Abstract
Background and Aims
Implantable cardioverter-defibrillators (ICDs) are critical for preventing sudden cardiac death (SCD) in arrhythmogenic right ventricular cardiomyopathy (ARVC). This study aims to identify cross-continental differences in utilization of primary prevention ICDs and survival free from sustained ventricular arrhythmia (VA) in ARVC.
Methods
This was a retrospective analysis of ARVC patients without prior VA enrolled in clinical registries from 11 countries throughout Europe and North America. Patients were classified according to whether they received treatment in North America or Europe and were further stratified by baseline predicted VA risk into low- (<10%/5 years), intermediate- (10%–25%/5 years), and high-risk (>25%/5 years) groups. Differences in ICD implantation and survival free from sustained VA events (including appropriate ICD therapy) were assessed.
Results
One thousand ninety-eight patients were followed for a median of 5.1 years; 554 (50.5%) received a primary prevention ICD, and 286 (26.0%) experienced a first VA event. After adjusting for baseline risk factors, North Americans were more than three times as likely to receive ICDs {hazard ratio (HR) 3.1 [95% confidence interval (CI) 2.5, 3.8]} but had only mildly increased risk for incident sustained VA [HR 1.4 (95% CI 1.1, 1.8)]. North Americans without ICDs were at higher risk for incident sustained VA [HR 2.1 (95% CI 1.3, 3.4)] than Europeans.
Conclusions
North American ARVC patients were substantially more likely than Europeans to receive primary prevention ICDs across all arrhythmic risk strata. A lower rate of ICD implantation in Europe was not associated with a higher rate of VA events in those without ICDs.
Keywords: Arrhythmogenic right ventricular cardiomyopathy, Sudden cardiac death, Ventricular arrhythmia, Primary prevention, Implantable cardioverter-defibrillator
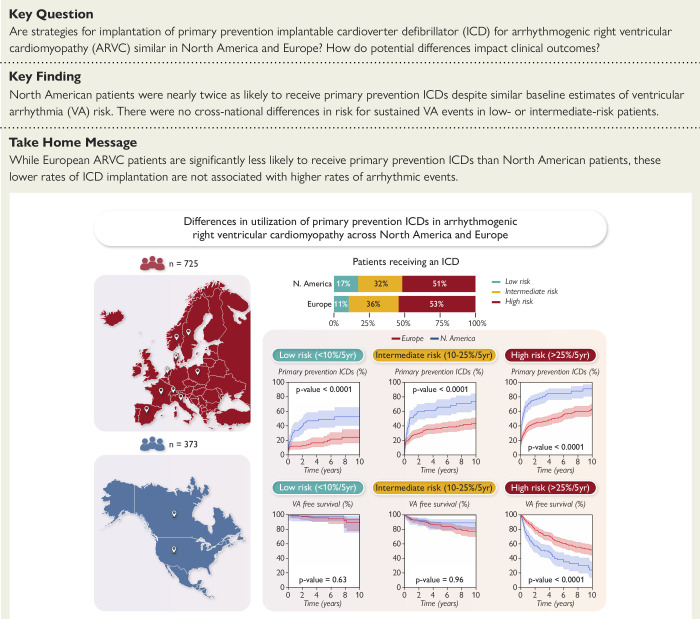
Structured Graphical Abstract
Structured Graphical Abstract.
In this multi-national cohort of arrhythmogenic right ventricular cardiomyopathy patients, North American patients were much more likely to receive implantable cardioverter-defibrillator (ICDs) than European patients across all risk strata. Differences in rates of sustained ventricular arrhythmia (VA) between North America and Europe were limited to patients identified as high-risk by baseline risk estimates.
See the editorial comment for this article ‘Transatlantic differences in the use of implantable cardioverter defibrillators in arrhythmogenic right ventricular cardiomyopathy', by P.M. Elliott, https://doi.org/10.1093/eurheartj/ehae022.
Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is an inherited cardiomyopathy characterized by progressive fibro-fatty replacement of the myocardium which predisposes patients to ventricular arrhythmias (VAs) and sudden cardiac death (SCD).1 Prevention of SCD through the placement of an implantable cardioverter-defibrillator (ICD) thus represents a mainstay of ARVC management. However, given the significant drawbacks and potential long-term complications associated with ICDs in this young population,2 appropriate patient selection is critical.
While there is consensus that ARVC patients with a history of prior sustained VA or aborted SCD merit the placement of secondary prevention ICDs,3 there is much more variability in patient selection for primary prevention implantation. Prior studies identifying predictors of sustained VA and SCD in ARVC patients4–6 have culminated in the publication of a series of consensus statements and guidelines3,7,8 and, more recently, in the development and external validation of an individualized risk prediction calculator for sustained VA and SCD in ARVC patients without a prior history of VA (ARVCrisk.com).9–11 The risk of sustained VA and SCD of each individual ARVC patient is now better understood than at any time previously. Cross-continental differences in ICD utilization have been observed in other forms of inherited heart disease,12 with patients in North American centres receiving more aggressive SCD prevention than those elsewhere. Similar trends may be suspected in ARVC as well.
Thus, the aim of the present study is to examine regional differences in primary prevention ICD implantation practice patterns using a large, multi-national cohort of primary prevention ARVC patients and to assess the impact of these differences on clinically relevant arrhythmic outcomes. In this study, we (i) explored regional differences in rates of primary prevention ICD implantation, (ii) examined if these differences can be accounted for by disparate ARVC patient risk profiles, (iii) determined if differing regional primary prevention ICD implantation patterns translate into adverse arrhythmic outcomes, and (iv) examined whether sex influences clinical practice regarding ICD implantation.
Methods
Study population
This was an observational, retrospective cohort study. The study population was drawn from 11 European and North American countries (see Supplementary data online, Table S1). Patients were included in the analysis if they (i) were diagnosed prior to January 2022 with definite ARVC by the current 2010 Task Force Criteria (TFC)13 and (ii) had not experienced prior sustained VA or SCD at the time of their ARVC diagnosis. This study conformed to the Declaration of Helsinki and was approved by local ethics and/or institutional review boards. To maintain patient confidentiality, data and study materials have not been made publicly available, but a limited data set may be made available upon request.
Data collection
Data were collected independently by each centre according to a standardized set of definitions, as previously published.9 Outcomes were adjudicated at each centre via review of electrocardiogram (ECG) tracings, ICD interrogation tracings, as well as medical and death records. Genetic variants were adjudicated according to the American College of Medical Genetics and Genomics guidelines by a consensus of specialists in cardiac genetics.14
Study outcomes
Two primary outcomes were examined in this study: (i) implantation of an ICD for primary prevention of SCD and (ii) first sustained VA after ARVC diagnosis. Primary prevention ICDs were defined as ICDs implanted prior to the first occurrence of sustained VA. Sustained VA was defined as a composite of the occurrence of SCD, aborted SCD, spontaneous sustained ventricular tachycardia (VT) (defined as VT lasting ≥30 s at ≥100 b.p.m. or with haemodynamic compromise requiring cardioversion), ventricular fibrillation/flutter (VF), or an appropriate ICD intervention. Secondary outcomes including the first episode of rapid and life-threatening VA (LTVA, defined as a composite of SCD, aborted SCD, VF, or VT >250 b.p.m.), heart transplantation, cardiovascular mortality, and all-cause mortality were also recorded. Protected patients were defined as those with a primary prevention ICD, while unprotected patients were defined as those without an ICD.
