Abstract
Background
T cell immunodeficiency is a common feature in cancer patients, which may relate to initiation and development of tumor. Our previous study showed skewed expression of T cell receptor beta variable region (TRBV) subfamilies and clonal expansion of T cells in leukemia patients. In the present study, in order to further characterize the T cell immunity in acute myeloid leukemia (AML) patients, the level of recent thymic emigrants (RTE) was analyzed.
Materials and methods
Quantitative analysis of signal joint T cell recombination excision circles (δRec-ψJα sjTRECs) was performed in peripheral blood mononuclear cells (PBMCs) by real-time PCR (TaqMan), and the analysis of 23 TRBV-BD1 sjTRECs was performed by semi-nested PCR. Eighty-eight cases with AML were selected for this study; ten AML cases in complete remission (AML-CR) and 38 healthy individuals served as controls.
Results
The levels of δRec-ψJα sjTRECs in PBMCs and CD3+ T cells were significantly decreased in AML patients, compared with healthy individuals and in patients in completive remission. Also the frequency of 23 TRBV-BD1 sjTRECs, and the number of detectable TRBV subfamily sjTRECs were significantly lower in AML patients than in healthy individuals. Moreover, the sjTRECs numbers and the frequency of TRBV-BD1 sjTRECs showed a progressive linear decline with age in AML patients.
Conclusions
The decreased numbers of universal (δRec-ψJα) and family-specific (TRBV-BD1) sjTRECs indicate that the severe T cell immunodeficiency in AML patients is associated with reduced levels of recent thymic emigrants. In patients achieving complete remission both sjTREC counts return to normal values indicating the recovery of thymic function. Better understanding of the mechanisms underlying persistent immunodeficiency in leukemia patients may lead to novel treatment strategies to enhance immune competence.
Keywords: T cells, δRec-ψJα sjTRECs, TRBV-BD sjTRECs, AML
Introduction
Acute myeloid leukemia (AML) is the most common acute leukemia affecting adults, and its incidence is expected to further increase as the population ages. Despite recent scientific advances in understanding the molecular biology of AML, the survival rates in AML, with an exemption of acute promyelocytic leukemia, did not improve substantially over the last 30 years and are still below 30% [1, 2]. T cell immunodeficiency was suggested to play an important role in cancer patients, promoting the expansion of the malignant clone [3, 4]. Several studies on T cell receptor beta variable region (TRBV) repertoire showed that skewed expression of TRBV subfamilies is a common feature in patients with leukemia [5]. However, little is known about the proliferative history of T cells in these patients [6].
T cell differentiation in the thymus is characterized by a hierarchical order of rearrangement steps in the T cell receptor (TCR) genes, resulting in the joining of variable (V), diversity (D) and joining (J) gene segments. During each of the rearrangement steps, DNA fragments between rearranging gene segments are deleted as circular signal joint T cell receptor excision circles (sjTRECs). The TCR delta gene (TRD) is located within the TRA gene segments along chromosome 14q11 (TRAD locus). During the process of TCR alpha-delta locus (TRAD) rearrangements the TCR delta gene (TRD), which is located within the TCR alpha (TRA) gene, has to be deleted before the TRA recombination starts. Two so-called TRD deleting elements, δRec and ψJα, that flank the major part of the TRD gene were identified [7–11]. Recombination between δRec and ψJα produces δRec-ψJα signal joint TRECs, which are assumed to have high over-time stability, but cannot multiply and consequently are diluted during T cell proliferation. A maximum of two sjTRECs can be present within one αβ T cell if the corresponding rearrangement event occurs in both alleles and if the cell did not divide upon the rearrangement. sjTRECs are exported from thymus to the periphery within recent thymic emigrants (RTEs); therefore, the frequency of sjTRECs is considered to be the most accurate marker of T cell neogenesis. Although it was reported that the TRD locus could be excised through other recombination events that will not generate sjTRECs, more than 70% of the TRD deletion though δRec-ψJα rearrangement. Since 1998, quantitative detection of sjTRECs was used for direct measurement of the proliferative history of T cells [8]. In addition, expansion of particular TRBV family T cells can be determined by quantitative analysis of series of TRBV-BD sjTRECs [12, 13]. The first report on TRECs analysis in hematopoietic malignancy was published by Petridou and colleagues [14], who compared the sjTREC values in patients with childhood B-ALL and T-ALL. There was highly significant reduction of sjTREC values in children with T cell malignancies, whereas children with B cell origin ALL had slightly, but nonsignificantly lower sjTRECs values compared to healthy children. In another study, Haining et al. [15] reported that consistent with the reduction in naïve T cells, thymopoiesis (measured by sjTRECs levels) was significantly lower in 73 children with ALL than in normal controls. The first description of analysis of the sjTRECs-content in patients with AML was reported in ASH meeting from our previous study [16].
The main objective of our study was to investigate the proliferative history of normal T cells in AML patients by quantitative analysis of total sjTRECs and TRBV subfamily sjTRECs.
Design and methods
Samples
Eighty-eight newly diagnosed, untreated AML cases were included in the study (51 males and 37 females, median age: 42.5 years, range 4–77), classified according to the French–American–British (FAB) criteria as M0: 15 cases, M1: 6 cases, M2: 23 cases (AML1-ETO-M2: 12 cases, AML1-ETO+M2: 11 cases), M3: 11 cases, M4: 8 cases, M5: 21 cases and M6: 4 cases. In 70 AML cases peripheral blood mononuclear cells (PBMCs) were analyzed and in 18 cases purified CD3+ T cells were used for TREC quantification. Ten AML cases in complete remission (AML-CR) (10 males, median age 45.5 years, range 17–61) and 38 healthy individuals (17 males and 21 females, median age: 32 years, range 17–66) served as controls. The percentage of blast cells in PB samples from AML ranged 0–93%, the median number was 60.75%.
