Abstract
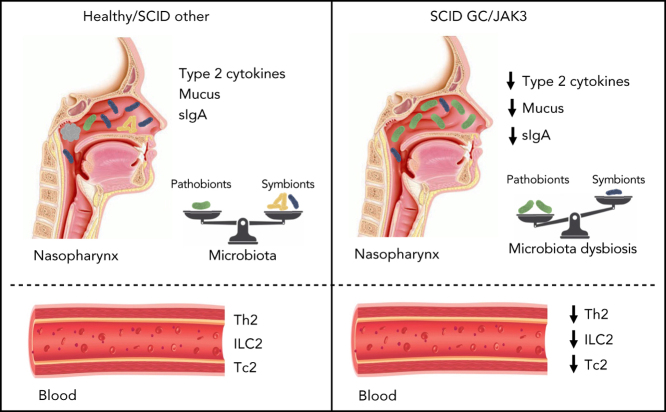
Both innate and adaptive lymphocytes have critical roles in mucosal defense that contain commensal microbial communities and protect against pathogen invasion. Here we characterize mucosal immunity in patients with severe combined immunodeficiency (SCID) receiving hematopoietic stem cell transplantation (HSCT) with or without myeloablation. We confirmed that pretransplant conditioning had an impact on innate (natural killer and innate lymphoid cells) and adaptive (B and T cells) lymphocyte reconstitution in these patients with SCID and now show that this further extends to generation of T helper 2 and type 2 cytotoxic T cells. Using an integrated approach to assess nasopharyngeal immunity, we identified a local mucosal defect in type 2 cytokines, mucus production, and a selective local immunoglobulin A (IgA) deficiency in HSCT-treated SCID patients with genetic defects in IL2RG/GC or JAK3. These patients have a reduction in IgA-coated nasopharyngeal bacteria and exhibit microbial dysbiosis with increased pathobiont carriage. Interestingly, intravenous immunoglobulin replacement therapy can partially normalize nasopharyngeal immunoglobulin profiles and restore microbial communities in GC/JAK3 patients. Together, our results suggest a potential nonredundant role for type 2 immunity and/or of local IgA antibody production in the maintenance of nasopharyngeal microbial homeostasis and mucosal barrier function.
Key Points
-
•
Pretransplant conditioning affects innate (NK and ILCs) and adaptive (T helper 2 and type 2 cytotoxic T cells) reconstitution.
-
•
GC/JAK3-deficient SCID receiving nonconditioned HSC grafts fail to develop type 2 responses and have mucosal IgA deficiency with dysbiosis.
Introduction
Hematopoietic stem cell transplantation (HSCT) for severe combined immunodeficiency (SCID) represents a life-saving therapy for this heterogeneous group of hematopoietic disorders.1, 2 HSCT generates a variable degree of hematolymphoid reconstitution that depends on the pretransplant conditioning regimen (eg, myeloablation) as well as the genetic defect being treated.2, 3 For example, T–B– natural killer cell (NK)+ SCID resulting from defects in the antigen receptor recombination pathway harbor immature lymphoid precursors in the thymus and bone marrow. These patients may receive either myeloablation that can enhance myeloid and lymphoid reconstitution after HSCT or reduced-intensity conditioning that may eliminate competitive but abnormal thymocyte precursor cells or NK cells. In contrast, patients with T–B+NK– SCID (caused by mutations in the common γ chain [γc] gene IL2RG or the Janus kinase JAK3) lack lymphoid precursors and are generally not cytoreduced before HSCT.3 As a result, lymphoid lineages engraft rapidly, but myeloid reconstitution is less robust.
Innate lymphoid cells (ILCs) are tissue-resident lymphocytes, enriched at mucosal barriers with roles in immune defense and tissue remodeling.4, 5 Diverse ILC subsets (ILC1/2/3) produce a restricted range of cytokines that target hematopoietic as well as non-hematopoietic (eg, stromal, epithelial, and endothelial) cells.6 Previous studies have documented the developmental and functional parallels between ILCs and T helper cells.7 This homology suggests a potential functional redundancy during immune responses but may also provide a means to synergistically promote immune defense.
Recently, it was shown that pretransplant conditioning allows for better post-HSCT immune reconstitution with higher frequencies of donor NK and ILC subsets in myeloablated T–B–NK+ SCID and cancer patients compared with nonconditioned T–B+NK– SCID recipients.3 The differential ILC engraftment in these patients results from a combination of both absence of conditioning and inherent genetic defects, providing a unique setting (ILC/NK+ vs ILC/NK– phenotypes) to assess biological roles for ILC/NK cells in human immunity. Interestingly, both HSCT groups showed robust donor T-cell engraftment with restoration of cellular immunity and recovery of immune competence. In a long-term follow-up of these 2 HSCT-treated patient groups, no obvious differences in clinical course or disease susceptibility were noted. Because both HSCT groups showed similar clinical recoveries (“cure”), it was concluded that NK cells and diverse ILC subsets may be redundant for most aspects of normal human immunity3, 8 that more recently have been extended to development and function of lymphoid tissues.9
Diverse ILC subsets are enriched at mucosal surfaces and, in conjunction with adaptive T- and B-cell responses, promote barrier defense and tissue regeneration after infection and inflammation and regulate microbial communities that have a symbiotic relationship with the host.10, 11 The reciprocal interactions and coordinated regulation of ILCs vs T helper cells for immune defense remains unclear. A better characterization of mucosal immunity in ILC/NK+ vs ILC/NK– HSCT patients may shed light on the specific and/or redundant roles of innate lymphocytes at barrier surfaces for protection from disease.
Here we further analyzed a large cohort of HSCT-treated patients with SCID to assess impact of hematopoietic reconstitution on mucosal barrier function. We document a selective deficiency in type 2 immunity, strong decreases in nasopharyngeal immunoglobulin A (IgA), and nasal microbial dysbiosis in IL2RG/JAK3-deficient patients receiving nonconditioned HSCT.
Methods
Patient and control cohorts
Healthy donors were recruited originally as part of the Milieu Intérieur cohort (https://www.milieuinterieur.fr/en/; supplemental Materials and methods, available on the Blood Web site). HSCT-treated SCID patients were followed up at Hôpital Necker-Enfants Malades (French National Reference Center for Primary Immunodeficiencies). Pathogenic mutations were identified in all cases (supplemental Table 1). Written informed consent was obtained from all patients and/or parents. Nasopharyngeal swabs were obtained concurrently with blood samples during routine visits (no evidence of ongoing infection, autoimmunity, or allergy; no antibiotic use) and were processed as described elsewhere.12, 13
Cell isolation and fluorescence-activated cell sorting analysis
Human peripheral blood mononuclear cells were isolated by using density gradient centrifugation. For fluorescence-activated cell sorting analysis, cells were first stained with Flexible Viability Dye eFluor 506 (eBioscience) following by surface antibody staining on ice. Fc receptors were blocked by using IgG from human serum (MilliporeSigma). Samples were acquired with an LSRFortessa (BD) and analyzed by using FlowJo version 10.7.1 (Tree Star). Bacterial species-specific antibody against microbiota were assessed as described previously.14
Analysis of nasopharyngeal proteins
Total IgA, IgM, IgG1, IgG2, IgG3, and IgG4 were determined by using the Bio-Plex Pro Human Isotyping Assay Panel (Bio-Rad). Data were acquired on a Bio-Plex 200 System (Bio-Rad) and analyzed with Bio-Plex Manager version 5 (Bio-Rad). IgA1 and IgA2 subclasses were measured by Simoa (Quanterix). Total IgD were determined by using an enzyme-linked immunosorbent assay (ELISA) kit (MBS564048; MyBioSource). Total IgE was determined by using an ELISA kit (88-50610; Invitrogen). Data were collected with the Multiskan Spectrum (Thermo Fisher Scientific).
Cytokines were quantified by Simoa Cytokine 3-Plex B, Discovery, or Advantage Kits (Quanterix) except interferon-γ and interleukin-17F (IL-17F), which used Quanterix Homebrew assays. Nasopharyngeal mucin levels were analyzed by using an MUC5AC ELISA Kit (NBP2-76703; Novus Biologicals; diluted 1/50). Eosinophil cationic protein was determined for swabs medium using an ELISA kit (MBS2602477; MyBioSource; diluted 1/2). Total protein content of the supernatants was calculated by using the Bradford method.15
16S ribosomal RNA sequencing and analysis
16S ribosomal RNA (rRNA) sequencing and sequence processing and statistical analysis have been described previously.12, 13 A total of 2 974 329 reads (90 131 reads on average per sample) were obtained.
Bacterial quantification by quantitative reverse transcription polymerase chain reaction assays
Bacterial quantitative polymerase chain reaction used universal 16S rRNA primers to measure total bacteria (16S_F: 5′-ATTACCGCGGCTGCTGG-3′ and 16S and 16S_R: 5′-ATTACCGCGGCTGCTGG-3′) and Streptococcus pneumoniae (LytA gene, F: 5′- ACGCAATCTAGCAGATGAAGC-3′ and R: 5′-TGTTTGGTTGGTTATTCGTGC-3′).
Statistical analysis
Statistics were performed by using GraphPad Prism (GraphPad Software). P values were determined by a Kruskal-Wallis test, followed by Dunn's posttest for multiple group comparisons with median reported. Correlations between the different assays were calculated by using the Spearman test. Heatmaps were generated with Qlucore OMICS Explorer version 3.5. Correlation matrices were built using the Spearman correlation and computed by using R version 4.0.3 (R Foundation for Statistical Computing).