Statistical analyses
Analyses were performed in PyCharm software version 2021.2 (JetBrains Inc., Boston, MA, USA) and the open-source Pandas, Lifelines, and Statsmodels statistical code libraries. Categorical variables were summarized as frequencies (%) and compared using proportional z-tests. Continuous variables were presented as mean ± standard deviation or median [interquartile range (IQR)] and compared using independent sample Student’s t-tests or Mann–Whitney U tests, as appropriate. The overall probabilities of (i) cumulative incidence of primary prevention ICD placement and (ii) survival free from sustained VA were estimated using the Kaplan–Meier method. Event rates are reported as averages over the 5-year period following initial ARVC diagnosis. Follow-up duration was calculated from the date of diagnosis to the date of a study outcome or censoring, which was defined as death from any other cause, heart transplantation, or the most recent follow-up visit at which the outcomes could be ascertained. In a sub-analysis of first VA event in unprotected (those without ICD) and protected (those with ICD) patients, follow-up time for unprotected patients was additionally censored at the time of ICD placement, and follow-up time for protected patients was defined relative to the date of ICD implantation (rather than relative to the date of ARVC diagnosis). Multivariable Cox regression modelling was performed to assess the association between geographic location and both ICD implantation and sustained VA events (considered separately), with adjustment for each of the individual VA risk factors included in the ARVC risk calculator (see Supplementary data online, Methods, page 2). Association between geographic location and sustained VA events was also adjusted for the presence of ICD, which was modelled as a time-dependent variable. Missing data were imputed using multiple imputation with chained equations; a more detailed description of imputation and missingness is presented in the Supplementary data online, Methods. Sensitivity analysis was performed using visual comparison of Kaplan–Meier survival with an Aalen–Johansen survival estimator allowing for competing risks from cardiac transplantation and non-arrhythmic death. Competing risks did not impact results.
Sub-group analyses
Kaplan–Meier survival curves were also generated for a series of patient sub-groups, and log-rank (LR) testing was used to assess differences between groups. Patients were divided according to (i) whether they received treatment at a North American (Canada or the USA) vs. European centre (Denmark, France, Italy, the Netherlands, Norway, Poland, Spain, Sweden, or Switzerland), (ii) their baseline predicted risk for VA—defined as low- (<10%/5 years), intermediate- (10%–25%/5 years), or high-risk (>25%/5 years)—and (iii) patient sex. Here, geographic groupings were based upon similarities in rates of ICD implantation (see Supplementary data online, Figure S1). Baseline 5-year VA risk predictions were generated using the ARVC risk calculator (www.arvcrisk.com) as previously described;9,10 a more detailed description is presented in the Supplementary data online, Methods.
Additional examination of ICD implantation and incident VA event rates stratified by temporal era of ARVC diagnosis are included as a Supplementary data online, Analysis. Furthermore, an additional analysis with follow-up times censored at 3 years to account for different follow-up times between the two cohorts was performed as a sensitivity analysis, also included in the Supplementary data online, Analysis.
Results
Study population
The study population consisted of 1098 patients with definite ARVC and no history of sustained VA at the time of diagnosis, of whom 1043 (95.0%) did not have an ICD at the time of diagnosis. Exactly half of the patients (n = 549, 50.0%) were male, nearly all were white (98.1%), and the average age at the time of diagnosis was 40.3 ± 16 years. About one-third (n = 373, 34.0%) of patients were enrolled in North American centres, while two-thirds (n = 725, 66.0%) were enrolled in 29 European centres. While there were only two US-based registries included, the Johns Hopkins ARVC Registry enrols patients from across the nation. Patients included in the Johns Hopkins Registry cohort were managed by 133 cardiovascular centres. More than half of the patients were probands, defined as the first affected individual in a family seeking medical attention for ARVC (n = 640, 58.3%). Of the 857 patients (78.1%) who underwent genetic testing, 576 (67.2%) were identified as having a causal (pathogenic or likely pathogenic) variant. Other clinical and demographic characteristics are summarized in Table 1. Characteristics of patients contributed by each country are shown in Supplementary data online, Table S2.
Table 1.
Baseline clinical characteristics
| Variable | All Patients (n = 1098) | European (n = 725) | North American (n = 373) | P value |
|---|---|---|---|---|
| Age (years) | 40.3 (±15.8) | 42.3 (±15.7) | 36.3 (±15.2) | <.0001 |
| Female sex | 549 (50.0%) | 330 (45.5%) | 219 (58.7%) | <.0001 |
| Male sex | 549 (50.0%) | 395 (54.5%) | 154 (41.3%) | <.0001 |
| History of syncope | 117 (10.7%) | 78 (10.8%) | 39 (10.5%) | .88 |
| # ECG leads w/ TWI | 3.5 (±2.2) | 3.6 (±2.2) | 3.3 (±2.1) | .051 |
| log(PVC count) | 6.6 (±2.5) | 6.7 (±2.4) | 6.2 (±2.8) | .0072 |
| History of NSVT | 454 (46.9%) | 293 (45.5%) | 161 (49.7%) | .38 |
| RVEF (%) | 43.6 (±10.9) | 43.9 (±11.0) | 43.1 (±10.8) | .21 |
| LVEF (%) | 56.3 (±9.3) | 55.6 (±9.5) | 57.7 (±8.5) | .0006 |
| LVEF < 50% | 186 (16.9%) | 135 (18.6%) | 51 (13.7%) | .038 |
| LVEF < 35% | 34 (3.1%) | 27 (3.7%) | 7 (1.9%) | .094 |
| 5-year VA risk (ARVC calculator %) | 19.3 [10.3; 36.5] | 19.2 [10.4; 33.7] | 19.7 [9.8; 39.9] | .59 |
| Genetic testing | 857 (78.1%) | 515 (71.0%) | 342 (91.7%) | <.0001 |
| Proband status | 640 (58.3%) | 446 (61.5%) | 194 (52.0%) | .0025 |
| Gene: PKP2 | 389 (45.4%) | 234 (45.4%) | 155 (45.3%) | .97 |
| Gene: DSP | 73 (8.5%) | 43 (8.3%) | 30 (8.8%) | .83 |
| Gene: PLN | 29 (3.4%) | 24 (4.7%) | 5 (1.5%) | .011 |
Variables are expressed as frequency (%), mean ± standard deviation, or median (IQR). Total number of patients for a given variable mentioned if missing data.
PKP2, plakophilin-2; DSP, desmoplakin; PLN, phospholamban.
Outcomes
During a median follow-up of 5.1 (IQR: 2.4; 9.5) years, 554 patients (50.5%) received primary prevention ICDs. Average ICD implantation rate was 9.5%/year (95% CI 8.8, 10.2). A total of 286 patients (26.0%) developed the composite VA outcome, at an average rate of 4.8%/year (95% CI 4.2, 5.4). Within the composite VA outcome, the most common first sustained VA was appropriate ICD therapy (n = 177, 62.1%), followed by spontaneous sustained VT (n = 89, 31.2%), aborted SCD (n = 14, 5.0%), and SCD (n = 6, 2.1%). Life-threatening VA (VA >250 b.p.m., VF, or aborted SCD/SCD) was experienced by 102 (9.3%) patients. At the last follow-up, 45 patients (4.1%) had died and 35 (3.2%) had undergone heart transplantation.