Mononuclear cell isolation
PBMCs were isolated from AML and healthy individuals by Ficoll-Hypaque gradient centrifugation.
CD3+ cell determination
The PLP-fixed cytospin preparations were incubated with 200 μg/ml of murine anti-CD3 mAb (Boster Biological Technology Ltd, Wuhan, China), washed and incubated with 1:50 dilution of fluorescein labeled goat anti-mouse Ig (Boster Biological Technology Ltd, Wuhan, China). The slides were counterstained with Mayer’s hematoxylin for 30 min. All slides were blindly evaluated with the fluorescent microscope (Nikon WFX-II, Nikon Ltd, Japan); 200 cells were counted.
CD3+T cells sorting
The CD3+ T cells from PBMCs from 18 AML cases and 10 healthy individuals were sorted using CD3 MoAb (Miltenyi Biotec, Germany) and MACS® Magnetic Cell sorting technique.
DNA extraction
Total DNA from distinct cell populations was extracted using QIAamp® DNA Blood Mini Kit (QIAGEN, Germany); the quality of RNA was analyzed in 0.8% agarose gel stained with ethidium bromide and the concentration was determined by spectrophotometric analysis at 260 and 280 nm (Lambda 45 UV/VIS Spectrometer, Perkin Elmer USA).
Real-time quantitative PCR (RQ-PCR)
Quantitative detection of δRec-ψJα sjTRECs in DNA from PBMCs was performed by real-time PCR using the ABI PRISM 7700 Sequence Detector TaqMan (PE Biosystems, Foster City, CA). The primers and probes were purchased from TIB MOLBIOL GmbH, Berlin, Germany and the RQ-PCR was performed as described previously [16, 17]. In brief, PCR of 25 μl total volume was performed with approximately 100 ng of genomic DNA, 25 pmol of each primers (TREC-1 and TREC-2 for sjTRECs, RAG2-for and RAG2-back for RGA2 amplification), 10 nmol each dNTP (Perkin Elmer), 1.5 U AmpliTaq Gold (Perkin Elmer), 5 pmol of 6FAM-TAMRA probe, and PCR Buffer including 4.5 mM MgCl2. After the initial denaturation at 95°C for 5′, 45 cycles consisting of 95°C 30″ and 67°C 1′ were performed [17, 18].
Semi-nest PCR
Twenty-three TRBV-BD1 sjTRECs were amplified by semi-nest PCR using different amounts of genomic DNA: 0.325 μg or 0.065 μg corresponding to 5 × 104 or 1 × 104cells, respectively. Two nested 5′ TRBD1 primers, located upstream of the segment, and 23 BV primers (BV1-19 and BV21-24; the rearrangement of BV20 does not generate a sjTRECs due to its reverse orientation) were used [18]. In the first round PCR, aliquots of the DNA (2 μl) were amplified in 10 μl reactions with one of the 23 BV primers (antisense) and a BD1 primer (out sense primer); the final reaction mixture contained 0.375 μM sense primer and antisense primer, 0.1 mM dNTP, 1.5 mM MgCl2, 1× PCR buffer, and 1U Taq polymerase (Promega, USA). The amplification was performed on a DNA thermal cycler (BioMetra, Germany). After 3 min denaturation at 94°C, 30 PCR cycles were performed, each cycle consisting of 94° for 1.5 min, 65°C for 1 min and 72°C for 1 min, and a final 6 min elongation at 72°C. Then, the products were stored at 4°C. In the second round PCR, aliquots of the first PCR products (2 μl) were subjected to semi-nested PCR reaction with the same BV primer and the inner sense BD1 primer. The final 10 μl reaction system contained 0.375 μM sense and antisense primers, 1.5 mM MgCl2, 0.1 mM dNTP, 1U Taq polymerase and PCR buffer (Promega, USA). After a 3-min denaturation at 94°C, 25 cycles of amplification were carried out (1 min at 94°C, 2 min at 72°C and a final 6-min elongation at 72°C).
DNA sequencing
PCR products from each TRBV-BD1 sjTRECs were direct sequenced to confirm the formation of BV-BD1 sjTRECs. The sequencing was done according to the direction by using BigDye® Terminator v3.1 Cycle Sequencing kit and ABI PRISM 3100-Avant Genetic Analyzer.
Statistical analysis
Univariate analyses were done using the Mann–Whitney test to compare manes of δRec-ψJα sjTRECs or number of detectable subfamily of TRBV-BD1 sjTRECs between AML and healthy control groups. The Fisher exact test was used to compare the frequency of TRBV-BD1 sjTRECs in PBMCs between AML and healthy control groups. Pearson correlation and linear regression analysis were used to estimate the correlation between age and sjTRECs numbers, or the blast cell percentage and sjTRECs number.