Results
This study analyzed a cohort of 21 patients with SCID who have been successfully treated with HSCT at Necker Hospital since 1977. Patients with SCID and X-linked as well as autosomal etiologies were included; some patients required immunoglobulin replacement therapy (IgRT) by subcutaneous injection of IgG for specific clinical conditions (including recurrent respiratory tract infections16, 17, 18) (supplemental Table 1). Several patients have been previously reported.3, 9 The group “GC/JAK3” were T–B+NK– SCID (IL2RG and JAK3) patients who received non-myeloablative HSCT, and the group “SCID-other” were T–B–NK+ or T–B+NK+ SCID (RAG1/2, ARTEMIS, major histocompatibility complex class II, IL7RA) patients, the majority of whom received pretransplant cytoreduction. All HSCT-treated SCID patients exhibited successful donor hematopoietic reconstitution and recovered T-cell immunity. Once clinically stable, patients were discharged and followed up periodically in our outpatient clinic. The follow-up period varied from 18 to 42 years.
HSCT-treated GC/JAK3 patients have reduced circulating type 2 lymphocytes
Although HSCT-treated SCID patients have stable T-cell reconstitution with balanced CD4/CD8 ratios, naive T cells, and T-cell receptor excision circles,1, 3, 19 an in-depth analysis of their differentiated T-cell subsets has not been previously performed. ILC and NK cell reconstitution in SCID patients with SCID receiving myeloablative conditioning for HSCT has only been reported in two RAG-deficient patients.3 As reciprocal interactions between ILCs and T cells have been documented,20, 21, 22, 23 previously reported lack of NK and ILCs in the nonconditioned SCID recipients might be associated with perturbations in their T-cell compartment. We paid particular attention to differentiated T-cell subsets that can be identified by expression of specific chemokine receptors (see “Methods”; supplemental Figure 1 describes fluorescence-activated cell sorting gating).24, 25 Nonconditioned GC/JAK3 patients receiving IgRT post-HSCT (supplemental Table 1) were analyzed separately.
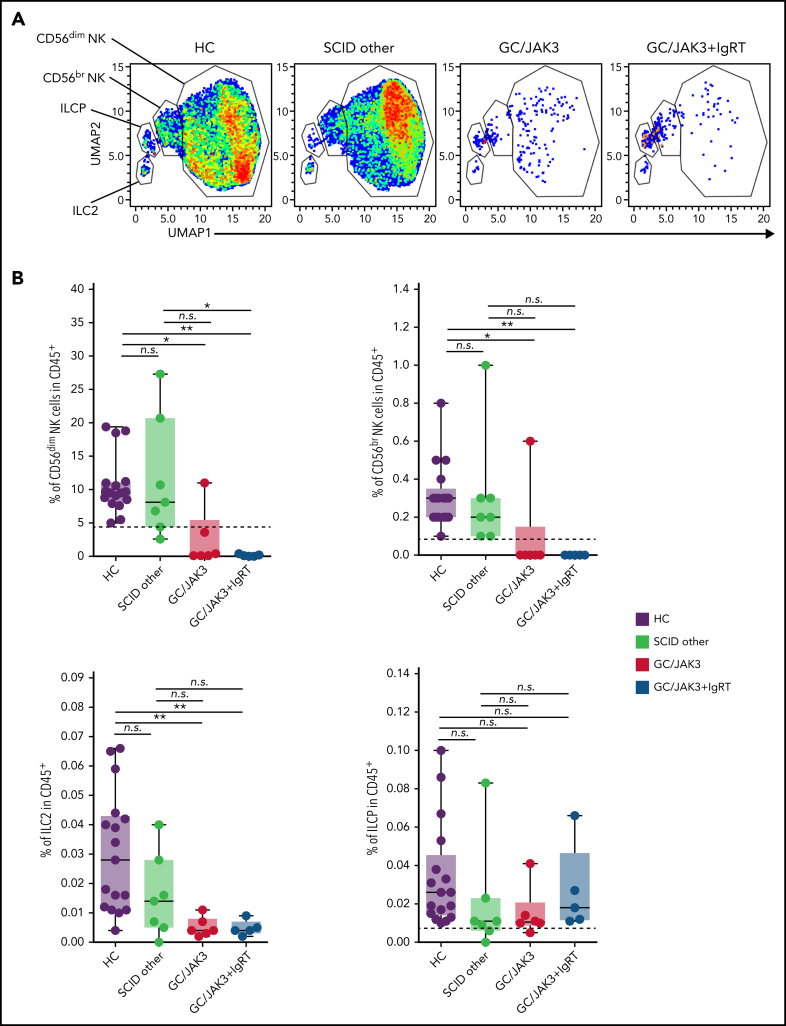
Circulating ILCs include CD56+ NK cells (CD56+++CD16– and CD56+CD16+ cells) and CD127+ ILC2 (CRTH2+) and ILCP (ILC precursors, CRTH2–CD117+ CD45RA+NKp44–).26 Using unsupervised clustering analysis, we observed a significant reduction in frequencies of NK cells and ILC2 but not ILCP in GC/JAK3 and GC/JAK3+IgRT patients compared with healthy control subjects (HC) and SCID-other patients (Figure 1A-B), confirming previous reports in HSCT-treated IL2RG/JAK3-deficient and RAG-deficient patients3 and further extending this observation to other SCID etiologies.
Figure 1.
Fluorescence-activated cell sorting analysis of peripheral blood mononuclear cells reveal a defect in differentiation of type 2 lymphocytes in HSCT-treated GC/JAK3 patients. (A) Unsupervised Uniform Manifold Approximation and Projection (UMAP)27 of single live CD45+Lin–CD3–CD4–CD7+ cells was applied for CD56, CD16, CD94, NKp46, CD94, CD127, CD161, CD25, CD117, and CRTH2 fluorescence parameters. (B) Supervised analysis of circulating ILCs including two CD56+ subsets of NK cells and two CD127+ subsets denoted as ILC2 (CRTh2+) and ILCP (ILC precursors, CRTh2–CD117+CD45RA+NKp44–) (manually gating strategy presented in supplemental Figure 1A). (C) UMAP analysis on CD4+ T cells, including CXCR3, CCR4, CRTH2, CCR6, CXCR5, CD25, CD127, and CD45RA fluorescence parameters (supplemental Figure 2A). (D) Supervised analysis of circulating T-cell populations. The different subsets were identified as follow: naive (CD45RA+), Th1 (Treg–CD45RA–CXCR5–CCR6–CXCR3+CCR4–), Th17 (Treg–CD45RA–CXCR5–CCR6+), Th2 (Treg–CD45RA–CXCR5–CCR6–CXCR3–CCR4+CRTH2+/−), and Treg (CD127loCD25+) (manually gating strategy is provided in supplemental Figure 1B). (E) UMAP analysis on CD8+ type 2 cytotoxic T-cell (Tc2) subset including CCR4 and CRTH2 fluorescence parameters (supplemental Figure 3). (F) Supervised analysis of circulating CD8+ Tc2 subset defined as CD45RA–CD25–CD94–CD56–CXCR5–CCR6–CXCR3–CCR4+CRTH2+/−. Panels B, D, and F: box plots with median ± minimum to maximum. P values were determined with the Kruskal-Wallis test followed by Dunn's posttest for multiple group comparisons; *P < .05, **P < .005, ***P < .001. n.s., not significant.
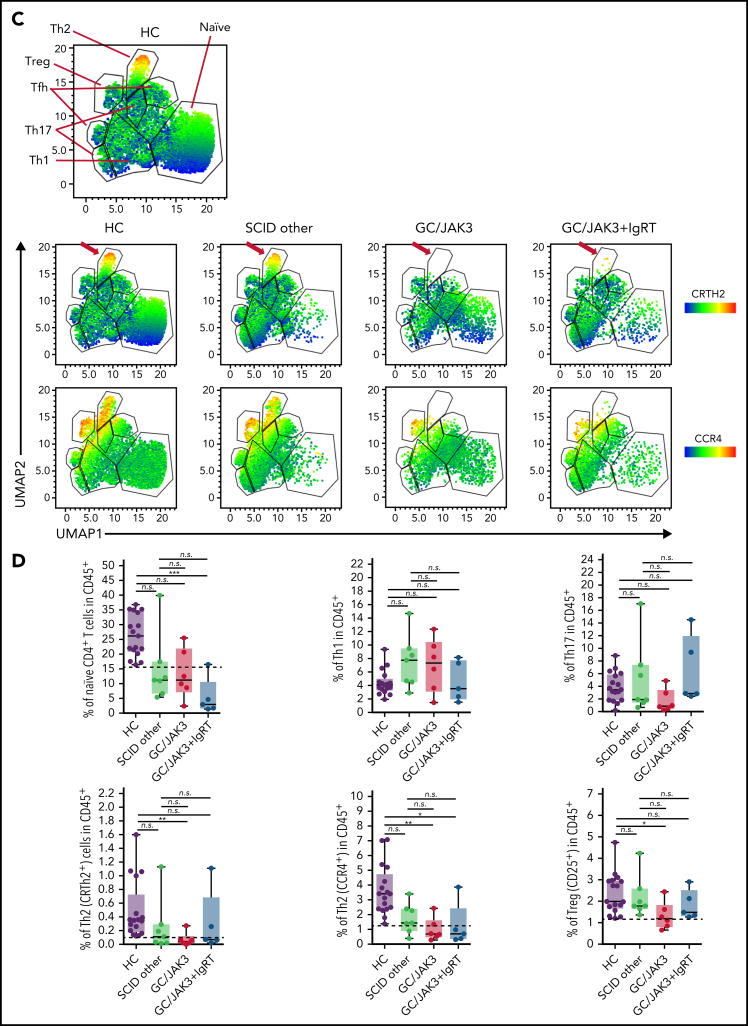
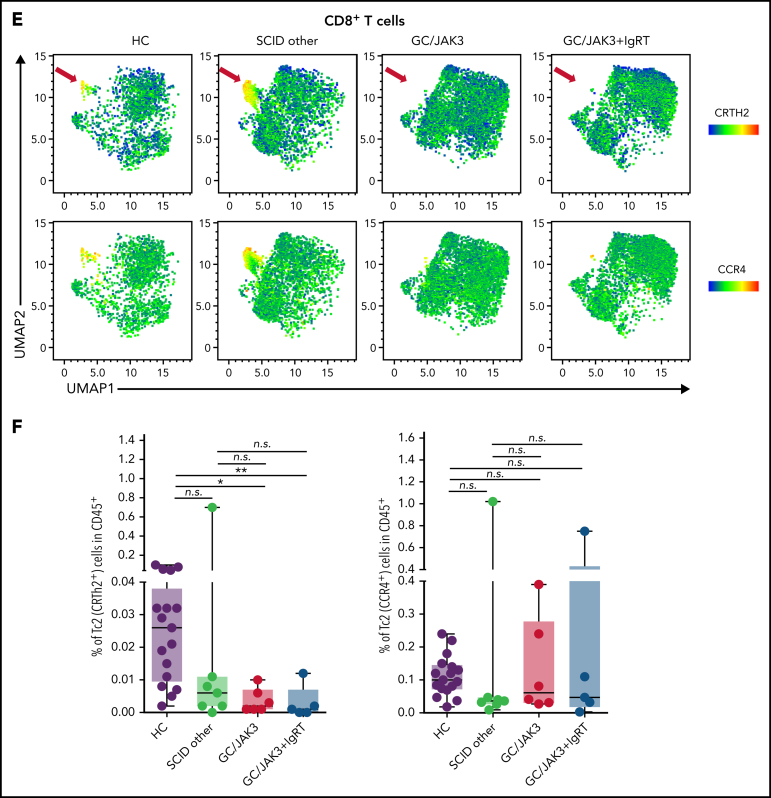
We next characterized naive and differentiated CD4+ T-cell subsets in this SCID cohort. Unsupervised clustering analysis allowed us to identify T-cell subsets, including naive (CD45RA+), T regulatory (Treg) (CD127loCD25+), follicular T helper (Treg–CD45RA–CXCR5+), T helper 1 (Th1) (Treg–CD45RA–CXCR5–CCR6–CXCR3+CCR4–), Th2 (Treg–CD45RA–CXCR5–CCR6–CXCR3–CCR4+CRTH2+/−), and Th17 (Treg–CD45RA–CXCR5–CCR6+). A significant reduction was observed in clusters of CCR4+CRTH2+/− cells corresponding to the Th2 subset, as well as a reduction in naive T cells (CD45RA+) in GC/JAK3 and GC/JAK3+IgRT patients compared with HC and SCID-other patients (Figure 1C-D). Other T helper subsets (ie, Th1, Th17, follicular T helper) were normally present in all HSCT SCID patients (Figure 1D; supplemental Figure 2).