North American vs. European centres
Median follow-up (without event censoring) was longer for European [5.6 (IQR 2.9; 10.4) years] compared with North American [3.8 (IQR 1.5, 7.5) years] patients. European patients were older at the time of diagnosis (42.3 ± 16 vs. 36.3 ± 15 years, P < .0001) and more likely to be probands (61.5% vs. 52.0%, P = .0025). While the rates of genetic testing were much higher in North America (91.7% vs. 71.0%, P < .0001), genotype distributions in those tested were similar, except for a higher prevalence of a specific pathogenic phospholamban (PLN) variant in the Dutch population (see Supplementary data online, Table S2).
While the median baseline predictions of 5-year sustained VA risk were similar between North Americans and Europeans [19.7% (IQR 10%; 40%) vs. 19.2% (IQR 10%; 34%), P = .59], the distribution of predicted risk within each risk sub-group differed (see Supplementary data online, Table S3). Predicted 5-year VA risk was similar in the low- and intermediate-risk groups, but the risk distribution of North American patients in the high-risk group was more skewed towards higher risk than their European counterparts [predicted 5-year VA risk: 43.9% (IQR: 34%, 60%) vs. 41.7% (IQR: 30%, 55%), P = .024].
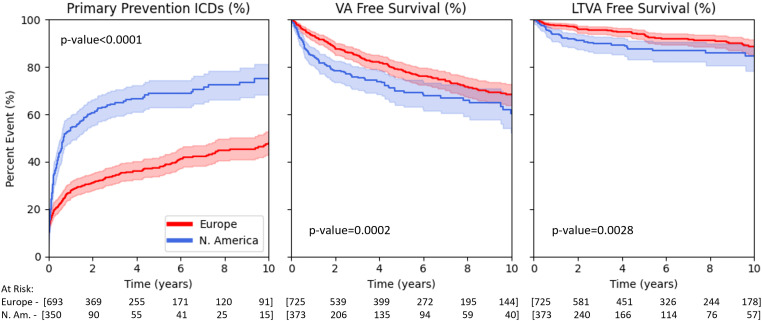
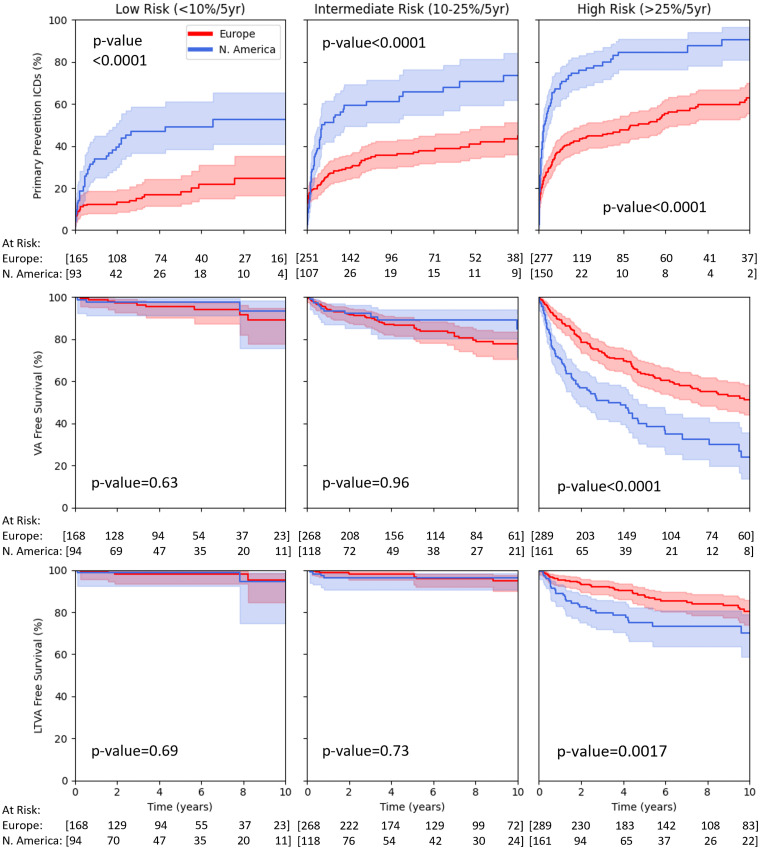
Overall, the rate of primary prevention ICD use was significantly higher in North Americans than in Europeans (13.8%/year vs. 7.5%/year, LR P < .0001) (Figure 1, left panel). This remained true across all baseline risk groups (Figure 2, top row). In multivariable Cox regression, the likelihood of receiving an ICD was 3.1-fold (95% CI 2.5, 3.8) higher for North Americans (Table 2).
Figure 1.
Cumulative rates of (left) primary prevention ICD implantation, (middle) sustained VA-free survival, and (right) LTVA-free survival (defined as VT at >250 b.p.m. or aborted SCD) according to geographic cohort. Shaded areas present 95% confidence intervals. Statistical significance was assessed using log-rank testing.
Figure 2.
Cumulative rates of (top row) primary prevention ICD implantation, (centre row) sustained VA-free survival, and (bottom row) LTVA-free survival (defined as VT at >250 b.p.m. or aborted SCD) in low-risk (left column; <10% 5-year VA risk), intermediate-risk (middle column; 10%–25% 5-year VA risk), and high-risk (right column; >25% 5-year VA risk) sub-groups according to geographic cohort. Shaded areas present 95% confidence intervals. Statistical significance was assessed using log-rank testing.
Table 2.
Multivariable Cox regression
| ICD implantation | Sustained VA event | |||
|---|---|---|---|---|
| Multivariable Cox HR (95% CI) | P value | Multivariable Cox HR (95% CI) | P value | |
| North American location | 3.084 (2.521; 3.774) | <.0001 | 1.355 (1.046; 1.754) | .021 |
| Age (years) | 0.999 (0.993; 1.005) | .69 | 0.987 (0.979; 0.995) | .0015 |
| Male sex | 1.215 (0.997; 1.479) | .053 | 1.840 (1.429; 2.369) | <.0001 |
| # ECG leads w/ TWI | 1.052 (1.002; 1.105) | .041 | 1.046 (0.987; 1.108) | .13 |
| log(PVC count) | 1.039 (0.989; 1.092) | .13 | 1.157 (1.073; 1.248) | .0002 |
| History of syncope | 2.272 (1.728; 2.988) | <.0001 | 1.679 (1.234; 2.283) | .0010 |
| History of NSVT | 1.726 (1.387; 2.149) | <.0001 | 2.325 (1.741; 3.106) | <.0001 |
| RVEF (%) | 0.984 (0.975; 0.993) | .0007 | 0.981 (0.970; 0.992) | .0008 |
| Presence of ICD | NA | NA | 3.283 (2.497; 4.317) | <.0001 |
Multivariable Cox regression assessing associations between geographic location (North American vs. European centres) and both ICD implantation and sustained VA event. In assessment of association with sustained VA events, presence of ICD was modelled as a time-dependent variable. Hazard ratios (HR) are presented along with 95% confidence intervals (CI).
Rates of sustained VA were significantly higher in North Americans (6.0%/year vs. 4.2%/year, LR P = .0002) (Figure 1, middle panel), as were rates of LTVA (2.5%/year vs. 1.2%/year, LR P = .0028) (Figure 1, right panel). In multivariable Cox regression, the adjusted risk for sustained VA was 1.4-fold (95% CI 1.1, 1.8) higher for North Americans (Table 2). However, when stratified by baseline VA risk, the increased rate of sustained VA events and LTVA in North Americans was isolated to the high-risk group, while no differences were observed in either the low- or intermediate-risk groups (Figure 2, Supplementary data online, Table S4).