Results
The δRec-ψJα sjTRECs level in PBMCs and CD3+ T cells from AML patients
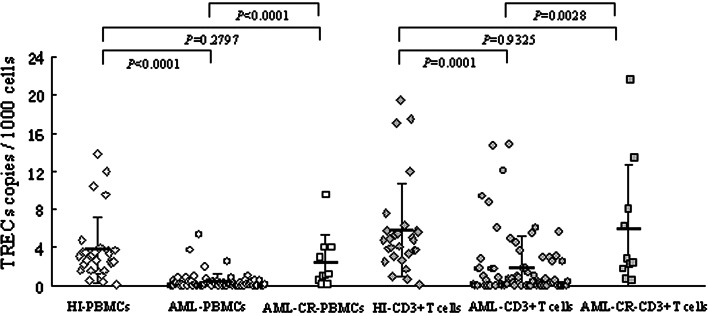
The absolute numbers of sjTRECs and RAG2 were measured in two independent assays and each 1,000 PBMCs carrying sjTRECs was calculated using a formula n = 2×1,000 × [TREC(1) + TREC(2)]/[RAG2(1) + RAG2(2)]. The sjTRECs values in T cells were determined by normalization with the percentage of CD3-positive cells in the analyzed sample; n = (TRECs/1,000 PBMCs)/(CD3+%). The sjTRECs levels in PBMCs and CD3 + T cells from patients with AML were 0.38 ± 0.86 copies/1,000 PBMCs and 1.93 ± 3.29 copies/1,000 CD3+ cells, respectively (Fig. 1). In comparison with the sjTRECs in healthy individuals (3.78 ± 3.45 copies/1,000 PBMCs, 5.79 ± 4.87 copies/1,000 CD3+ cells), a dramatic reduction of sjTRECs values in patients with AML was found (p < 0.0001 and p < 0.0001, respectively). The TREC counts decrease logarithmically during the 50 years of adult life span (20–70 years) about tenfold [8]. Since on average the AML patients were 11 years older than healthy individuals, the TREC counts in AML patients were normalized—multiplied by the factor of 10E + (11/50) = 1.67. Even when age adjusted the TREC levels in AML (0.63 copies/1,000 PBMCs and 3.22 copies/1,000 CD3+ cells) were significantly lower than in healthy control. The sjTRECs number in AML-CR group was 2.44 ± 1.84 copies/1,000 PBMCs and 5.96 ± 6.79 copies/1,000 CD3+ cells, which was significantly increased, compared with the AML group (p < 0.0001 and p = 0.0028, respectively), and did not significantly differ from the healthy individuals group (p = 0.2523 and p = 0.9325, respectively) (Fig. 1). In three cases the pre-treatment and the CR sample were taken from the same patients. After a successful treatment the sjTREC counts increased in all three patients, in PBMCs and in CD3+ cells, directly confirming the recovery of naïve T cells in patients upon achieving a complete remission (Table 1).
Fig. 1.
The sjTRECs number in PBMCs and CD3 + T cells from AML, AML in complete remission (AML-CR) and healthy individuals (HI). The groups which were compared are indicated by arrows and the p value is given
Table 1.
sjTREC counts in AML patients before treatment and in complete remission
| Patients | Sex | Age | Diagnosis | TRECs/1,000 PBMC | TRECs/1,000 CD3+ cells |
|---|---|---|---|---|---|
| XCZ | M | 50 | M2-pre treatment | 0.001 | 0.009 |
| M2-CR | 0.164 | 0.534 | |||
| LHR | M | 52 | M3-pre treatment | 0.017 | 0.095 |
| M3-CR | 0.185 | 0.632 | |||
| JDY | M | 32 | M4-pre treatment | 0.305 | 1.906 |
| M4-CR | 1.225 | 2.374 |
The numbers of sjTRECs in PBMCs and CD3+ T cells from different AML subtypes were analyzed. In comparison with healthy group, sjTRECs number from the most AML subtype groups were significantly decreased, except M3-CD3+ T cell and both M6-PBMCs and CD3 + T cells groups; the latter may be due to limited number of samples in the group.
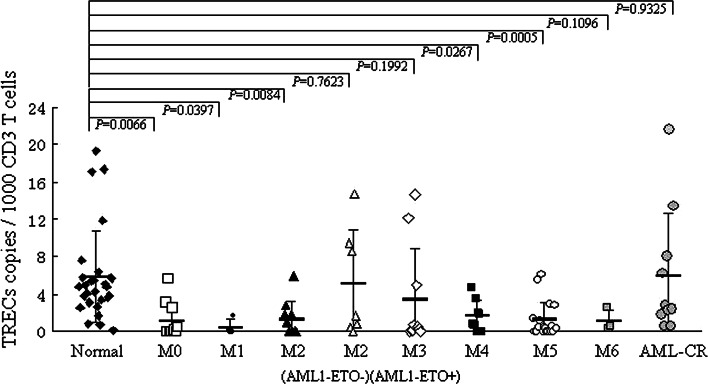
Interestingly, AML cases with good prognosis: 10/10 M3 cases with t(15:17) expressing the PML-RARA fusion, and 7/17 M2 cases with t(8:21) expressing the AML1-ETO fusion, showed the highest sjTREC counts among the AML patients, which did not differ from the healthy individuals. In contrast, AML1-ETO negative M2 was significantly decreased; however, 7/17 M2 cases with t(8:21) expressing the AML1-ETO fusion which is thought to be good prognosis, showed no significant difference in sjTRECs number (Fig. 2).
Fig. 2.
The sjTRECs number in CD3 + T cells from different FAB subtypes of AML, AML in complete remission (AML-CR) and healthy individuals (HI). Each AML group was compared with the healthy individuals
Similar results were found in comparison with AML-CR groups; both M0-PBMCs (p = 0.0123) and CD3 + T cells (p = 0.0221) groups, both AML1-ETO-M2-PBMCs (p = 0.0129) and CD3 + T cells (p = 0.0250) groups, M4-PBMCs group (p = 0.0283), both M5-PBMCs (p = 0.0016) and CD3 + T cells (p = 0.0028) groups were significantly decreased (Fig. 2). No significant correlation was found between the blast cell percentage and the sjTRECs numbers in CD3 + T cells using the Pearson’s correlation and linear regression analysis (r = −0.142534, p = 0.239167).
