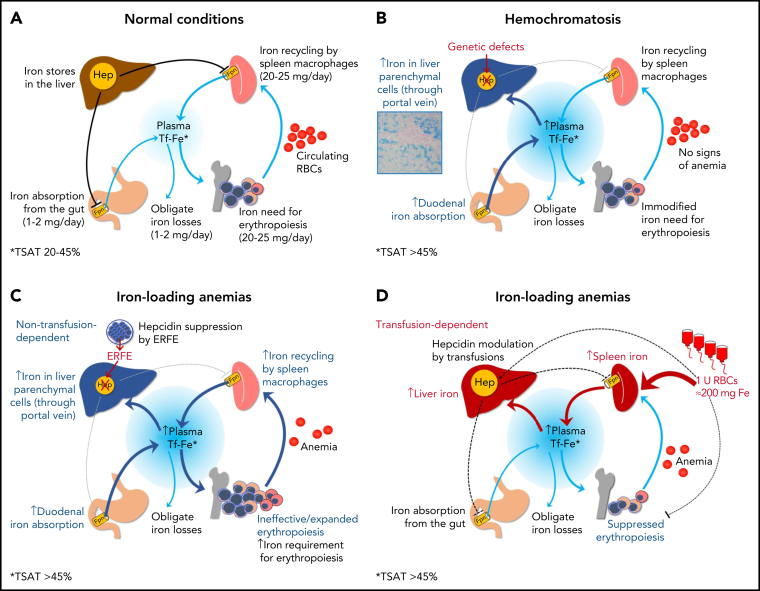
Figure 3.
Iron homeostasis in normal conditions (A) and mechanisms leading to iron accumulation in HC (B) and in iron-loading anemias that are nontransfusion-dependent (C) and transfusion-dependent (D). In HC, iron hyperabsorption through the portal vein leads to iron accumulation in liver parenchymal cells, initially with a typical portal-central gradient (see histology) and sparing of macrophages (Kupffer cells). In nontransfusion-dependent anemias with ineffective erythropoiesis, hepcidin insufficiency is also central to the pathogenesis of IO, but it is due to suppression by soluble factors (eg, ERFE) produced by ineffective/expanded erythroblasts rather than to a genetic defect in pathways regulating hepcidin synthesis. In transfusion-dependent anemias, regular red blood cells (RBCs) transfusions represent the major contributing factor to IO; in these conditions, hepcidin is relatively upregulated by iron but fluctuates in response to intermittent erythropoiesis suppression by transfusions.