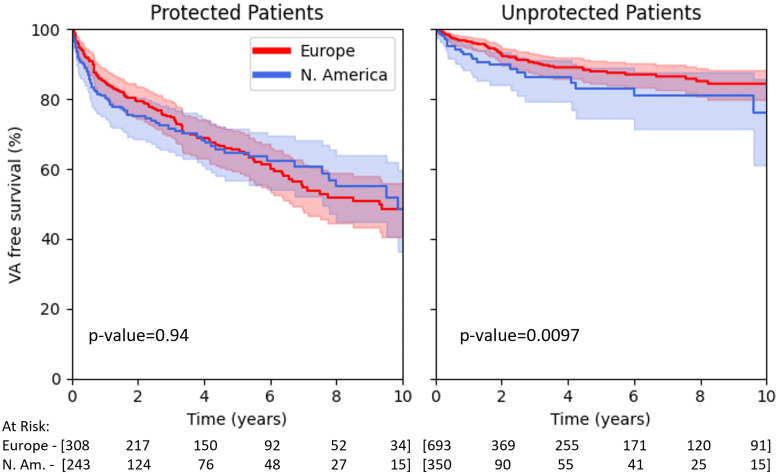
The difference in VA event rates between North Americans and Europeans was driven predominantly by increased rates of appropriate ICD therapy [75/106 (70.8%) vs. 102/180 (56.7%) of sustained VA events, P = .010]. There were no differences in the proportion of sustained VA events that were either aborted SCD [6/75 (8.0%) vs. 8/180 (4.4%), P = .25] or SCD [2/75 (2.7%) vs. 4/180 (2.2%), P = .83]. Rates of sustained VA in ICD protected patients were also similar between North American and European patients (7.1%/year vs. 6.9%/year, LR P = .94). In contrast, unprotected North Americans had higher rates of sustained VA events (3.4%/year vs. 2.4%/year, LR P = .010) (Figure 3), with an adjusted HR of 2.1 (95% CI: 1.3, 3.4) (see Supplementary data online, Table S5). When stratified by baseline risk, however, this difference in VA events for unprotected patients was only appreciated in high-risk patients (10.0%/year vs. 4.3%/year, LR P < .0001), while no difference was observed in either low- (0.2%/year vs. 0.7%/year, LR P = .50) or intermediate-risk groups (1.0%/year vs. 1.9%/year, LR P = .87) (see Supplementary data online, Figure S2).
Figure 3.
Cumulative survival free from sustained VA in protected (patients with primary prevention ICD) and unprotected (patients without primary prevention ICD) according to geographic cohort. For protected patients, time 0 is the time of ICD implantation. Shaded areas present 95% confidence intervals. Statistical significance was assessed using log-rank testing.
Finally, Europeans had higher incidence of both heart failure–related death (n = 18, 2.5% vs. n = 1, 0.3%; P = .0077) and non-cardiac death (n = 13, 1.8% vs. n = 0, 0.0%; P = .0093).
Male vs. female
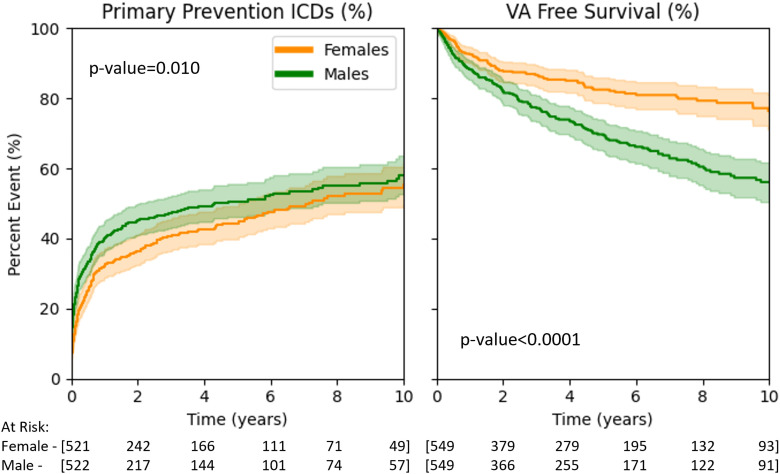
Men received primary prevention ICDs at a slightly higher rate compared with women (10.1%/year vs. 8.8%/year, LR P = .010), but the rate of VA events was much higher in men (6.1%/year vs. 3.5%/year, LR P < .0001) (Figure 4). In multivariable Cox regression, male sex was a strong independent risk factor for sustained VA [HR 1.9 (95% CI: 1.5, 2.4)] but not for ICD implantation [HR 1.2 (95% CI: 0.99, 1.4)]. When patients were further stratified by geographic location (see Supplementary data online, Figure S3 and Table S6), the rate of ICD implantation was likewise slightly higher in European men compared with European women as was the rate in North American men compared with North American women. In Europe, however, there was a pronounced difference in the rate of sustained VA events in men vs. women, while rates of sustained VA in North America were statistically similar in men and women.
Figure 4.
Cumulative rates of (left) primary prevention ICD implantation and (right) sustained VA-free survival according to sex. Shaded areas present 95% confidence intervals. Statistical significance was assessed using log-rank testing.
Discussion
Main findings
In the largest international cohort of primary prevention ARVC patients to date, we found a nearly two-fold higher rate of primary prevention ICD implantation in North American compared with European centres. This difference was consistent across all calculated VA risk groups. Rates of sustained VA, including all VA, LTVA, and unprotected VA, were also globally higher in North Americans than Europeans, but after stratifying by baseline risk, differences in the incidence of sustained VA between groups were limited to high-risk patients (Structured Graphical Abstract). Sex-based differences in primary prevention ICD implantation were also noteworthy, with women having only slightly lower rates of ICD implantation compared with men despite substantially lower VA event rates.
Implantable cardioverter-defibrillator implantation and ventricular arrhythmias during follow-up
The rate of primary prevention ICD implantation was significantly higher in the North American cohort than in the European cohort, and this difference was consistent across all pre-specified VA risk groups. This lower threshold for primary prevention ICD implantation in ARVC patients from North America was consistent with previously observed cross-continental trends in the utilization of ICDs for other indications.15,16 Particular to primary prevention devices, higher ICD utilization in North America has also been demonstrated in both hypertrophic cardiomyopathy12 and heart failure patients.17 We also observed higher rates of both VA and LTVA events (VA >250 b.p.m., VF, or aborted SCD/SCD) in North American patients. While higher VA event rates could appear to justify higher primary prevention ICD implantation rates in North America, there are a number of important points to consider in the interpretation of these findings.
First, the primary driver of the differences in rates of our composite VA outcome was appropriate ICD therapy. Given the much higher prevalence of ICDs in North Americans, this suggests a component of surveillance bias that predisposes towards increased event rates in North Americans. However, sustained VA event rates were also higher in unprotected North American patients (those without ICDs). Increased surveillance in ICD recipients therefore does not fully account for the observed differences in VA event rates. Second, when patients were further stratified by baseline 5-year VA risk, the higher North American VA and LTVA event rates were isolated to the high-risk group and there was no difference in VA or LTVA event rates in the low- and intermediate-risk groups. A similar pattern was observed in unprotected patients. Low- and intermediate-risk European patients were thus no more likely than their North American counterparts to experience the most clinically significant events—either LTVA or VA without the protection of an ICD—despite a significantly lower utilization of primary prevention ICDs. Finally, there was a skew towards higher risk in the sub-group of North American patients for whom baseline VA risk was predicted to be >25% at 5 years (high-risk) compared with similarly categorized European patients. This skewed baseline risk distribution could also partially account for the overall increased rate of VA events observed in North Americans.