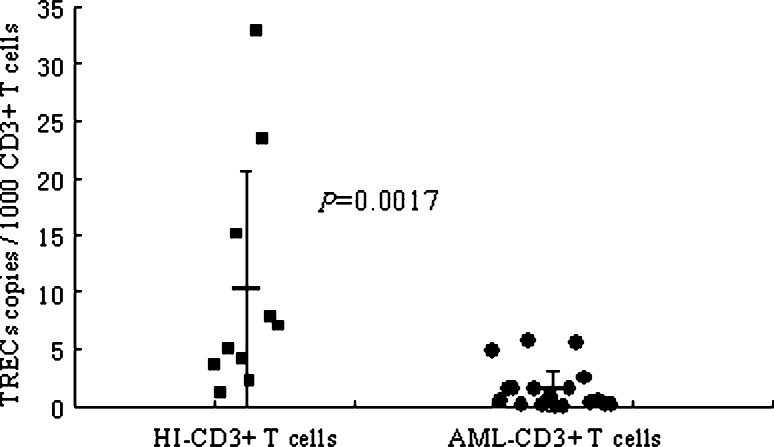
To further confirm the result of absolute lower sjTRECs level in CD3 + T cells from AML, CD3 + T cells were sorted from PBMCs from AML patients and healthy individuals. The number of sjTRECs in sorted CD3 + T cells from AML (1.53 ± 1.89/1,000 cells) was again significantly lower than that from healthy individuals (10.26 ± 10.41/1,000 cells, p = 0.0017) (Fig. 3).
Fig. 3.
The sjTREC numbers in purified CD3 + T cells from AML and healthy individuals (HI)
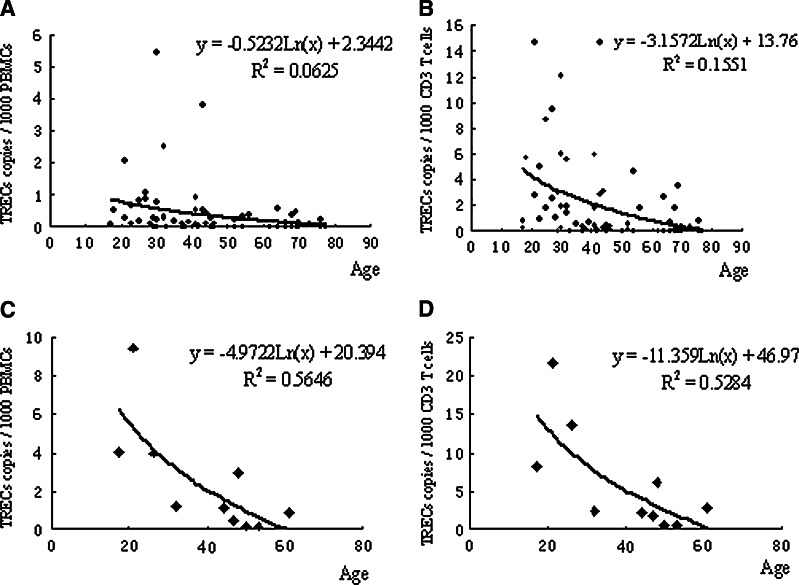
In the present study, females, in both healthy control (4.36 ± 3.92 copies/1,000 PBMCs or 6.57 ± 5.53 copies/1,000 CD3 + cells) and AML groups (0.47 ± 1.02 copies/1,000 PBMCs or 2.67 ± 3.95 copies/1,000 CD3 + cells), had slightly but nonsignificantly higher sjTRECs values compared to males (3.11 ± 2.82 copies/1,000 PBMCs or 4.88 ± 4.00 copies/1,000 CD3 + cells in healthy controls, 0.32 ± 0.72 copies/1,000 PBMCs or 1.35 ± 2.57 copies/1,000 CD3 + cells in AML) (p > 0.05). The sjTRECs numbers showed a progressive linear decline with age in AML patients (AML-PBMCs: r = −0.266, p = 0.027, y = −0.5232Ln(x) + 2.3442, R 2 = 0.0625; AML-CD3 + T cells: r = −0.388, p = 0.01, y = −3.1572Ln(x) + 13.76, R 2 = 0.1551; AML-CR-PBMCs: r = −0.771, p = 0.025, y = −4.9722Ln(x) + 20.394, R 2 = 0.5646; and AML-CR-CD3 + T cells: r = −0.767, p = 0.026, y = −11.359Ln(x) + 46.97, R 2 = 0.5284) (Fig. 4); however, this was not statistically significant in healthy individuals in PBMCs (r = −0.219, p = 0.253) and in CD3 + T cells (r = −0.232, p = 0.227).
Fig. 4.
TREC numbers in AML patients from the age of 17–77 years. The TREC counts show a progressive logarithmic decline with age. a AML-PMBCs group, b AML-CD3 + T cells group, c AML-CR-PBMCs group, d AML-CR-CD3 + T cells group
Comparison of TRECs levels in different age groups, <40 years and ≥40 years, revealed significantly lower TREC count in the ≥40 years group (n = 40, 0.16 ± 0.21 copies/1,000 PBMCs, 0.78 ± 1.40 copies/1,000 CD3 + cells) than in the <40 years group of AML (n = 30, 0.69 ± 1.24 copies/1,000 PBMCs, 3.39 ± 4.40 copies/1,000 CD3 + cells) (p = 0.0089, p = 0.0008, respectively). However, the reduction of TRECs numbers was not significantly age-associated in healthy controls (p = 0.3563 in PBMCs, p = 0.3289 in CD3+ T cells).