A similar analysis was performed on CD8+ T cells. The unsupervised clustering analysis showed a significant decrease in the CCR4+CRTH2+ cluster corresponding to the type 2 cytotoxic T cell subset in CD8+ T cells in GC/JAK3 and GC/JAK3+IgRT patients (Figure 1E-F), whereas other CD8+ T-cell subsets were similar in SCID-other patients compared with HC (supplemental Figure 3).
The observations of a relative decrease in naive CD4+ T cells with a compensatory increase in activated CD8+ T cells after HSCT for SCID confirm earlier work,28 while our detailed assessment of differentiated T-cell subsets allowed us to identify a selective deficiency in blood CD4+ Th2 cells and CD8+ type 2 cytotoxic T cells in HSCT-treated GC/JAK3 patients. In all SCID etiologies, differentiation of other T helper subsets (ie, Th1, Th17, Treg) appeared largely intact. These results suggest that nonconditioned HSCT-treated GC/JAK3 patients manifest a generalized and selective deficiency in innate and adaptive lymphocytes involved in type 2 immunity.
HSCT-treated GC/JAK3 patients have reduced nasopharyngeal type 2 cytokines
We next assessed mucosal immune responses in HSCT-treated SCID patients. Nasopharyngeal swabs were obtained concurrently with blood samples and were processed as described elsewhere12, 13 to yield nucleic acids as well as a soluble fraction that harbored cytokines, antibodies, antimicrobial peptides, and various metabolites. Because differentiated T helper cells and ILCs maintain mucosal homeostasis,4, 5 we used digital ELISA (Simoa) to quantitate cytokines associated with Th1/ILC1, Th2/ILC2, and Th17/ILC3 responses in these nasopharyngeal samples.
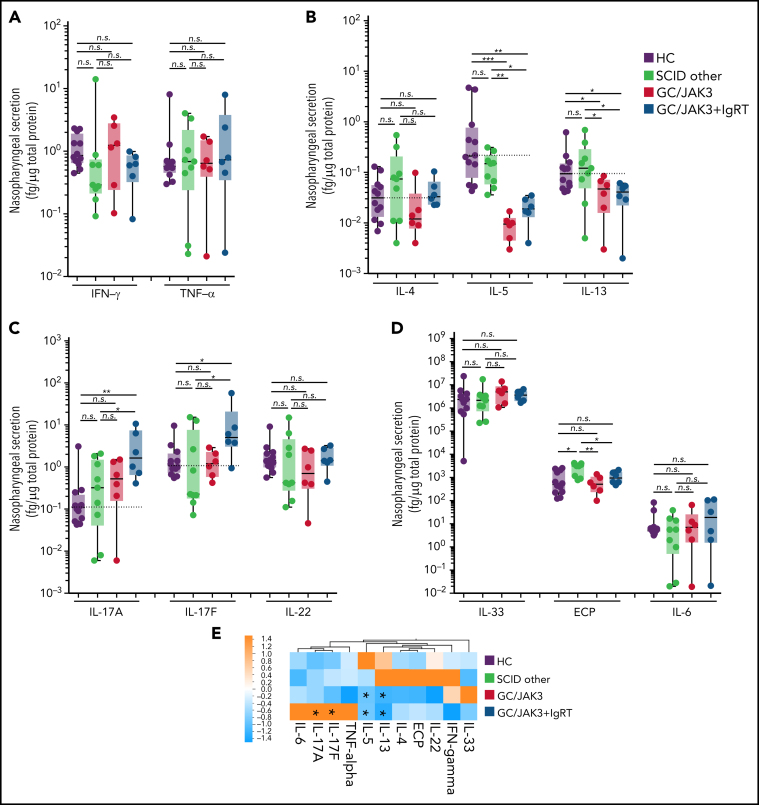
We found no significant differences in the levels of type 1 cytokines (interferon-γ, tumor necrosis factor-α) in normal controls compared with HSCT-treated GC/JAK3 or SCID-other patients (Figure 2A). In contrast, levels of type 2 cytokines IL-5 and IL-13 were clearly decreased in nonconditioned GC/JAK3 patients, whereas IL-4 levels were within healthy ranges (Figure 2B). Although the deficiency in nasopharyngeal IL-13 persisted in GC/JAK3 patients receiving intravenous immunoglobulin (IVIG), IL-4 and IL-5 levels were somewhat higher in these patients compared with nonconditioned GC/JAK3 patients who did not receive IgRT. Concerning inflammatory type 3 cytokines (IL-17A, IL-17F, and IL-22), nasopharyngeal mucosal levels were not different from controls except in GC/JAK3 patients being treated with IgRT (Figure 2C). It is unclear whether these increases in nasopharyngeal cytokines result from IgRT treatment or are related to other mechanisms that underlie the need to treat (eg, infections) with IgRT.
Figure 2.
HSCT-treated GC/JAK3 patients have a generalized defect in nasopharyngeal type 2 immunity. (A) Nasopharyngeal levels of type 1 cytokines (interferon [IFN]-γ and tumor necrosis factor [TNF]-α). (B) Nasopharyngeal levels of type 2 cytokines (IL-4, IL-5, and IL-13). (C) Nasopharyngeal levels of type 3 cytokines (IL-17A, IL-17F, and IL-22). (D) Nasopharyngeal levels of IL-33, IL-6, and eosinophil cationic protein (ECP)/RNase 3. (E) Heatmap representation of the mean of the concentration of all nasopharyngeal cytokines in healthy and HSCT-treated SCID patients. Panels A-D: box plots with median ± minimum to maximum. P values were determined with the Kruskal-Wallis test followed by Dunn's posttest for multiple group comparisons; *P < .05, **P < .005, ***P < .001. n.s., not significant.
Type 2 cytokine secretion is regulated by stromal-derived factors and promotes activation of hematopoietic (ie, eosinophils and mast cells) as well as nonhematopoietic (goblet cells) targets.29, 30 We found that IL-33 (a major inducer of recruitment, activation, and IL-5 and IL-13 production by type 2 lymphocytes31, 32, 33) was not reduced in nasopharyngeal samples (Figure 2D), whereas eosinophil cationic protein (a marker for tissue eosinophilia34, 35) was reduced in GC/JAK3 patients consistent with reduced IL-5 levels (Figure 2B,D). Nasopharyngeal IL-6 levels were not significantly elevated in any SCID patient, although they tended to be higher in GC/JAK3+IgRT patients (Figure 2D). When all data were clustered, the heatmap clearly distinguished the defective type 2 cytokine production (in particular, IL-5 and IL-13) in the context of nonconditioned HSCT for GC/JAK3 and irrespective of IgRT (Figure 2E).