Interestingly, despite the higher rate of ICDs implanted, more unprotected high-risk North American patients experienced VA events compared with similarly unprotected Europeans. The exact reason for this discrepancy is unclear but may relate to cultural differences in the perception of risk, differing approaches to medical decision-making, different lifestyles and sports regulations, or more difficult access to ICD use for some individuals in the US privatized healthcare system.18,19
Phenotypic differences and relationship to outcomes
Some phenotypic differences between European and American patients should be highlighted while interpreting these results. European patients were significantly older, more likely to be probands, and less likely to have undergone genetic testing. In combination, these features suggest that European patients enrolled in the included registries received their diagnosis at a later stage of the disease process compared with included North American patients, who in turn were more likely to be identified via family screening and genetic testing. Consistent with this hypothesis, European patients were also more likely to undergo heart transplantation or suffer heart failure–related death. However, while the higher rate of probands within the European cohort would be expected to translate to a higher rate of VA events,20 we observed the opposite. The possibility that a non-negligible group of European patients had a VA or SCD event prior to a diagnosis of ARVC, and would thereby be excluded from this primary prevention cohort, cannot be ruled out. Mechanistic21 and clinical22,23 evidence have also suggested that the ARVC disease process may be characterized by an early, electrically active phase during which unstable VAs occur prior to significant structural alterations. In keeping with this, recent data tracking ARVC patients longitudinally over time have also suggested that 5-year VA risk drops by nearly 50% between the time of initial diagnosis and 5-year follow-up.24,25 It is therefore possible that enrolment of European patients later in the disease process may have contributed to their observed lower rate of VA events. Importantly, prior studies have demonstrated adequate calibration of the ARVC risk calculator in both European and North American patients,9,10 and thus, these phenotypic discrepancies are accounted for during calculation of VA risk.
Sex differences
One of the most striking findings of our study resides in differences in primary prevention ICD use in men compared with women. Consistent with prior data supporting the role of male sex as an important independent risk factor for VA events in ARVC,9,10,20,26 we observed a strong association between male sex and risk for VA that was matched by a nearly two-fold higher rate of VA events per year in men. In contrast, the average rate of ICD implantation was only slightly higher in men than women and its association with sex did not meet statistical significance on multivariable testing. When the role of sex was further examined from the perspective of geographic location, this mismatch between ICD utilization and observed VA event rates was most prominent in European patients.
This surprising finding contrasts with the usual tendency to undertreat women in many areas of cardiovascular diseases,27–29 including ICD implantation.30 These results could highlight an under-appreciation of male sex as an important independent risk factor for VA in ARVC. Alternatively, other pragmatic reasons such as differing tolerance to the risk of SCD vs. the risk of ICD complications according to sex may have played a role in these results.
Clinical implications
Accurate identification of patients at high risk for SCD is central to patient selection for primary prevention ICD implantation. This study provides direct insight into real-world practices related to the utilization of primary prevention ICDs in ARVC, as well as the impact of these strategies on patient outcomes. Critically, lower implantation rates in Europe, especially in low- and intermediate-risk patients, did not result in higher numbers of adverse VA events in unprotected patients (those without ICD). These results support the safety of a more lenient approach to ICD implantation in ARVC, particularly for low- and intermediate-risk patients. Rates of ICD implantation were also disproportionately high in female patients relative to their observed VA event rates. This points towards a possible under-appreciation of male sex as an important risk factor for VA events in ARVC which may be most pronounced in European patients. That said, European and North American cohorts demonstrated a number of key differences in their characteristics, and it is possible that European patients represent a less arrhythmogenic phenotype due to their assessment at a later stage of disease progression. The findings above should thus be interpreted in this context. Nonetheless, the ARVC risk calculator9 provides a continuum of patient risk that offers quantitative guidance in the nuanced decision-making process that underlies primary prevention ICD implantation. While the clinical impact of the ARVC risk calculator, which due to its recent introduction is not reflected in these data, remains to be seen, its use permits a more accurate comparison of otherwise similar ARVC patients.
Limitations
This is a retrospective, observational cohort study with a population drawn from tertiary care centres across North America and Europe. Due to the retrospective nature of this work, there may be risk factors that were not accounted for in our analysis that could have biased our results. In particular, the use of ICDs in these centres might not reflect the full spectrum of ARVC disease in the general population or the full spectrum of management of ARVC in non-tertiary care centres. The sub-population of patients followed at tertiary centres and included in these registries might also vary in different countries. While the grouping of patients by geographical origin was necessary to achieve comparisons of cohorts of adequate sizes and was supported by similarities in North American centres vs. European centres, regional and national heterogeneities certainly do exist within these two groups. There was also no central adjudication of non-arrhythmic death or cardiac transplantation, and we cannot exclude the possibility of ascertainment bias in these results.
Additionally, the primary VA outcome, designed to capture all VA events, is an imperfect surrogate for (aborted) SCD, which did not occur at a sufficient rate to be analysed independently. The LTVA outcome aims to approximate SCD more closely but also has the limitations of including fatal events while missing slower events with a deadly potential if untreated. In addition to differential rates of ICD implantation, ICD programming data, which was not collected systematically, may also differ regionally, contributing to the possibility of surveillance bias. However, given that LTVA (defined by a rate of 250 b.p.m. and thus captured with any ICD settings) and VA events in patients unprotected by ICDs demonstrated similar regional trends as sustained VA, we do not expect that differences in ICD settings contributed substantially to our results. We cannot exclude that the absence of statistically significant differences in the arrhythmic event rates between North Americans and Europeans in the low- and intermediate-risk groups could be the result of an inability to detect differences of small magnitude given the lower event rates in these risk groups.
Complications of ICD implantation, whether at time of implantation or during follow-up, were not collected systematically as part of this study. However, ICD-associated complications in ARVC patients have been well described in the literature.2,31,32
Conclusion
In this unprecedently large ARVC cohort, North American ARVC patients received more primary prevention ICDs than their European counterparts across all risk strata. North Americans demonstrated higher rates of sustained VA, LTVA, and VA events occurring in patients without ICDs, but there were no differences in the rates of these outcomes in low- and intermediate-risk patients. Ventricular arrhythmia event rates in patients with ICDs were the same in North American and European patients. Thus, lower rates of ICD implantation in Europeans did not translate to apparent harm. Females received ICD implantation at only a slightly decreased rate despite a markedly lower risk for sustained VA events, suggesting that male sex is an under-recognized risk factor for VA. In the future, implementing individualized ICD decision-making based on quantitative predictions of baseline VA risk may offer improved rates of appropriate primary prevention ICD utilization.
Supplementary Material
Acknowledgements
We are grateful to the ARVC patients and families who have made this work possible.
Contributor Information
Richard T Carrick, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Corrado De Marco, Cardiovascular Genetics Centre, Montreal Heart Institute, Université de Montréal, 5000 rue Bélanger, Montréal, Québec H1T 1C8, Canada.
Alessio Gasperetti, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA; Division of Heart and Lungs, Department of Cardiology, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands.
Laurens P Bosman, Division of Heart and Lungs, Department of Cardiology, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands; Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart).