The frequencies of 23 TRBV-BD1 sjTRECs in PBMCs from AML patients
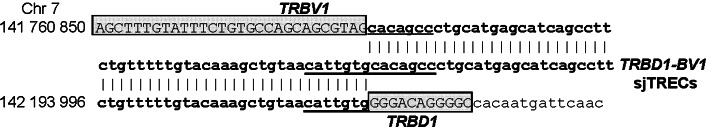
The TRBV-D1 sjTRECs from TRBV1-19 and TRBV21-24 were analyzed by semi-nested PCR, using different amounts of DNA (corresponding to 5 × 104 or 1 × 104 cells, respectively). The sequences of the junction regions of each TRBV-D1 sjTRECs were confirmed by direct sequencing of PCR products; some of the sequences are shown in Fig. 5.
Fig. 5.
Nucleotide sequence of junction regions of TRBD1-BV1-sjTRECs compared with the germline sequence of the TRAD locus. The TRBD1 and TRBV1 segments are indicated by boxes, heptamer motifs of the recombination signal sequences (RSS) are underlined
Thirty-nine AML cases and ten healthy individuals were used to analyze the frequencies of 23 TRBV-BD1 sjTRECs in PBMCs. The number of detectable TRBV subfamily sjTRECs differed significantly in AML (13.70 ± 2.67/5 × 104 PBMCs and 5.50 ± 2.07/1 × 104 PBMCs) and healthy individuals (4.46 ± 3.15/5 × 104 PBMCs and 2.26 ± 1.97/1 × 104 PBMCs) (p < 0.0001, p < 0.0001). sjTRECs TRBV subfamilies could be detected in healthy groups; however, only sjTRECs TRBV subfamilies could be found in both AML groups The number of detectable TRBV subfamily sjTRECs in different AML subtypes ranged from 3.40 ± 3.05 to 5.82 ± 3.87/5 × 104 PBMCs and 1.20 ± 0.84 to 3.33 ± 3.21/1 × 104 PBMCs, except the AML-M1 (1 × 104) group (p = 0.168); all of them were significantly decreased in AML subtypes when compared with healthy controls (13.70 ± 2.67/5 × 104 PBMCs and 5.50 ± 2.07/1 × 104 PBMCs) (p < 0.01 or p < 0.05). But the difference was not significant within FAB subtype AML patients.
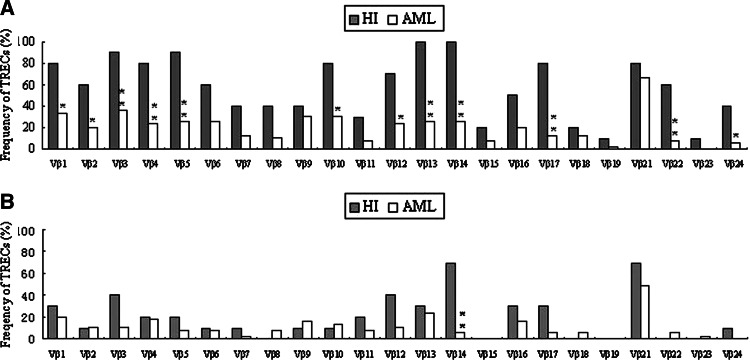
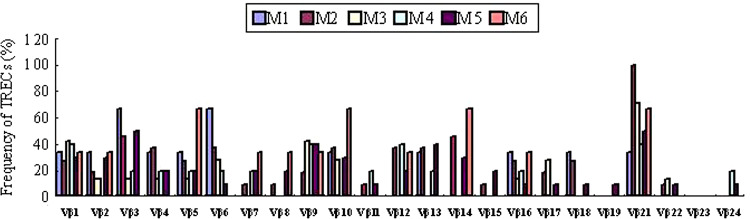
Comparison of the frequencies of 23 TRBV-BD1 sjTRECs in PBMCs between AML patients and healthy controls at 5 × 104 PBMCs level showed that the frequencies of the most TRBV subfamily sjTRECs were significantly lower than those from healthy individuals (Fig. 6). But no significant difference could be found when the frequency of TRBV subfamily sjTRECs in 1 × 104 PBMCs between both groups were compared, except for BV14-BD1 sjTRECs, which was more frequent in healthy PBMCs (70%) than in AML samples (5.13%) (p = 0.0001). The frequency of TRBV-BD1 sjTRECs in PBMCs from different AML subtype was showed in Fig. 7. TRBV21-BD1 sjTRECs were the most frequent TRECs in M2 (11/11 cases, 100%) and M3 (5/7 cases, 71.43%) subtype. TRBV23-BD1 sjTRECs could be detected in none of all AML cases. Similar results were found in TRBV19-BD1 sjTRECs, which could be detected in only one case with M5 subtype, and TRBV24-BD1 sjTRECs, which could be detected only in one case with M4 and one case with M5 subtypes.
Fig. 6.
The frequency of TRBV-BD1 sjTRECs in PBMCs from AML and control groups. Note: * p < 0.05, compared to healthy control, ** p < 0.01, compared to healthy control. a DNA amount corresponding to 5 × 104 PBMCs/per reaction, b amount corresponding to 1 × 104 PBMCs/per reaction
Fig. 7.