Systemic and mucosal immunoglobulin subtypes in HSCT-treated SCID patients
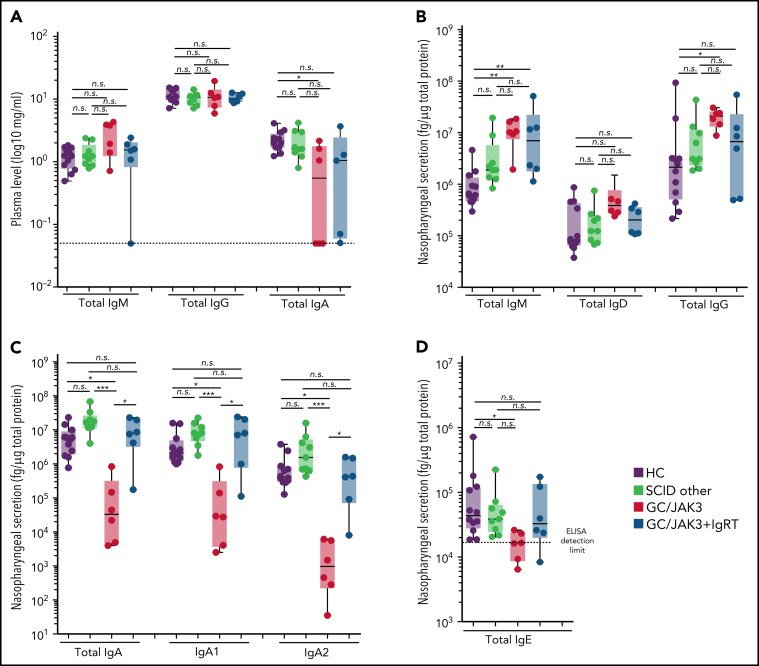
Previous studies have analyzed the impact of pre-HCST conditioning on systemic antibody levels after hematopoietic reconstitution for SCID.18, 36 In particular, busulfan administration is correlated with higher donor chimerism, especially in the B-cell compartment.36 We found that nonconditioned GC/JAK3 patients exhibited somewhat elevated total serum IgM, but all 6 patients studied had normal total serum IgG levels (Figure 3A), confirming that GC/JAK3–deficient B cells can produce switched IgGs in the presence of normal T cells.18 In contrast, serum IgA was undetectable (selective IgA deficiency) in one-half of HSCT-treated GC/JAK3 patients, mirroring previous reports.37, 38 SCID-other patients harbored normal immunoglobulin subtype distributions and levels. Interestingly, need for IgRT in GC/JAK3 patients did not clearly correlate with any selective serum immunoglobulin deficiency but was dictated by the clinical context (history of recurrent respiratory tract infections).
Figure 3.
HSCT-treated GC/JAK3 patients without immunoglobulin replacement therapy have a decrease in nasopharyngeal secretory IgA. (A) Serum immunoglobulin concentrations in healthy and HSCT-treated SCID patients. (B) Nasopharyngeal concentrations of total IgM, IgD, and IgG in healthy and HSCT-treated SCID patients. (C) Nasopharyngeal concentrations of total IgA and IgA1 and IgA2 in healthy and HSCT-treated SCID patients. (D) Nasopharyngeal concentrations of total IgE in healthy and HSCT-treated SCID patients. Panels A through D: box plots with median ± minimum to maximum. P values were determined with the Kruskal-Wallis test followed by Dunn's posttest for multiple group comparisons; *P < .05, **P < .005, ***P < .001. n.s., not significant.
We next assessed mucosal immunoglobulins in HSCT-treated SCID patients by measuring immunoglobulin isotypes and subclasses in paired nasopharyngeal samples. We found that total nasopharyngeal IgM and IgG were elevated in GC/JAK3 patients compared with controls but less so compared with SCID-other patients (Figure 3B), which seemed related to higher levels of IgG3 (supplemental Figure 4A). In contrast, all GC/JAK3 patients exhibited a strong reduction in total nasopharyngeal IgA that concomitantly involved both IgA1 and IgA2 (Figure 3C; supplemental Figure 4B) and a significant reduction in total nasopharyngeal IgE (Figure 3D). Interestingly, total nasopharyngeal IgD levels were significantly increased in GC/JAK3 patients. Lastly, GC/JAK3+IgRT patients “normalized” nasopharyngeal immunoglobulin distributions with increased IgA and IgE (Figure 3C-D), although the mechanistic basis remains unclear. Together, our results illustrate the distinct profiles of systemic and local mucosal IgA responses in HSCT-treated SCID patients.
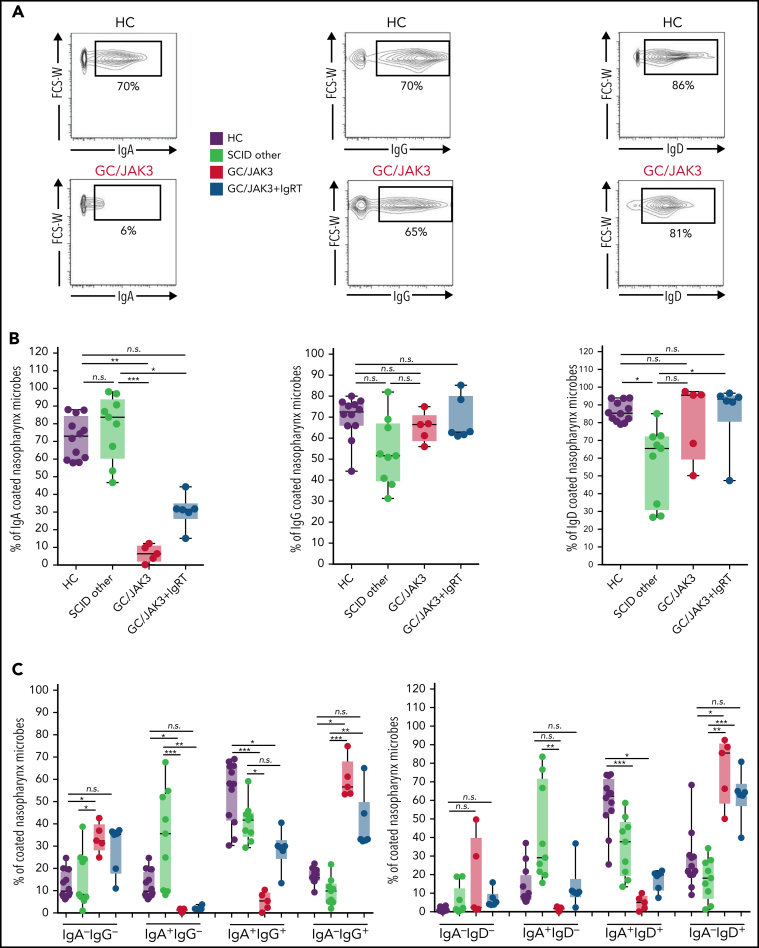
IgG and IgD may provide mucosal protection in the context of IgA deficiency
We next analyzed the binding of different immunoglobulin isotypes to nasopharyngeal microbiota using a flow cytometer–based assay.12 We found a significant decrease in the percentage of IgA-coated nasopharyngeal microbes as well as the density of IgA coating (IgA mean fluorescence intensity, not shown) in GC/JAK3 patients compared with SCID-other patients and HC (Figure 4A-B). Interestingly, GC/JAK3+IgRT patients exhibited a partial but significant increase in IgA-coated nasopharyngeal microbes (Figure 4B) consistent with the increase in nasopharyngeal IgA (Figure 3C). Whether the increase in IgA activity after IgRT results from an indirect effect following stimulation of type 2 cytokine production39, 40, 41 remains unclear.
Figure 4.
HSCT-treated GC/JAK3 patients without IVIG replacement therapy have decreased IgA-coating of nasopharyngeal bacteria. (A) Representative dot plots of IgA, IgG, and IgD binding to nasopharyngeal microbiota in healthy and HSCT-treated SCID patients. (B) Percentage of IgA/IgG/IgD–coated nasopharynx microbes in healthy and HSCT-treated SCID patients. (C) Double IgA/IgG or IgA/IgD–coated nasopharynx microbes in healthy and HSCT-treated SCID patients. Panels A through C: box plots with median ± minimum to maximum. P values were determined with the Kruskal-Wallis test followed by Dunn's posttest for multiple group comparisons; *P < .05, **P < .005, ***P < .001. FCS-W, forward scatter, width; n.s., not significant.
Compensatory IgG responses to gut commensal bacterial communities may operate in the absence of IgA-specific responses.42 Because other immunoglobulin isotypes and subclasses were normally present (IgD) or elevated (IgM and IgG) in GC/JAK3 patients (Figure 3B), we quantitated the fraction (%) and intensity (mean fluorescence intensity) of nasopharyngeal microbes that were coated with IgG, IgA, or IgD by using a recently reported multiplexing technique.12 The majority of nasopharyngeal microbes in healthy individuals are coated with IgA in combination with IgD and to a lesser extent with IgG (Figure 4C). SCID-other patients showed a similar pattern of nasopharyngeal microbe coating, whereas nasopharyngeal microbes in GC/JAK3 patients were more abundantly coated with IgG and IgD alone. Finally, we observed an increase in IgA-/IgG-double coated nasopharyngeal microbes in GC/JAK3 patients receiving IgRT, consistent with the increased nasopharyngeal IgA in these individuals. These results are consistent with the notion that IgG42 and IgD43, 44, 45 may provide a layer of mucosal protection during IgA deficiency.