Jean-Baptiste Gourraud, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Department of Cardiology, Centre Hospitalier Universitaire Nantes, Nantes, France.
Alessandro Trancuccio, Molecular Cardiology, Istituti Clinici Scientifici Maugeri (IRCCS), Pavia, Italy.
Andrea Mazzanti, Molecular Cardiology, Istituti Clinici Scientifici Maugeri (IRCCS), Pavia, Italy.
Brittney Murray, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Catherine Pendleton, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Crystal Tichnell, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Harikrishna Tandri, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA; Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
Katja Zeppenfeld, Department of Cardiology, Leiden University Medical Center, Leiden, The Netherlands.
Arthur A M Wilde, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Amsterdam UMC, Heart Center Department of Cardiology, Amsterdam Cardiovascular Sciences, Heart Failure and Arrhythmias, University of Amsterdam, Amsterdam, The Netherlands.
Brianna Davies, Center for Cardiac Innovation, Division of Cardiology, University of British Columbia, Vancouver, British Columbia, Canada.
Colette Seifer, St.Boniface Hospital, University of Manitoba, Winnipeg, Manitoba, Canada.
Jason D Roberts, Hamilton Health Sciences, Population Health Research Institute, McMaster University, Hamilton, Ontario, Canada; Section of Cardiac Electrophysiology, Division of Cardiology, Department of Medicine, Western University, London, Ontario, Canada.
Jeff S Healey, Hamilton Health Sciences, Population Health Research Institute, McMaster University, Hamilton, Ontario, Canada.
Ciorsti MacIntyre, Queen Elizabeth II Health Sciences Centre, Dalhousie University, Halifax, Nova Scotia, Canada; Department of Medicine, Mayo Clinic, Rochester, Minnesota, USA.
Wael Alqarawi, Department of Cardiac Sciences, College of Medicine, King Saudi University, Riyadh, Saudi Arabia; Division of Cardiology, University of Ottawa Heart Institute, University of Ottawa, Ottawa, Canada.
Rafik Tadros, Cardiovascular Genetics Centre, Montreal Heart Institute, Université de Montréal, 5000 rue Bélanger, Montréal, Québec H1T 1C8, Canada.
Michael J Cutler, Intermountain Medical Center, Intermountain Medical Center Heart Institute, Murray, UT, USA.
Mattia Targetti, Cardiomyopathy Unit, Careggi Hospital and Meyer Children’s Hospital IRCCS, Florence, Italy.
Leonardo Calò, Division of Cardiology, Policlinico Casilino, Rome, Italy.
Francesco Vitali, Cardiology Unit, Sant’Anna University Hospital, University of Ferrara, Ferrara, Italy.
Matteo Bertini, Cardiology Unit, Sant’Anna University Hospital, University of Ferrara, Ferrara, Italy.
Paolo Compagnucci, Cardiology and Arrhythmology Clinic, University Hospital Ospedali Riuniti, Ancona, Italy.
Michela Casella, Cardiology and Arrhythmology Clinic, University Hospital Ospedali Riuniti, Ancona, Italy.
Antonio Dello Russo, Cardiology and Arrhythmology Clinic, University Hospital Ospedali Riuniti, Ancona, Italy.
Chiara Cappelletto, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Division of Cardiology, Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina and University of Trieste, Trieste, Italy; Division of Cardiology, Department of Medicine, Karolinska Institutet, Solna, Stockholm, Sweden.
Antonio De Luca, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Division of Cardiology, Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina and University of Trieste, Trieste, Italy.
Davide Stolfo, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Division of Cardiology, Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina and University of Trieste, Trieste, Italy; Division of Cardiology, Department of Medicine, Karolinska Institutet, Solna, Stockholm, Sweden.
Firat Duru, Department of Cardiology, University Heart Center Zurich, Zurich, Switzerland.
Henrik K Jensen, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Department of Cardiology, Aarhus University Hospital, Aarhus N, Denmark; Department of Clinical Medicine, Health, Aarhus University, Aarhus N, Denmark.
Anneli Svensson, Department of Cardiology, Linköping University Hospital, Linköping, Sweden; Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden.
Pia Dahlberg, Department of Cardiology, Sahlgrenska University Hospital, Gothenburg, Sweden.
Nina E Hasselberg, ProCardio Center for Innovation, Department of Cardiology, Oslo University Hospital, Rikshospitalet, University of Oslo, Oslo, Norway.
Andrea Di Marco, Arrhythmia Unit, Department ofCardiology, Hospital Universitari de Bellvitge, L'Hospitalet de Llobregat, Barcelona, Spain; BioHeartCardiovascular Diseases Research Group, Bellvitge Biomedical Research Institute (IDIBELL), L'Hospitalet de Llobregat, Barcelona, Spain.
Paloma Jordà, Cardiovascular Genetics Centre, Montreal Heart Institute, Université de Montréal, 5000 rue Bélanger, Montréal, Québec H1T 1C8, Canada; Arrhythmia Section, Department of Cardiology, Hospital Clínic, Universitat de Barcelona, Barcelona, Spain.
Elena Arbelo, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Arrhythmia Section, Department of Cardiology, Hospital Clínic, Universitat de Barcelona, Barcelona, Spain; Institut d'Investigació August Pi i Sunyer (IDIBAPS), Barcelona, Spain; Centro de Investigación Biomédica en Red de Enfermedades Cardiovasculares (CIBERCV), Madrid, Spain.
Zoraida Moreno Weidmann, Arrhythmia Unit, Department of Cardiology, Hospital Universitari Sant Pau, Barcelona, Spain.
Karolina Borowiec, Department of Congenital Heart Diseases, Cardinal Wyszynski National Institute of Cardiology, Warsaw, Poland; Outpatient Department of Genetic Arrhythmias, Cardinal Wyszynski National Institute of Cardiology, Warsaw, Poland.
Antoine Delinière, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Department of Cardiology, National Reference Center for Inherited Arrhythmias of Lyon, Louis Pradel Cardiovascular Hospital, Hospices Civils de Lyon, Lyon, France; University of Lyon, Claude Bernard Lyon 1 University, MeLiS, CNRS UMR 5284, INSERM U1314, Institut NeuroMyoGène, Lyon, France.
Elżbieta K Biernacka, Department of Congenital Heart Diseases, Cardinal Wyszynski National Institute of Cardiology, Warsaw, Poland; Outpatient Department of Genetic Arrhythmias, Cardinal Wyszynski National Institute of Cardiology, Warsaw, Poland.
J Peter van Tintelen, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Department of Genetics, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands.
Pyotr G Platonov, Department of Cardiology, Clinical Sciences, Lund University, Lund, Sweden.
Iacopo Olivotto, Cardiomyopathy Unit, Careggi Hospital and Meyer Children’s Hospital IRCCS, Florence, Italy.
Ardan M Saguner, Department of Cardiology, University Heart Center Zurich, Zurich, Switzerland.
Kristina H Haugaa, ProCardio Center for Innovation, Department of Cardiology, Oslo University Hospital, Rikshospitalet, University of Oslo, Oslo, Norway.
Moniek Cox, Department of Cardiology, University Medical Center Groningen, Groningen, The Netherlands.
Claudio Tondo, Department of Clinical Electrophysiology and Cardiac Pacing, Centro Cardiologico Monzino, IRCCS, University of Milan, Milan, Italy; Department of Biomedical, Surgical and Dental Sciences, University of Milan, Milan, Italy.