The frequency of TRBV-BD1 sjTRECs in PBMCs from different AML subtypes. DNA amount corresponding to 5 × 104 PBMCs was used per reaction
Comparison of TRBV-BD1 sjTRECs subfamily numbers in different genders showed no statistically significant difference between female (4.38 ± 3.88 subfamiles/5 × 104 PBMCs, 2.00 ± 2.08 subfamilies/104 PBMCs) and male (4.81 ± 2.98 subfamilies/5 × 104 PBMCs, 2.77 ± 2.44 subfamilies/104 PBMCs) groups of AML patients (p = 0.7032, p = 0.3368).
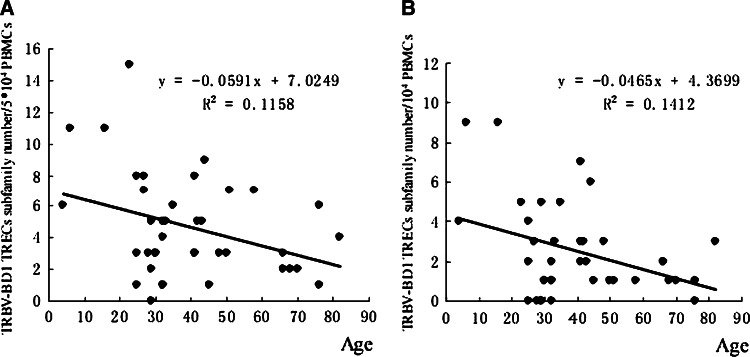
The numbers of TRBV-BD1 sjTRECs subfamily showed age-associated decline in AML patients, when analyzed 5 × 104 PBMCs (r = −0.3402, p = 0.0341, y = −0.0591x + 7.0249, R 2 = 0.1158) or 104 PBMCs (r = −0.3757, p = 0.0184, y = −0.0465x + 4.3699, R 2 = 0.1412) (Fig. 8); however, there was no significant age-associated decline in both 5 × 104 PBMCs or 104 PBMCs group of healthy individuals (r = −0.5913, p = 0.0718 in 5 × 104 PBMCs and r = −0.1020, p = 0.7793 in 104 PBMCs group), which may be due to the limited number of samples (n = 10).
Fig. 8.
The numbers of TRBV-BD1 sjTREC subfamilies in AML patients from the age of 4–76 years. The number of TRBV-BD1 sjTREC subfamilies shows age-associated decline. a DNA amount corresponding to 5 × 104 PBMCs was analyzed, b DNA amount corresponding to 104 PBMCs was analyzed
Comparison of TRBV-BD1 sjTRECs in younger and older AML patients revealed lower, but not statistically significant, TRBV-BD1 sjTRECs subfamily numbers in ≥40 years group (n = 18; 4.11 ± 2.42 subfamilies/5 × 104 PBMCs, 2.22 ± 1.80 subfamilies/104 PBMCs) than in <40 years group (n = 21; 5.14 ± 3.84 subfamilies/5 × 104 PBMCs, p = 0.3324 and 2.76 ± 2.72 subfamilies/104 PBMCs, p = 0.4775).
Discussion
Poor cellular immune function may relate to carcinogenic processes and to worse prognosis in solid tumor patients as well as in leukemia [3, 4]. Previous research showed that skewed expression of TRBV subfamilies is a common feature in patients with leukemia [19–21]. Clonally expanded T cells could be identified in some TRBV subfamilies, which display specific anti-leukemia cytotoxicity, indicating that specific anti-leukemic T cells could be generated in vivo [5, 19]. This suggests that the host could have the ability of specific immune response to leukemia-associated antigens, despite T cell immunodeficiency.
In the present study, in order to further evaluate the potential T cell immune function, the proliferative history in AML patients was analyzed. The sjTRECs-content in PBMCs and CD3 + T cells from AML patients was determined. We showed a dramatic reduction of sjTREC values in total AML patients as well as in different subtypes of AML. In some cases no sjTREC copies could be detected in 40,000 T cells. This indicates either poor thymic output or extensive T cell proliferation and apoptosis, or most likely combination of all these factors in AML patients. This effect seems to be even more pronounced than in patients with ALL [14]. Increased sjTRECs numbers in the AML-CR samples show that thymic function may recover in AML patients in complete remission phase. To date there are only two publications describing TREC level in hematopoietic malignancies; both in pediatric ALL [14, 15]. Our study is the first to provide data on TRECs values in adult AML. We clearly show a prominent reduction of sjTREC levels in this malignancy; but whether this is due to clonal expansion of T cells to antigens, for example, leukemia-associated antigens, or reflects impairment of immune function associated to the malignancy, remains an open question [5, 9, 16, 20–23].
The majority of published studies focus only on the total number of recent thymic emigrants, as measured by quantitative analysis of δRec-ψJα sjTRECs. This approach does not allow for evaluation of the complexity of thymic output and T cell proliferation in different TRBV subfamilies, which is an important factor in the immune competence. In this study, we have successfully established a semi-nested PCR to analyze the total 23 subfamilies of TRBV-DB1 sjTRECs in normal T cells in AML patients. The results indicate that the percentage of cases positive for TRBV-DB1 sjTRECs varies in different TRBV subfamilies; the highest for TRBV2-5, V13-14 and V21. It corresponds to the percentage of cases expressing individual TRVB subfamily genes, as published previously [24]. The most important observation in this study was the significantly lower frequency of 23 TRBV-BD1 sjTRECs in PBMCs from AML patients than those from healthy individuals, indicating poor thymic output in AML patients. The results further support and explain the significant reduction of recent thymic emigrant numbers in peripheral blood of AML patients, as measured by quantitative detection of δRec-ψJα sjTRECs.