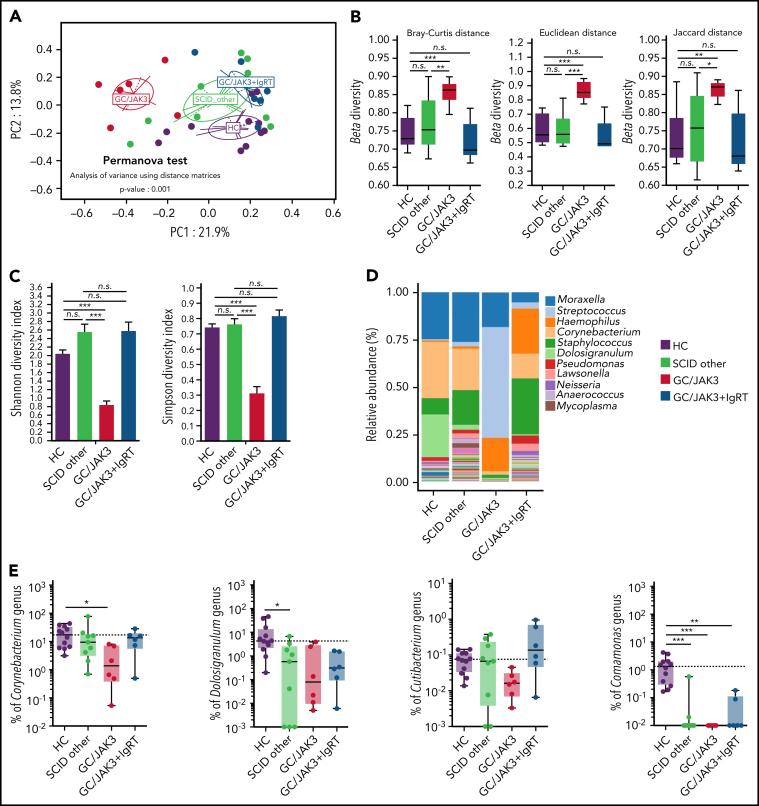
HSCT-treated GC/JAK3 patients have nasopharyngeal microbiota dysbiosis
Secretory IgA produced locally at mucosal sites plays an essential role in host defense12 and shapes commensal microbiota composition and activity in each individual.46 To characterize local nasopharyngeal microbial communities, we performed 16S rRNA gene sequencing from nasopharyngeal samples, calculated bacterial β diversity, and subjected sequenced operational taxonomic units to principal coordinate analysis. We found that nasopharyngeal samples derived from HSCT-treated GC/JAK3 patients without IVIG replacement therapy clustered distinctively from the HC and SCID-other patient samples (Figure 5A) and had elevated β diversity based on Bray-Curtis, Euclidean, and Jaccard distance matrices (Figure 5B). Accordingly, Shannon and Simpson diversity indices were reduced in these GC/JAK3 patients (Figure 5C). We further applied a nonmetric multidimensional scaling using Bray-Curtis distances and found a similar distinctive clustering of GC/JAK3 patients not treated with IVIG (supplemental Figure 5A). In contrast, SCID-other patients with more complete hematopoietic reconstitution exhibited nasopharyngeal microbial communities that were more similar to HC (Figure 5A-C; supplemental Figure 5B). Total bacterial load was also increased in GC/JAK3 patients not treated with IgRT compared with HC and other SCID patients (supplemental Figure 5C).
Figure 5.
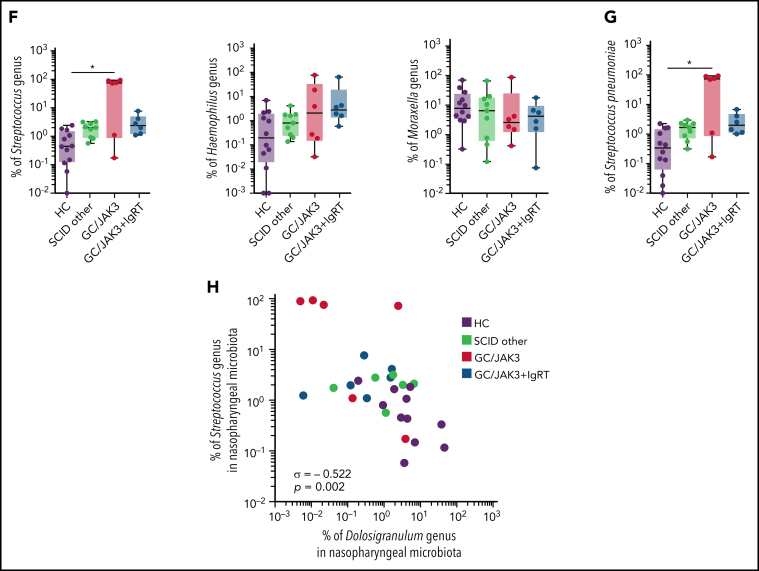
HSCT-treated GC/JAK3 patients without IVIG replacement therapy have nasopharyngeal microbiota dysbiosis. (A) Unsupervised principal coordinate (PC) analysis of 16S RNA sequencing Operational Taxonomic Units of the HC and HSCT-treated SCID patients along the first two PC axes, based on Bray-Curtis distances. The respective PERMANOVA test showing that nasopharynx microbiota from SCIDX/JAK3 patients is significantly different from HC. (B) The beta (β) diversity, calculated by using the Bray-Curtis, Jaccard, and Euclidean distances, among subjects according to group. (C) The alpha (α) diversity, calculated by using the Shannon index and Simpson index, in healthy and HSCT-treated SCID patients. Mean and standard error of mean values are indicated. (D) Bar plot showing the mean of the microbiota genus abundance (%) in healthy and HSCT-treated SCID patients. (E-F) Individual genus abundance (%) plots for selected ‘protective’ (E) and ‘pathobiont’ (F) genera in healthy and HSCT-treated SCID patients. (G) Individual S pneumoniae (%) plot in healthy and HSCT-treated SCID patients σ. (H) Individual correlation plot between Streptococcus genus abundance (%) and Dolosigranulum genus abundance (%). Panels B, E, F, and G: box plots with median ± minimum to maximum. P values were determined with the Kruskal-Wallis test followed by Dunn's posttest for multiple group comparisons; *P < .05, **P < .005, ***P < .001. In panel H, σ represents Spearman coefficient and p the P value. n.s., not significant.
Nasopharyngeal microbial communities in these different SCID patients were further characterized by annotation of the 16S rRNA data sets. It has been reported that the nasopharyngeal microbiota of healthy individuals is enriched in commensal bacteria, including Corynebacterium and Dolosigranulum genera.47, 48 We found a general reduction in Dolosigranulum and Comamonas genera in HSCT SCID patients compared with HC and a selective reduction in Corynebacterium, Cutibacterium, and Staphylococcus genera in GC/JAK3 patients compared with other SCID patients and HC (Figure 5D-E). These “cornerstone” bacterial communities (particularly Corynebacterium and Dolosigranulum genera) can reduce carriage of several pathobionts (S pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis) that may be present in normal healthy individuals.49, 50 Relative abundance of Streptococcus, Haemophilus, and Moraxella were not significantly increased in HSCT SCID-other patients compared with HC, although a higher abundance of Streptococcus and Haemophilus, genera were detected in GC/JAK3 patients who were not treated with IgRT (Figure 5D,F). This was in part due to the increased abundance of S pneumoniae (Figure 5G; supplemental Figure 5D). Finally, a significant negative correlation of S pneumoniae abundance with Dolosigranulum genus abundance could be detected in the nasopharynx (Figure 5H).
IgRT is an established treatment to combat infections in HSCT-treated SCID patients for whom S pneumoniae is a leading cause of disease.51 Nasopharyngeal samples from GC/JAK3 patients receiving IgRT clustered closer to SCID-other patients and HC (Figure 5A). Moreover, IgRT in GC/JAK3 patients “normalized” microbiota diversity (β Shannon and Simpson diversity indices) with higher representation of Corynebacterium and reduced levels of Streptococcus (Figure 5B-D). Moreover, we could confirm a decrease in S pneumoniae in GC/JAK3+IgRT patients (Figure 5G). Intriguingly, IgA level under IgRT correlated with microbial α-diversity indicating the intricate interplay between immune selection and maintenance of complex commensal communities (supplemental Figure 5E). Taken together, these data suggest that HSCT-treated GC/JAK3 patients without IgRT can present persistent nasopharyngeal microbial dysbiosis with expansion of bacteria associated with increased morbidity and mortality risk. Because IgRT appears to ameliorate the nasopharyngeal dysbiosis, one may consider potential use of IgRT in all GC/JAK3 patients to pre-empt or correct this abnormality.
Role for type 2 immunity and nasal IgA in maintaining commensal microbiota diversity and protection against “pathobiont” carriage
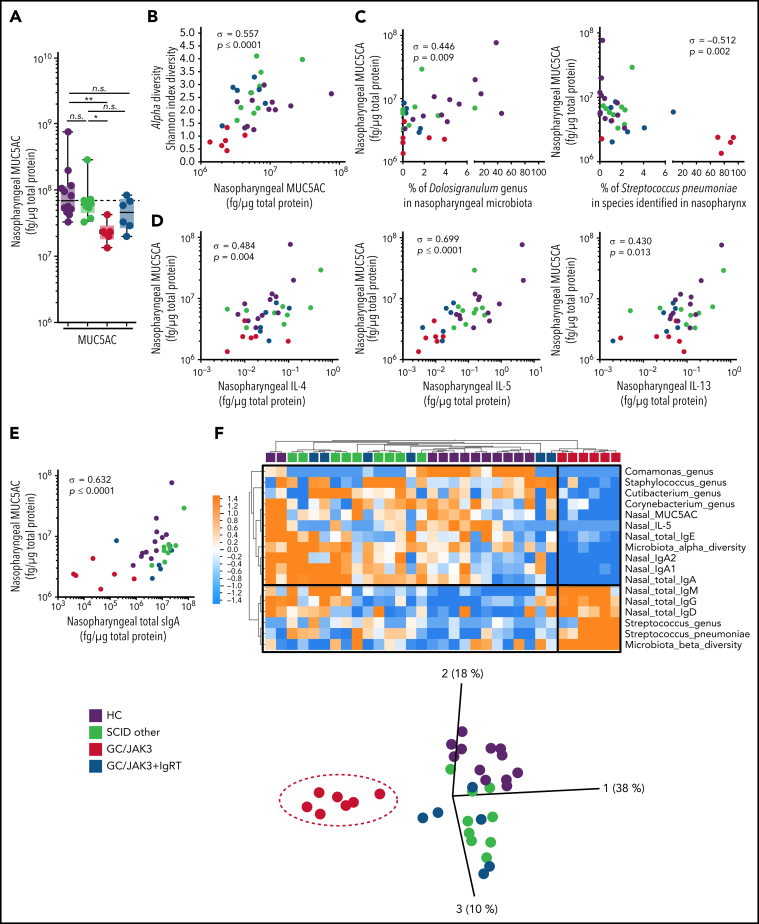
Secretory IgA is implicated in human nasopharyngeal microbial homeostasis52 and may protect mucosal surfaces from pathogen invasion through agglutination.53, 54 However, other “nonspecific” barriers, including a dense mucus layer, restrict commensal and pathobiont colonization at mucosal sites.55 Although total protein levels in nasopharyngeal samples from SCID patients and HC were not significantly different (supplemental Figure 3B), we found that GC/JAK3 patients (treated or not with IgRT) had markedly reduced MUC5AC levels compared with SCID-other and HC (Figure 6A). MUC5AC levels were positively correlated with α-diversity, Dolosigranulum, and Corynebacterium genera abundance and strongly negatively correlated with S pneumoniae abundance (Figure 6B-C). These results suggest that nasopharyngeal mucus plays a role in homeostasis of local commensal microorganisms and is selectively reduced after HSCT for GC/JAK3.