Marco Merlo, Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart); Division of Cardiology, Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina and University of Trieste, Trieste, Italy.
Andrew D Krahn, Center for Cardiac Innovation, Division of Cardiology, University of British Columbia, Vancouver, British Columbia, Canada.
Anneline S J M te Riele, Division of Heart and Lungs, Department of Cardiology, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands; Member of the European Reference Network for Rare, Low Prevalence and Complex Diseases of the Heart (ERN GUARD-Heart).
Katherine C Wu, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Hugh Calkins, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Cynthia A James, Heart and Vascular Institute, Johns Hopkins University, Baltimore, MD, USA.
Julia Cadrin-Tourigny, Cardiovascular Genetics Centre, Montreal Heart Institute, Université de Montréal, 5000 rue Bélanger, Montréal, Québec H1T 1C8, Canada.
Supplementary data
Supplementary data are available at European Heart Journal online.
Declarations
Disclosure of Interest
A.G.: consulting fees from Lexeo. J.S.H.: grants and honoraria from Boston Scientific and Medtronic and on DSMB for the PRAETORIAN trial (Boston Scientific). J.D.R.: consulting fees from Lexeo and Ionis Pharmaceuticals. M.J.C.: consulting fees or advisory boards for Janssen, Boston Scientific, and Biosense Webster. C.C.: honoraria from AstraZeneca and Novo Nordisk E.A.: consulting fees/honoraria from Biosense Webster. A.S.J.M.t.R.: honoraria from Springer Healthcare. H.K.J.: grants from the Novo Nordisk Foundation NNF18OC0031258 and NNF20OC0065151 and honoraria from Amgen, Abbott, and Biosense Webster. A.S.: honoraria from Abbott. M.B.: honoraria from Boston, Daiichi, Behringer, Biotronik, MicroPort, Abbott, Medtronic, Bayer, and Pfizer. Z.M.W.: honoraria from Abbott and expert testimony for Boston Scientific. P.G.P.: consulting fees, honoraria, or advisory board from PSI Inc., Pfizer, and Tenaya. I.O.: consulting fees and advisory board from BMS, Cytogenetics, Amicus, Genzyme, Takeda, Chiesi, Rocket Pharma, Lexeo, and Tenaya. A.M.S.: grants through institution from Abbott, Bayer Healthcare, Biosense Webster, Biotronik, Boston Scientific, BMS/Pfizer, and Medtronic; speaker/advisory board/consulting fees from Bayer Healthcare, Biotronik, Daiichi-Sankyo, Medtronic, Novartis, Pfizer, and StrideBio; and stocks from Gilead. K.H.H.: honoraria from Pfizer and Novartis. Cl.T.: honoraria from Medtronic, Abbott, and Boston Scientific. M.M.: grant from Pfizer (amyloidosis) and honoraria from Pfizer, Novartis, Vifor Pharma, AstraZeneca, and Novo Nordisk. H.C. is a consultant for Medtronic Inc., Biosense Webster, Pfizer, StrideBio, Abbott, and Tenaya. H.C. receives research support from Boston Scientific; Cr. T. and C.A.J. receive salary support from this grant. C.A.J. receives research support from Lexeo, Inc. Cr. T. and A.G. receive salary support from this grant. C.A.J. is a consultant for Pfizer, Lexeo, and StrideBio. J.C.-T.: consulting fees from Tenaya, Lexeo, BMS/Pfizer, and Bayer.
Data Availability
To maintain patient confidentiality, data and study materials have not been made publicly available, but a limited data set may be made available upon request.
Funding
The Johns Hopkins ARVD/C Program is supported by the Leonie-Wild Foundation; the Leyla Erkan Family Fund for ARVD Research; the Hugh Calkins, Marvin H. Weiner, and Jacqueline J. Bernstein Cardiac Arrhythmia Center; the Dr Francis P. Chiaramonte Private Foundation; the Dr Satish, Rupal, and Robin Shah ARVD Fund at Johns Hopkins; the Bogle Foundation; the Campanella Family; the Patrick J. Harrison Family; the Peter French Memorial Foundation; and the Wilmerding Endowments. R.T.C. is funded by an NIH T32 grant (T32HL007227) and the NIH Loan Repayment Program (L30HL165535). J.C.-T. is supported by the Philippa and Marvin Carsley Cardiology Research Chair and the Montreal Heart Institute Foundation and receives salary support as a research scholar of the FRQS. K.H.H. is funded by the Norwegian Research Council, ProCardio #309762, GENE POSITIVE #288438, and EMPATHY #298736. A.S.J.M.t.R. receives funding from ZonMW Off Road personal research grant and Dutch Heart Association Dr Dekker Stipend. J.P.v.T. is supported by the Netherlands Cardiovascular Research Initiative, supported by the Dutch Heart Foundation 2018–30 PREDICT2. The Netherlands Arrhythmogenic Cardiomyopathy (ACM) Registry is supported by the Netherlands Heart Institute (project 06901). The Zurich ARVC Program (F.D. and A.M.S.) is supported by grants from the Georg and Bertha Schwyzer-Winiker Foundation, Baugarten Foundation, Swiss National Science Foundation, Swiss Heart Foundation, and USZ Foundation (Dr Wild Grant). P.J. received support by the Daniel Bravo Foundation and Spanish Society of Cardiology (Magda Heras mobility grant). The Hospital Clínic cohort (P.J. and E.A.) was funded by Sociedad Española de Cardiología. P.G.P. is supported by the Swedish Heart Lung and ALF foundations.
Ethical Approval
This study conformed to the Declaration of Helsinki and was approved by local ethics and/or institutional review boards.
Pre-registered Clinical Trial Number
None supplied.