It was previously shown that due to age-associated thymus involution, the thymus output declines with age [8, 25]. In the present study, we report a similar age-associated decline in sjTRECs numbers in patients with de novo AML and in patients in clinical remission. In addition, we analyzed the relationship between the numbers of TRBV-BD1 subfamily sjTRECs and the age. We show that in parallel to the δRec-ψJα sjTRECs content decline, also the numbers of TRBV-BD1 sjTRECs decline with age in AML patients.
Pido-Lopez et al. [25] reported that slower δRec-ψJα sjTRECs decline after 40 years of age, but we did not observe this relation either in healthy individuals or in AML patients. Also the decline rate of the TRBV-BD1 sjTRECs did not differ significantly in <40 and ≥40 years old patients.
Moreover, Pido-Lopez et al. [25] showed that the decline in number of recent thymic emigrants in the blood with increasing age is gender-linked. Peripheral blood from females contained significantly higher levels of sjTRECs per CD3 + T cell than blood from males. Also in children, the number of sjTRECs was higher in healthy girls than in healthy boys, and a similar pattern was evident in T cell malignancies [14]. In the present study, we observed slightly, but nonsignificantly higher δRec-ψJα and TRBV-BD1 sjTRECs values in healthy females as well as in female AML patients. The lower sjTRECs level may relate to the poor prognosis; as Petridou et al. showed that during a median follow-up period of about 19 months, only four children died. All of them had a T cell hematopoietic malignancy and relatively low sjTRECs values. And it appears that there is a pattern of concordance of high sjTRECs values with better disease prognosis in hematological childhood malignancies. In the present study, AML cases with good prognosis for example, APL with PML-RARα fusion gene and M2 with AML1-ETO fusion gene, showed the highest sjTREC counts among the AML patients. These findings may be used as hypothesis-generating indications that should be confirmed in larger data sets. It is a matter of regret that we are unable to follow up the clinical outcome and the survival time of the AML patients, although we provide the analysis of the sjTRECs level in AML-CR patients, which showed a normal number of sjTRECs.
In conclusion, it is, to our knowledge, the first description of the T cell proliferative history in AML patients using both quantitative analysis of δRec-ψJα sjTRECs and frequency analysis of TRBV-DB1 subfamily specific sjTRECs. The study provides evidence for reduced numbers of recent thymic emigrants in AML patients, which recovers in patients achieving complete remission. This finding should be confirmed in a larger study including the analysis of the relationship between sjTREC numbers and prognosis in AML.
Acknowledgments
This project was sponsored by grants from National Natural Science Foundation of China (No. 30270579), Natural Science Foundation of Guangdong Province (No.23001) and the Department of Education of Guangdong Province (No. Q 02022). We thank Prof. Xin Du from Dept. of Hematology, Guangdong Provincial People’s Hospital for kindly providing AML samples.
Contributor Information
Yangqiu Li, Email: yangqiuli@hotmail.com.
Grzegorz K. Przybylski, Phone: +48-61-6579225, FAX: +48-61-8233235, Email: przybylg@man.poznan.pl
References
- 1.Deschler B, Lübbert M. Acute myeloid leukemia: epidemiology and etiology. Cancer. 2006;107:2099–2107. doi: 10.1002/cncr.22233. [DOI] [PubMed] [Google Scholar]
- 2.Erba HP. Prognostic factor in elderly patients with AML and the implications for treatment. Hematology Am Soc Hematol Educ Program. 2007;2007:420–428. doi: 10.1182/asheducation-2007.1.420. [DOI] [PubMed] [Google Scholar]
- 3.Hadden JW. Immunodeficiency and cancer: prospects for correction. Int Immunopharmacol. 2003;3:1061–1071. doi: 10.1016/S1567-5769(03)00060-2. [DOI] [PubMed] [Google Scholar]
- 4.Costello RT, Rey J, Fauriat C, Gastaut JA, Olive D. New approaches in the immunotherapy of haematological malignancies. Eur J Haematol. 2003;70:333–345. doi: 10.1034/j.1600-0609.2003.00065.x. [DOI] [PubMed] [Google Scholar]
- 5.Li Y, Chen S, Yang L, Zhou Y, Wu X, Huang M, Geng S. Clonal expanded TCR Vβ T cells in patients with APL. Hematology. 2005;10:135–139. doi: 10.1080/10245330400026196. [DOI] [PubMed] [Google Scholar]
- 6.Li Y. Recent thymic output function in patients with hematological malignancy. Hematology. 2005;10:297–305. doi: 10.1080/10245330500093591. [DOI] [PubMed] [Google Scholar]
- 7.De Villartay JP, Hockett R, Coran D, Korsmeyer SJ, Cohen DI. Deletion of the human T-cell receptor δ-gene by a site specific recombination. Nature. 1998;335:170–174. doi: 10.1038/335170a0. [DOI] [PubMed] [Google Scholar]
