied as robotic assistance was not utilized. In a prospective, randomized, parallel, single-center study, Banger et al. compared 55 robotic-assisted vs. 49 manual UKAs at 5 postoperative years.16 While no statistical differences between the cohorts were noted regarding patient reported or clinical outcomes, the authors noted a lower re-operation rate in the robotic-arm-assisted cohort compared to that of the manual cohort (0 versus 9%; p < 0.001). It is notable that, historically, disease progression was a common reason for revision for UKAs. Only one case of that was observed in this series, which would lead to the hypothesis that the robotic-assisted UKAs reconstruct the joint more anatomically and thus do not overstress the other compartments. Kazarian et al.17 demonstrated improved accuracy of component position with the same robotic-assisted system as used in the current study compared to manual UKA.
There are some potential limitations to the current study. The sample of patients evaluated represents a single surgeon's experience at a single institution, so larger samples with patients from multiple surgeons and hospitals would make these results more generalizable. Additionally, there was no comparison cohort included in this analysis as it focused exclusively on robotic-arm-assisted UKA survivorship. Future studies should compare matched cohorts between robotic-arm-assisted and manual-technique UKAs at long-term follow-up. In addition, patients were called by a surgeon different from their operating surgeon, so data collection bias is another source of potential error. Nevertheless, this study represents one of the few longer-term analyses of robotic-arm-assisted unicompartmental knee arthroplasty survivorship and patient satisfaction scores.
5. Conclusion
Based on the data from the current study, robotic-assisted unicompartmental knee arthroplasty has potential long-term survivorship and patient-reported satisfaction advantages. Nearly all the patients evaluated maintained their original implants and were satisfied with their outcomes. A likely reason for the high survivorship is due to the more optimally placed components resulting in patient-specific limb alignment that more evenly distributes forces across the joint. Given the potential benefits, we recommend utilizing this technology when performing UKAs.
Funding/Sponsership
None.
Ethical approval
IRB exemption due to retrospective nature and public database.
Ethical approval
IRB exemption due to retrospective nature and public database.
No need for Guardian/Parent consent.
Data availability
Available in a respository upon request.
CRediT authorship contribution statement
Martin Roche: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Roles, Writing – original draft, and, Writing – review & editing. Rushabh Vakharia: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Roles, Writing – original draft, and, Writing – review & editing. Tsun Law: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Roles, Writing – original draft, and, Writing – review & editing. Nipun Sodhi: Writing – review & editing. Daniel Hameed: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Roles, Writing – original draft, and, Writing – review & editing. Michael A. Mont: Writing – review & editing.
Declaration of competing interest
MR- None RV- None TL- None DH- None NS- None MM- None.
Acknowledgements
None.
References
- 1.Carlson S.W., Lu Y., Sierra R.J. Minimum 10-year survivorship of mobile-bearing unicompartmental arthroplasty: single surgeon, North American non-Designer consecutive series. J Arthroplasty. 2022;37:S88–S93. doi: 10.1016/J.ARTH.2022.02.066. [DOI] [PubMed] [Google Scholar]
- 2.Lyons M.C., MacDonald S.J., Somerville L.E., Naudie D.D., McCalden R.W. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012;470:84–90. doi: 10.1007/S11999-011-2144-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parratte S., Pauly V., Aubaniac J.M., Argenson J.N.A. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2012;470:61–68. doi: 10.1007/S11999-011-1961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lustig S., Lording T., Frank F., Debette C., Servien E., Neyret P. Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee. 2014;21(Suppl 1):S26–S32. doi: 10.1016/S0968-0160(14)50006-3. [DOI] [PubMed] [Google Scholar]
- 5.Carlson S.W., Sierra R.J. Unicompartmental knee arthroplasty over total knee arthroplasty: a more cost-effective strategy for treating medial compartment arthritis. Ann Transl Med. 2020;8:510. doi: 10.21037/atm.2020.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson W.B., Engh C.A., Parks N.L., Hamilton W.G., Ho P.H., Fricka K.B. A lower threshold for revision of aseptic unicompartmental vs total knee arthroplasty. Bone Joint J. 2020;102-B:91–95. doi: 10.1302/0301-620X.102B6.BJJ-2019-1538.R1. [DOI] [PubMed] [Google Scholar]
- 7.Lombardi A.v., Kolich M.T., Berend K.R., Morris M.J., Crawford D.A., Adams J.B. Revision of unicompartmental knee arthroplasty to total knee arthroplasty: is it as good as a primary result? J Arthroplasty. 2018;33:S105–S108. doi: 10.1016/J.ARTH.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Vasso M., Corona K., D'Apolito R., Mazzitelli G., Panni A.S. Unicompartmental knee arthroplasty: Modes of failure and conversion to total knee arthroplasty. Joints. 2017;5:44. doi: 10.1055/S-0037-1601414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J., Ng N., Scott C.E.H., et al. Cite this article. Bone Joint J. 2022;104:541–548. doi: 10.1302/0301-620X.104B5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iturriaga C., Salem H.S., Ehiorobo J.O., Sodhi N., Mont M.A. Robotic-assisted versus manual unicompartmental knee arthroplasty: a Systematic review. Surg Technol Int. 2020;37:275–279. [PubMed] [Google Scholar]
- 11.Cool C.L., Needham K.A., Khlopas A., Mont M.A. Revision analysis of robotic arm-assisted and manual unicompartmental knee arthroplasty. J Arthroplasty. 2019;34:926–931. doi: 10.1016/J.ARTH.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 12.Pearle A.D., van der List J.P., Lee L., Coon T.M., Borus T.A., Roche M.W. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee. 2017;24:419–428. doi: 10.1016/J.KNEE.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heckmann N.D., Antonios J.K., Chen X.T., et al. Midterm survivorship of robotic-assisted lateral unicompartmental knee arthroplasty. J Arthroplasty. 2022;37:831–836. doi: 10.1016/J.ARTH.2022.01.023. [DOI] [PubMed] [Google Scholar]
- 14.St Mart J.P., de Steiger R.N., Cuthbert A., Donnelly W. The three-year survivorship of robotically assisted versus non-robotically assisted unicompartmental knee arthroplasty. Bone Joint J. 2020;102-B:319–328. doi: 10.1302/0301-620X.102B3.BJJ-2019-0713.R1. [DOI] [PubMed] [Google Scholar]
- 15.Carlson S.W., Lu Y., Sierra R.J. Minimum 10-year survivorship of mobile-bearing unicompartmental arthroplasty: single surgeon, North American non-Designer consecutive series. J Arthroplasty. 2022;37:S88–S93. doi: 10.1016/J.ARTH.2022.02.066. [DOI] [PubMed] [Google Scholar]
- 16.Banger M., Doonan J., Rowe P., Jones B., MacLean A., Blyth M.J.B. Robotic arm-assisted versus conventional medial unicompartmental knee arthroplasty: five-year clinical outcomes of a randomized controlled trial. Bone Joint J. 2021;103-B:1088–1095. doi: 10.1302/0301-620X.103B6.BJJ-2020-1355.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radiological outcomes following manual and robotic-assisted unicompartmental knee arthroplasty. Kazarian GS, Barrack RL, Barrack TN, Lawrie CM, Nunley RM. Bone Jt Open. 2021;2(3):191–197. doi: 10.1302/2633-1462.23.BJO-2020-0205.R1. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available in a respository upon request.