Figure 6.
Defective type 2 immunity underlies nasopharyngeal dysbiosis in HSCT-treated GC/JAK3 patients. (A) Nasopharyngeal MUC5AC concentration in HC and HSCT-treated SCID patients. (B) Individual correlation plot between nasopharyngeal MUC5AC concentration and α-diversity. (C) Individual correlation plot between nasopharyngeal MUC5AC concentration and Dolosigranulum genus abundance (%) or S pneumoniae abundance (%). (D) Individual correlation plot between nasopharyngeal MUC5AC concentration and nasopharyngeal IL-4, IL-5, and IL-13 concentration. (E) Individual correlation plot between nasopharyngeal MUC5AC concentration and nasopharyngeal secretory IgA (SIgA). (F) Heatmap representation of statistically different (P < .05) nasopharyngeal features between GC/JAK3 patients and the other patients and the three-dimensional principal coordinate analysis representation. Panel A: box plots with median ± minimum to maximum. P values were determined with the Kruskal Wallis test followed Dunn's posttest for multiple-group comparisons; *P < .05, **P < .005. In panels B through E, σ represents Spearman coefficient and p the P value. n.s., not significant.
We next looked for possible correlations in the cytokine data set that could associate with reduced MUC5AC levels in these patients with SCID. The reduction in nasopharyngeal IgA and type 2 cytokine levels in GC/JAK3 patients (Figure 2, Figure 3) paralleled the observed reductions in MUC5AC (Figure 6D-E), suggesting a possible link. Type 2 cytokines are known to regulate barrier immunity by promoting mucus production,29, 30 but other factors stimulate epithelial cell renewal and differentiation, including IL-22.56 IL-22 levels were correlated with MUC5AC levels (supplemental Figure 6C). All 2-parameter correlations are presented in supplemental Figure 6D. Together, these results identify critical soluble factors that coordinate local mucosal immune defense in the nasopharynx via mucus production. Finally, a supervised analysis of nasopharyngeal factors that were significantly different in GC/JAK3 patients reiterates the key parameters that integrate the unique mucosal immune profile of these individuals (Figure 6F), including reduced type 2 cytokines, reduced MUC5AC levels, reduced IgA, and microbial dysbiosis.
Discussion
In this report, we assess local mucosal immunity in the human nasopharynx in a well-characterized cohort of patients with SCID treated with curative HSCT. Previous studies on systemic immune reconstitution after bone marrow transplantation have highlighted differences in homeostasis of peripheral pools of innate and adaptive lymphocytes.1, 3, 18, 19 Pretransplant conditioning regimens may allow for differential engraftment of donor hematopoietic precursor cells and downstream myeloid and innate lymphocyte pools, the latter including NK cells and ILCs.3 The impact of differences in “innate reconstitution” on overall systemic immune responses appeared limited given the similar clinical profiles of these HSCT-treated SCID patients.3 These studies raised questions concerning the specific vs redundant functions of innate lymphocytes in human immunity.
Because ILCs abundantly populate mucosal sites, we explored their potential immune roles by comparing HSCT-treated SCID patients who exhibit variable innate lymphocyte reconstitution.3 Clear differences were observed in mucosal immune parameters in a subset of patients with SCID and genetic defects in GC or JAK3 that were not conditioned prior to HSCT. We documented a generalized reduction in mucosal type 2 immunity and IgA production and an inability to maintain “healthy” commensal bacterial communities consistent with a defect in nasopharyngeal mucosal barrier function. In contrast, other SCID etiologies (with or without myeloablative protocols before HSCT) exhibited normal type 2 cytokines and IgA production without nasal dysbiosis. Thus, the underlying SCID etiology is apparently a major factor for the observed defects in mucosal immunity.
Local IgA production is a hallmark of mucosal immunity and is largely driven by specific immune responses to resident microorganisms.57 Cytokines promote IgG and IgE production.58 In contrast, the key soluble factors that regulate switch to IgA are a matter of debate.57, 59 Previous studies have documented absence of serum IgA in about one-half of HSCT-treated GC/JAK3 patients.18, 36, 37, 38 Here we found that mucosal IgA was absent in all HSCT-GC/JAK3 patients examined, including those with normal circulating IgA. Interestingly, nasopharyngeal type 2 cytokines were most strongly perturbed in these patients, suggesting a causative link to mucosal IgA production. Type 2 cytokines can promote the survival and differentiation of tissue resident memory B cells and IgA-secreting plasma cells,60, 61, 62, 63, 64 thereby increasing IgA production.30, 65, 66, 67, 68 Along these lines, a recent report described a major role for ILC2-derived IL-5 in promoting local mucosal IgA production in mice.69 Whether locally generated IL-5 (by ILC2 or Th2 cells) regulates mucosal IgA production in humans remains unclear.
An alternative explanation for the observed IgA deficiencies may result from a defective immunoglobulin switch in residual GC/JAK3-deficient host B cells, the latter not being fully replaced by donor HSCT after nonablative conditioning.36 The inability of GC/JAK3-deficient B cells to respond to any γc-dependent cytokine might also reduce IgA switch mechanisms and result in selective IgA deficiency. However, nasopharyngeal IgG subclasses were not decreased in HSCT-treated GC/JAK3 patients, and serum IgG levels were normal, consistent with the ability of GC/JAK3-deficient host B cells to switch immunoglobulin isotypes.18 However, these patients have an intrinsic B-cell deficiency (defective response to IL-2, IL-9, and in part to IL-4) that can affect antibody production. γc-dependent signals in epithelial cells70 may also play a role. These observations suggest a contribution of impaired γc-dependent signaling pathways to the defective mucosal IgA production in these patients.
Th2 differentiation is considered as a “default” pathway that can be subverted to alternative T helper fates by environmental signals.71, 72 However, Th2 differentiation requires reinforcing signals through STAT6 (ie, IL-4 and IL-13) to upregulate GATA3 expression and seal Th2 cell fate.73 The defect in generation of Th2 cells in HSCT-treated GC/JAK3 patients may result from the absence of these STAT6-dependent signals, perhaps delivered by innate lymphocytes (ie, NK T cells, ILC2). In addition, ILC2 can prime tissue Th2 responses via DC recruitment.20, 21, 22, 23
The mucus layer that lines mucosal surfaces provides a physical barrier to commensal micro-organisms as well as pathogens and segregates “niches” harboring complex microbial biofilms.74 Secreted mucins (MUC5AC) are produced by goblet cells in the nasopharyngeal mucosa and tracheobronchial surface epithelium of the lower respiratory tract that act as a “scaffold” to present and organize secreted proteins such as secretory IgA, antimicrobial peptides, and cytokines. Type 2 cytokines (including IL-13) activate goblet cells to produce mucus.29, 30 Whether the loss of MUC5AC in GC/JAK3 patients secondary to reduced IL-13 predisposes these individuals to microbial dysbiosis will require further study.
Finally, nasopharyngeal IgA deficiency in HSCT-treated GC/JAK3 patients is associated with local microbial dysbiosis that may have been present prior to HSCT. It is well established that mucosal IgA plays a major role in regulating bacterial communities in the gut,46, 75 and the reduction in nasopharyngeal IgA observed in GC/JAK3 patients is correlated with loss of microbial diversity and frequently accompanied by increased pathobiont carriage. Although other immunoglobulin subclasses are present (and even elevated) in the nasopharynx in these patients and are able to coat bacteria, IgA remains a nonredundant immune factor required for microbial mucosal homeostasis.
Acknowledgments
The authors thank Sean Kennedy and Laurence Motreff (Biomics Platform) for 16S rRNA sequencing, Amine Ghozlane and Emna Achouri (HUB) for assistance with sequencing data analysis, and the Di Santo laboratory for discussions.
This study was supported by grants from the Institut Pasteur, INSERM, Agence National de la Recherche (ANR) (15-CE15-000-ILC3_MEMORY), and The European Research Council (695467-ILC_REACTIVITY). P.G. was supported in part by the Labex Milieu Intérieur (ANR 10-LBX-69 MI). The Biomics Platform is supported by France Génomique (ANR-10-INBS-09-09) and IBISA.
Footnotes
The raw 16SA sequence data were deposited in the National Center for Biotechnology Information Sequence Read Archive (accession number PRJNA772582). All other data sets generated during the current study are available upon reasonable request via e-mail to the corresponding author.
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Severe combined immunodeficiency (SCID) is a heterogeneous disease, but all subsets are treated with hematopoietic stem cell therapy (HSCT). In this Plenary paper, Goncalves et al investigate subtle heterogeneity of immune reconstitution, especially in patients with genetic defects in IL2R- γ or JAK3. This latter group of patients often receive nonmyeloablative HSCT, and despite that immune reconstitution evinces a local nasopharyngeal defect in type 2 cytokine production leading to mucosal IgA deficiency and microbial dysbiosis, the defect improved with immunoglobulin replacement therapy.