References
- 1.Corrado D, Link MS, Calkins H. Arrhythmogenic right ventricular cardiomyopathy. N Engl J Med 2017;376:61–72. 10.1056/NEJMra1509267 [DOI] [PubMed] [Google Scholar]
- 2.Olde Nordkamp LR, Postema PG, Knops RE, van Dijk N, Limpens J, Wilde AA, et al. . Implantable cardioverter-defibrillator harm in young patients with inherited arrhythmia syndromes: a systematic review and meta-analysis of inappropriate shocks and complications. Heart Rhythm 2016;13:443–54. 10.1016/j.hrthm.2015.09.010 [DOI] [PubMed] [Google Scholar]
- 3.Corrado D, Wichter T, Link MS, Hauer RN, Marchlinski FE, Anastasakis A, et al. . Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an international task force consensus statement. Circulation 2015;132:441–53. 10.1161/CIRCULATIONAHA.115.017944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corrado D, Calkins H, Link MS, Leoni L, Favale S, Bevilacqua M, et al. . Prophylactic implantable defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia and no prior ventricular fibrillation or sustained ventricular tachycardia. Circulation 2010;122:1144–52. 10.1161/CIRCULATIONAHA.109.913871 [DOI] [PubMed] [Google Scholar]
- 5.Bhonsale A, James CA, Tichnell C, Murray B, Gagarin D, Philips B, et al. . Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol 2011;58:1485–96. 10.1016/j.jacc.2011.06.043 [DOI] [PubMed] [Google Scholar]
- 6.Bosman LP, Sammani A, James CA, Cadrin-Tourigny J, Calkins H, van Tintelen JP, et al. . Predicting arrhythmic risk in arrhythmogenic right ventricular cardiomyopathy: a systematic review and meta-analysis. Heart Rhythm 2018;15:1097–107. 10.1016/j.hrthm.2018.01.031 [DOI] [PubMed] [Google Scholar]
- 7.Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. . 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2018;138:e272–391. 10.1161/CIR.0000000000000549 [DOI] [PubMed] [Google Scholar]
- 8.Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA, et al. . 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J 2022;43:3997–4126. 10.1093/eurheartj/ehac262 [DOI] [PubMed] [Google Scholar]
- 9.Cadrin-Tourigny J, Bosman LP, Nozza A, Wang W, Tadros R, Bhonsale A, et al. . A new prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy. Eur Heart J 2019;40:1850–8. 10.1093/eurheartj/ehz103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jordà P, Bosman LP, Gasperetti A, Mazzanti A, Gourraud JB, Davies B, et al. . Arrhythmic risk prediction in arrhythmogenic right ventricular cardiomyopathy: external validation of the arrhythmogenic right ventricular cardiomyopathy risk calculator. Eur Heart J 2022;43:3041–52. 10.1093/eurheartj/ehac289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Casella M, Gasperetti A, Gaetano F, Busana M, Sommariva E, Catto V, et al. . Long-term follow-up analysis of a highly characterized arrhythmogenic cardiomyopathy cohort with classical and non-classical phenotypes-a real-world assessment of a novel prediction model: does the subtype really matter. Europace 2020;22:797–805. 10.1093/europace/euz352 [DOI] [PubMed] [Google Scholar]
- 12.Nauffal V, Marstrand P, Han L, Parikh VN, Helms AS, Ingles J, et al. . Worldwide differences in primary prevention implantable cardioverter defibrillator utilization and outcomes in hypertrophic cardiomyopathy. Eur Heart J 2021;42:3932–44. 10.1093/eurheartj/ehab598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. . Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation 2010;121:1533–41. 10.1161/CIRCULATIONAHA.108.840827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. . Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015;17:405–24. 10.1038/gim.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seidl K, Senges J. Worldwide utilization of implantable cardioverter/defibrillators now and in the future. Card Electrophysiol Rev 2003;7:5–13. 10.1023/A:1023603118860 [DOI] [PubMed] [Google Scholar]
- 16.John Camm A, Nisam S. European utilization of the implantable defibrillator: has 10 years changed the ‘enigma’? Europace 2010;12:1063–9. 10.1093/europace/euq282 [DOI] [PubMed] [Google Scholar]
- 17.Schrage B, Uijl A, Benson L, Westermann D, Ståhlberg M, Stolfo D, et al. . Association between use of primary-prevention implantable cardioverter-defibrillators and mortality in patients with heart failure: a prospective propensity score-matched analysis from the Swedish Heart Failure Registry. Circulation 2019;140:1530–9. 10.1161/CIRCULATIONAHA.119.043012 [DOI] [PubMed] [Google Scholar]
- 18.Scherr S, Reifegerste D, Arendt F, van Weert JCM, Alden DL. Family involvement in medical decision making in Europe and the United States: a replication and extension in five countries. Soc Sci Med 2022;301:114932. 10.1016/j.socscimed.2022.114932 [DOI] [PubMed] [Google Scholar]
- 19.Gasperetti A, Carrick RT, Costa S, Compagnucci P, Bosman LP, Chivulescu M, et al. . Programmed ventricular stimulation as an additional primary prevention risk stratification tool in arrhythmogenic right ventricular cardiomyopathy: a multinational study. Circulation 2022;146:1434–43. 10.1161/CIRCULATIONAHA.122.060866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calkins H, Corrado D, Marcus F. Risk stratification in arrhythmogenic right ventricular cardiomyopathy. Circulation 2017;136:2068–82. 10.1161/CIRCULATIONAHA.117.030792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cerrone M, Noorman M, Lin X, Chkourko H, Liang FX, van der Nagel R, et al. . Sodium current deficit and arrhythmogenesis in a murine model of plakophilin-2 haploinsufficiency. Cardiovasc Res 2012;95:460–8. 10.1093/cvr/cvs218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cadrin-Tourigny J, Bosman LP, Wang W, Tadros R, Bhonsale A, Bourfiss M, et al. . Sudden cardiac death prediction in arrhythmogenic right ventricular cardiomyopathy: a multinational collaboration. Circ Arrhythm Electrophysiol 2021;14:e008509. 10.1161/CIRCEP.120.008509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grondin S, Davies B, Cadrin-Tourigny J, Steinberg C, Cheung CC, Jorda P, et al. . Importance of genetic testing in unexplained cardiac arrest. Eur Heart J 2022;43:3071–81. 10.1093/eurheartj/ehac145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carrick RT, Te Riele ASJM, Gasperetti A, Bosman L, Muller SA, Pendleton C, et al. . Longitudinal prediction of ventricular arrhythmic risk in patients with arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol 2022;15:e011207. 10.1161/CIRCEP.122.011207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gasperetti A, Cappelletto C, Carrick R, Targetti M, Tichnell C, Martino A, et al. . Association of premature ventricular contraction burden on serial holter monitoring with arrhythmic risk in patients with arrhythmogenic right ventricular cardiomyopathy. JAMA Cardiol 2022;7:378–85. 10.1001/jamacardio.2021.6016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akdis D, Saguner AM, Shah K, Wei C, Medeiros-Domingo A, von Eckardstein A, et al. . Sex hormones affect outcome in arrhythmogenic right ventricular cardiomyopathy/dysplasia: from a stem cell derived cardiomyocyte-based model to clinical biomarkers of disease outcome. Eur Heart J 2017;38:1498–508. 10.1093/eurheartj/ehx011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao M, Woodward M, Vaartjes I, Millett ERC, Klipstein-Grobusch K, Hyun K, et al. . Sex differences in cardiovascular medication prescription in primary care: a systematic review and meta-analysis. J Am Heart Assoc 2020;9:e014742. 10.1161/JAHA.119.014742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nanna MG, Wang TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, et al. . Sex differences in the use of statins in community practice. Circ Cardiovasc Qual Outcomes 2019;12:e005562. 10.1161/CIRCOUTCOMES.118.005562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bozkurt B, Khalaf S. Heart failure in women. Methodist Debakey Cardiovasc J 2017;13:216–23. 10.14797/mdcj-13-4-216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curtis LH, Al-Khatib SM, Shea AM, Hammill BG, Hernandez AF, Schulman KA. Sex differences in the use of implantable cardioverter-defibrillators for primary and secondary prevention of sudden cardiac death. JAMA 2007;298:1517–24. 10.1001/jama.298.13.1517 [DOI] [PubMed] [Google Scholar]
- 31.Christensen AH, Platonov PG, Svensson A, Jensen HK, Rootwelt-Norberg C, Dahlberg P, et al. . Complications of implantable cardioverter-defibrillator treatment in arrhythmogenic right ventricular cardiomyopathy. Europace 2022;24:306–12. 10.1093/europace/euab112 [DOI] [PubMed] [Google Scholar]
- 32.Wang W, Gasperetti A, Sears SF, Tichnell C, Murray B, Tandri H, et al. . Subcutaneous and transvenous defibrillators in arrhythmogenic right ventricular cardiomyopathy: a comparison of clinical and quality-of-life outcomes. JACC Clin Electrophysiol 2023;9:394–402. 10.1016/j.jacep.2022.09.020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
To maintain patient confidentiality, data and study materials have not been made publicly available, but a limited data set may be made available upon request.