Authorship
Contribution: P.G. conducted experiments, analyzed the data, and prepared the manuscript; J.-M.D., T.E., V.B., C.P., A.L., A.C., and B.C. performed experiments; C.L. processed samples; D.D. provided logistical support and access to samples from normal individuals via the Milieu Intérieur Consortium; B.N. and A.F. were responsible for patient care, collected samples, designed experiments, and prepared the manuscript; and J.P.D.S. designed experiments, analyzed the data, obtained funding, supervised research, and prepared the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Supplementary Material
REFERENCES
- 1.Neven B, Leroy S, Decaluwe H, et al. Long-term outcome after hematopoietic stem cell transplantation of a single-center cohort of 90 patients with severe combined immunodeficiency. Blood. 2009;113(17):4114–4124. doi: 10.1182/blood-2008-09-177923. [DOI] [PubMed] [Google Scholar]
- 2.Castagnoli R, Delmonte OM, Calzoni E, Notarangelo LD. Hematopoietic stem cell transplantation in primary immunodeficiency diseases: current status and future perspectives. Front Pediatr. 2019;7:295. doi: 10.3389/fped.2019.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vély F, Barlogis V, Vallentin B, et al. Evidence of innate lymphoid cell redundancy in humans [published correction appears in Nat Immunol. 2016;17(12):1479] Nat Immunol. 2016;17(11):1291–1299. doi: 10.1038/ni.3553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bal SM, Bernink JH, Nagasawa M, et al. IL-1β, IL-4 and IL-12 control the fate of group 2 innate lymphoid cells in human airway inflammation in the lungs. Nat Immunol. 2016;17(6):636–645. doi: 10.1038/ni.3444. [DOI] [PubMed] [Google Scholar]
- 5.Simoni Y, Fehlings M, Kl⊘verpris HN, et al. Human innate lymphoid cell subsets possess tissue-type based heterogeneity in phenotype and frequency. Immunity. 2018;48(5):1060. doi: 10.1016/j.immuni.2018.04.028. [DOI] [PubMed] [Google Scholar]
- 6.Vivier E, Artis D, Colonna M, et al. Innate lymphoid cells: 10 years on. Cell. 2018;174(5):1054–1066. doi: 10.1016/j.cell.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Cherrier DE, Serafini N, Di Santo JP. Innate lymphoid cell development: a T cell perspective. Immunity. 2018;48(6):1091–1103. doi: 10.1016/j.immuni.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Fischer A, Rausell A. Primary immunodeficiencies suggest redundancy within the human immune system. Sci Immunol. 2016;1(6):eaah5861. doi: 10.1126/sciimmunol.aah5861. [DOI] [PubMed] [Google Scholar]
- 9.Berteloot L, Molina TJ, Bruneau J, et al. Alternative pathways for the development of lymphoid structures in humans. Proc Natl Acad Sci USA. 2021;118(29):82118. doi: 10.1073/pnas.2108082118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thibeault C, Suttorp N, Opitz B. The microbiota in pneumonia: from protection to predisposition. Sci Transl Med. 2021;13(576):eaba0501. doi: 10.1126/scitranslmed.aba0501. [DOI] [PubMed] [Google Scholar]
- 11.Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science. 2012;336(6086):1268–1273. doi: 10.1126/science.1223490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goncalves P, Charbit B, Lenoir C, Duffy D, Fischer A, Di Santo JP. Antibody-coated microbiota in nasopharynx of healthy individuals and IVIg-treated patients with hypogammaglobulinemia. J Allergy Clin Immunol. 2020;145(6):1686–1690.e4. doi: 10.1016/j.jaci.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Smith N, Goncalves P, Charbit B, et al. Distinct systemic and mucosal immune responses during acute SARS-CoV-2 infection. Nat Immunol. 2021;22(11):1428–1439. doi: 10.1038/s41590-021-01028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moor K, Fadlallah J, Toska A, et al. Analysis of bacterial-surface-specific antibodies in body fluids using bacterial flow cytometry. Nat Protoc. 2016;11(8):1531–1553. doi: 10.1038/nprot.2016.091. [DOI] [PubMed] [Google Scholar]
- 15.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72(1-2):248–254. doi: 10.1006/abio.1976.9999. [DOI] [PubMed] [Google Scholar]
- 16.Buckley RH, Schiff SE, Schiff RI, et al. Hematopoietic stem-cell transplantation for the treatment of severe combined immunodeficiency. N Engl J Med. 1999;340(7):508–516. doi: 10.1056/NEJM199902183400703. [DOI] [PubMed] [Google Scholar]
- 17.Haddad E, Landais P, Friedrich W, et al. Long-term immune reconstitution and outcome after HLA-nonidentical T-cell-depleted bone marrow transplantation for severe combined immunodeficiency: a European retrospective study of 116 patients. Blood. 1998;91(10):3646–3653. [PubMed] [Google Scholar]
- 18.Haddad E, Le Deist F, Aucouturier P, et al. Long-term chimerism and B-cell function after bone marrow transplantation in patients with severe combined immunodeficiency with B cells: a single-center study of 22 patients. Blood. 1999;94(8):2923–2930. [PubMed] [Google Scholar]
- 19.Borghans JA, Bredius RG, Hazenberg MD, et al. Early determinants of long-term T-cell reconstitution after hematopoietic stem cell transplantation for severe combined immunodeficiency. Blood. 2006;108(2):763–769. doi: 10.1182/blood-2006-01-009241. [DOI] [PubMed] [Google Scholar]
- 20.Oliphant CJ, Hwang YY, Walker JA, et al. MHCII-mediated dialog between group 2 innate lymphoid cells and CD4(+) T cells potentiates type 2 immunity and promotes parasitic helminth expulsion. Immunity. 2014;41(2):283–295. doi: 10.1016/j.immuni.2014.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gold MJ, Antignano F, Halim TYF, et al. Group 2 innate lymphoid cells facilitate sensitization to local, but not systemic, TH2-inducing allergen exposures. J Allergy Clin Immunol. 2014;133(4):1142–1148. doi: 10.1016/j.jaci.2014.02.033. [DOI] [PubMed] [Google Scholar]
- 22.Halim TYF, Rana BMJ, Walker JA, et al. Tissue-restricted adaptive type 2 immunity is orchestrated by expression of the costimulatory molecule OX40L on group 2 innate lymphoid cells. Immunity. 2018;48(6):1195–1207.e6. doi: 10.1016/j.immuni.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Min J, Li Z, Wang J, Zhang F, Li F, Ding J. ILC2s induces adaptive Th2-type immunity in acute exacerbation of chronic obstructive pulmonary disease. Eur J Immunol. 2019;49:445–446. doi: 10.1155/2019/3140183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gaylo-Moynihan A, Prizant H, Popović M, et al. Programming of distinct chemokine-dependent and -independent search strategies for Th1 and Th2 cells optimizes function at inflamed sites. Immunity. 2019;51(2):298–309.e6. doi: 10.1016/j.immuni.2019.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morita R, Schmitt N, Bentebibel SE, et al. Human blood CXCR5(+)CD4(+) T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity. 2011;34(1):108–121. doi: 10.1016/j.immuni.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lim AI, Li Y, Lopez-Lastra S, et al. Systemic human ILC precursors provide a substrate for tissue ILC differentiation. Cell. 2017;168(6):1086–1100.e10. doi: 10.1016/j.cell.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 27.van Unen V, Höllt T, Pezzotti N, et al. Visual analysis of mass cytometry data by hierarchical stochastic neighbour embedding reveals rare cell types. Nat Commun. 2017;8(1):1740. doi: 10.1038/s41467-017-01689-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sarzotti M, Patel DD, Li X, et al. T cell repertoire development in humans with SCID after nonablative allogeneic marrow transplantation. J Immunol. 2003;170(5):2711–2718. doi: 10.4049/jimmunol.170.5.2711. [DOI] [PubMed] [Google Scholar]
- 29.Wynn TA. Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat Rev Immunol. 2004;4(8):583–594. doi: 10.1038/nri1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moro K, Yamada T, Tanabe M, et al. Innate production of T(H)2 cytokines by adipose tissue-associated c-Kit(+)Sca-1(+) lymphoid cells. Nature. 2010;463(7280):540–544. doi: 10.1038/nature08636. [DOI] [PubMed] [Google Scholar]
- 31.Puttur F, Denney L, Gregory LG, et al. Pulmonary environmental cues drive group 2 innate lymphoid cell dynamics in mice and humans. Sci Immunol. 2019;4(36):eaav7638. doi: 10.1126/sciimmunol.aav7638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salimi M, Barlow JL, Saunders SP, et al. A role for IL-25 and IL-33-driven type-2 innate lymphoid cells in atopic dermatitis. J Exp Med. 2013;210(13):2939–2950. doi: 10.1084/jem.20130351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stier MT, Zhang J, Goleniewska K, et al. IL-33 promotes the egress of group 2 innate lymphoid cells from the bone marrow. J Exp Med. 2018;215(1):263–281. doi: 10.1084/jem.20170449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nussbaum JC, Van Dyken SJ, von Moltke J, et al. Type 2 innate lymphoid cells control eosinophil homeostasis. Nature. 2013;502(7470):245–248. doi: 10.1038/nature12526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nahm DH, Park HS. Correlation between IgA antibody and eosinophil cationic protein levels in induced sputum from asthmatic patients. Clin Exp Allergy. 1997;27(6):676–681. [PubMed] [Google Scholar]
- 36.Miggelbrink AM, Logan BR, Buckley RH, et al. B-cell differentiation and IL-21 response in IL2RG/JAK3 SCID patients after hematopoietic stem cell transplantation. Blood. 2018;131(26):2967–2977. doi: 10.1182/blood-2017-10-809822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buckley RH, Schiff SE, Sampson HA, et al. Development of immunity in human severe primary T cell deficiency following haploidentical bone marrow stem cell transplantation. J Immunol. 1986;136(7):2398–2407. [PubMed] [Google Scholar]
- 38.Buckley RH, Win CM, Moser BK, Parrott RE, Sajaroff E, Sarzotti-Kelsoe M. Post-transplantation B cell function in different molecular types of SCID. J Clin Immunol. 2013;33(1):96–110. doi: 10.1007/s10875-012-9797-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anthony RM, Kobayashi T, Wermeling F, Ravetch JV. Intravenous gammaglobulin suppresses inflammation through a novel T(H)2 pathway. Nature. 2011;475(7354):110–113. doi: 10.1038/nature10134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tjon ASW, van Gent R, Jaadar H, et al. Intravenous immunoglobulin treatment in humans suppresses dendritic cell function via stimulation of IL-4 and IL-13 production. J Immunol. 2014;192(12):5625–5634. doi: 10.4049/jimmunol.1301260. [DOI] [PubMed] [Google Scholar]
- 41.Kazatchkine MD, Kaveri SV. Immunomodulation of autoimmune and inflammatory diseases with intravenous immune globulin. N Engl J Med. 2001;345(10):747–755. doi: 10.1056/NEJMra993360. [DOI] [PubMed] [Google Scholar]
- 42.Fadlallah J, Sterlin D, Fieschi C, et al. Synergistic convergence of microbiota-specific systemic IgG and secretory IgA. J Allergy Clin Immunol. 2019;143(4):1575–1585.e4. doi: 10.1016/j.jaci.2018.09.036. [DOI] [PubMed] [Google Scholar]
- 43.Chen K, Cerutti A. New insights into the enigma of immunoglobulin D. Immunol Rev. 2010;237(1):160–179. doi: 10.1111/j.1600-065X.2010.00929.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen K, Xu W, Wilson M, et al. Immunoglobulin D enhances immune surveillance by activating antimicrobial, proinflammatory and B cell-stimulating programs in basophils. Nat Immunol. 2009;10(8):889–898. doi: 10.1038/ni.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Forsgren A, Brant M, Möllenkvist A, et al. Isolation and characterization of a novel IgD-binding protein from Moraxella catarrhalis. J Immunol. 2001;167(4):2112–2120. doi: 10.4049/jimmunol.167.4.2112. [DOI] [PubMed] [Google Scholar]
- 46.Fadlallah J, El Kafsi H, Sterlin D, et al. Microbial ecology perturbation in human IgA deficiency. Sci Transl Med. 2018;10(439):eaan1217. doi: 10.1126/scitranslmed.aan1217. [DOI] [PubMed] [Google Scholar]
- 47.de Steenhuijsen Piters WAA, Jochems SP, Mitsi E, et al. Interaction between the nasal microbiota and S. pneumoniae in the context of live-attenuated influenza vaccine. Nat Commun. 2019;10(1):2981. doi: 10.1038/s41467-019-10814-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kelly MS, Surette MG, Smieja M, et al. The nasopharyngeal microbiota of children with respiratory infections in Botswana. Pediatr Infect Dis J. 2017;36(9):e211–e218. doi: 10.1097/INF.0000000000001607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brugger SD, Bomar L, Lemon KP. Commensal-pathogen interactions along the human nasal passages. PLoS Pathog. 2016;12(7):e1005633. doi: 10.1371/journal.ppat.1005633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bomar L, Brugger SD, Yost BH, Davies SS, Lemon KP. Corynebacterium accolens releases antipneumococcal free fatty acids from human nostril and skin surface triacylglycerols. mBio. 2016;7(1):e01725–e01e15. doi: 10.1128/mBio.01725-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Engelhard D, Cordonnier C, Shaw PJ, et al. Infectious Disease Working Party of the European Bone Marrow Transplantation (IDWP-EBMT) Early and late invasive pneumococcal infection following stem cell transplantation: a European Bone Marrow Transplantation survey. Br J Haematol. 2002;117(2):444–450. doi: 10.1046/j.1365-2141.2002.03457.x. [DOI] [PubMed] [Google Scholar]
- 52.Bunker JJ, Erickson SA, Flynn TM, et al. Natural polyreactive IgA antibodies coat the intestinal microbiota. Science. 2017;358(6361):eaan6619. doi: 10.1126/science.aan6619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Binsker U, Lees JA, Hammond AJ, Weiser JN. Immune exclusion by naturally acquired secretory IgA against pneumococcal pilus-1. J Clin Invest. 2020;130(2):927–941. doi: 10.1172/JCI132005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roche AM, Richard AL, Rahkola JT, Janoff EN, Weiser JN. Antibody blocks acquisition of bacterial colonization through agglutination. Mucosal Immunol. 2015;8(1):176–185. doi: 10.1038/mi.2014.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ha U, Lim JH, Jono H, et al. A novel role for IkappaB kinase (IKK) alpha and IKKbeta in ERK-dependent up-regulation of MUC5AC mucin transcription by Streptococcus pneumoniae. J Immunol. 2007;178(3):1736–1747. doi: 10.4049/jimmunol.178.3.1736. [DOI] [PubMed] [Google Scholar]
- 56.Fujisawa T, Velichko S, Thai P, Hung LY, Huang F, Wu R. Regulation of airway MUC5AC expression by IL-1beta and IL-17A; the NF-kappaB paradigm. J Immunol. 2009;183(10):6236–6243. doi: 10.4049/jimmunol.0900614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bunker JJ, Bendelac A. IgA responses to microbiota. Immunity. 2018;49(2):211–224. doi: 10.1016/j.immuni.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Snapper CM, Finkelman FD, Paul WE. Regulation of IgG1 and IgE production by interleukin 4. Immunol Rev. 1988;102(1):51–75. doi: 10.1111/j.1600-065x.1988.tb00741.x. [DOI] [PubMed] [Google Scholar]
- 59.Cerutti A. The regulation of IgA class switching. Nat Rev Immunol. 2008;8(6):421–434. doi: 10.1038/nri2322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Scheeren FA, Naspetti M, Diehl S, et al. STAT5 regulates the self-renewal capacity and differentiation of human memory B cells and controls Bcl-6 expression. Nat Immunol. 2005;6(3):303–313. doi: 10.1038/ni1172. [DOI] [PubMed] [Google Scholar]
- 61.Malin S, McManus S, Cobaleda C, et al. Role of STAT5 in controlling cell survival and immunoglobulin gene recombination during pro-B cell development. Nat Immunol. 2010;11(2):171–179. doi: 10.1038/ni.1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Diehl SA, Schmidlin H, Nagasawa M, et al. STAT3-mediated up-regulation of BLIMP1 Is coordinated with BCL6 down-regulation to control human plasma cell differentiation. J Immunol. 2008;180(7):4805–4815. doi: 10.4049/jimmunol.180.7.4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Matsumoto R, Matsumoto M, Mita S, et al. Interleukin-5 induces maturation but not class switching of surface IgA-positive B cells into IgA-secreting cells. Immunology. 1989;66(1):32–38. [PMC free article] [PubMed] [Google Scholar]
- 64.Karasuyama H, Rolink A, Melchers F. Recombinant interleukin 2 or 5, but not 3 or 4, induces maturation of resting mouse B lymphocytes and propagates proliferation of activated B cell blasts. J Exp Med. 1988;167(4):1377–1390. doi: 10.1084/jem.167.4.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Drake LY, Iijima K, Bartemes K, Kita H. Group 2 innate lymphoid cells promote an early antibody response to a respiratory antigen in mice. J Immunol. 2016;197(4):1335–1342. doi: 10.4049/jimmunol.1502669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fort MM, Cheung J, Yen D, et al. IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity. 2001;15(6):985–995. doi: 10.1016/s1074-7613(01)00243-6. [DOI] [PubMed] [Google Scholar]
- 67.Moon BG, Takaki S, Miyake K, Takatsu K. The role of IL-5 for mature B-1 cells in homeostatic proliferation, cell survival, and Ig production. J Immunol. 2004;172(10):6020–6029. doi: 10.4049/jimmunol.172.10.6020. [DOI] [PubMed] [Google Scholar]
- 68.Beagley KW, Eldridge JH, Kiyono H, et al. Recombinant murine IL-5 induces high rate IgA synthesis in cycling IgA-positive Peyer's patch B cells. J Immunol. 1988;141(6):2035–2042. [PubMed] [Google Scholar]
- 69.Satoh-Takayama N, Kato T, Motomura Y, et al. Bacteria-induced group 2 innate lymphoid cells in the stomach provide immune protection through induction of IgA. Immunity. 2020;52(4):635–649.e4. doi: 10.1016/j.immuni.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 70.Laffort C, Le Deist F, Favre M, et al. Severe cutaneous papillomavirus disease after haemopoietic stem-cell transplantation in patients with severe combined immune deficiency caused by common gammac cytokine receptor subunit or JAK-3 deficiency. Lancet. 2004;363(9426):2051–2054. doi: 10.1016/S0140-6736(04)16457-X. [DOI] [PubMed] [Google Scholar]
- 71.Gieseck RL, III, Wilson MS, Wynn TA. Type 2 immunity in tissue repair and fibrosis. Nat Rev Immunol. 2018;18(1):62–76. doi: 10.1038/nri.2017.90. [DOI] [PubMed] [Google Scholar]
- 72.Lloyd CM, Snelgrove RJ. Type 2 immunity: expanding our view. Sci Immunol. 2018;3(25):eaat1604. doi: 10.1126/sciimmunol.aat1604. [DOI] [PubMed] [Google Scholar]
- 73.Zhu J, Guo L, Watson CJ, Hu-Li J, Paul WE. Stat6 is necessary and sufficient for IL-4's role in Th2 differentiation and cell expansion. J Immunol. 2001;166(12):7276–7281. doi: 10.4049/jimmunol.166.12.7276. [DOI] [PubMed] [Google Scholar]
- 74.Zanin M, Baviskar P, Webster R, Webby R. The interaction between respiratory pathogens and mucus. Cell Host Microbe. 2016;19(2):159–168. doi: 10.1016/j.chom.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sterlin D, Fadlallah J, Adams O, et al. Human IgA binds a diverse array of commensal bacteria. J Exp Med. 2020;217(3):e20181635. doi: 10.1084/jem.20181635. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.