- 8.Douek DC, McFarland RD, Keiser PH, Gage EA, Massey JM, Haynes BF, Polis MA, Haase AT, Feinberg MB, Sullivan JL, Jamieson BD, Zack JA, Picker LJ, Koup RA. Changes in thymic function with age and during the treatment of HIV infection. Nature. 1998;396:690–695. doi: 10.1038/25374. [DOI] [PubMed] [Google Scholar]
- 9.Hazenberg MD, Verschuren MC, Hamann D, Miedema F, van Dongen JJ. T cell receptor excision circles as markers for recent thymic emigrants: basic aspects, technical approach, and guidelines for interpretation. J Mol Med. 2001;79:631–640. doi: 10.1007/s001090100271. [DOI] [PubMed] [Google Scholar]
- 10.Geenen V, Poulin JF, Dion ML, Martens H, Castermans E, Hansenne I, Moutschen M, Sekaly RP, Cheynier R. Quantification of T cell receptor rearrangement excision circles to estimate thymic function: an important new tool for endocrine-immune physiology. J Endocrinol. 2003;176:305–311. doi: 10.1677/joe.0.1760305. [DOI] [PubMed] [Google Scholar]
- 11.Al-Harthi L, Marchett G, Steffens CM, Poulin J, Sekaly R, Landay A. Detection of T cell receptor circles (TRECs) as biomarkers for de novo T cell synthesis using a quantitative polymerase chain reaction-enzyme linked immunosorbent assay (PCR-ELISA) J Immunol Methods. 2000;237:187–197. doi: 10.1016/S0022-1759(00)00136-8. [DOI] [PubMed] [Google Scholar]
- 12.Poulin JF, Viswanathan MN, Harris JM, Komanduri KV, Wieder E, Ringuette N, Jenkins M, McCune JM, Sékaly RP. Direct evidence for thymic function in adult humans. J Exp Med. 1999;190:479–486. doi: 10.1084/jem.190.4.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poulin JF, Sylvestre M, Champagne P, Dion ML, Kettaf N, Dumont A, Lainesse M, Fontaine P, Roy DC, Perreault C, Sékaly RP, Cheynier R. Evidence for adequate thymic function but impaired naive T-cell survival following allogeneic hematopoietic stem cell transplantation in the absence of chronic graft-versus-host disease. Blood. 2003;102:4600–4607. doi: 10.1182/blood-2003-05-1428. [DOI] [PubMed] [Google Scholar]
- 14.Petridou E, Klimentopoulou AE, Moustaki M, Kostrikis LG, Hatzakis A, Trichopoulos D. Recent thymic emigrants and prognosis in T- and B-cell childhood hematopoietic malignancies. Int J Cancer. 2002;101:74–77. doi: 10.1002/ijc.10568. [DOI] [PubMed] [Google Scholar]
- 15.Haining WN, Evans J, Seth N, Callaway G, Wucherpfennig K, Nadler L, Guinan E. Rapid T cell response to vaccination can occur without antibody response in children post HSCT. Blood. 2004;104(11):614a. [Google Scholar]
- 16.Li Y, Yang L, Chen S, Wang Z, Wu X, Przybylski GK, Schmidt CA. Recent thymic output function in patients with acute myelogenous leukemia. Blood. 2003;102(11):608a. [Google Scholar]
- 17.Kimmig S, Przybylski GK, Schmidt CA, Laurisch K, Mowes B, Radbruch A, Thiel A. Two subsets of naive T helper cells with distinct T cell receptor excision circle content in human adult peripheral blood. J Exp Med. 2002;195:789–794. doi: 10.1084/jem.20011756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y, Chen S, Yang L, Yin Q, Geng S, Wu X, Schmidt CA, Przybylski GK. TRAV and TRBV repertoire, clonality and the proliferative history of umbilical cord blood T cells. Transplant Immunol. 2007;18:151–158. doi: 10.1016/j.trim.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Li Y. Leukemia associated clonal expansion TCR Vβ subfamily T cells. Hematology. 2003;8:375–384. doi: 10.1080/10245330310001621288. [DOI] [PubMed] [Google Scholar]
- 20.Farace F, Orlanducci F, Dietrich PY, Gaudin C, Angevin E, Courtier MH, Bayle C, Hercend T, Triebel F. T cell repertoire in patients with B chronic lymphocytic leukemia evidence for multiple in vivo T cell clonal expansions. J Immunol. 1994;153:4281–4290. [PubMed] [Google Scholar]
- 21.Alatrakchi N, Farace F, Frau E, Carde P, Munck JN, Triebel F. T-cell clonal expansion in patients with B-cell lymphoproliferative disorders. J Immunother. 1998;21:363–370. doi: 10.1097/00002371-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Serrano D, Monteiro J, Allen SL, Kolitz J, Schulman P, Lichtman SM, Buchbinder A, Vinciguerra VP, Chiorazzi N, Gregersen PK. Clonal expansion within the CD4+CD57+ and CD8+CD57+T cell subsets in chronic lymphocytic leukemia. J Immunol. 1997;158:1482–1489. [PubMed] [Google Scholar]
- 23.Hazenberg MD, Borghans JAM, de Boer RJ, Miedema F. Thynic output: a bad TREC record. Nat Immunol. 2003;4:97–99. doi: 10.1038/ni0203-97. [DOI] [PubMed] [Google Scholar]
- 24.Yin QS, Li YQ, Chen SH, Yang LJ, Lu YH, Zhang XL. Detection of TCR Vbeta subfamily sjTRECs in normal peripheral blood and cord blood. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi (J Cell Mol Immunol) 2006;22:477–479. [PubMed] [Google Scholar]
- 25.Pido-Lopez J, Imami N, Aspinall R. Both age and gender affect thymic output: more recent thymic migrants in females than males as they age. Clin Exp Immunol. 2001;125:409–413. doi: 10.1046/j.1365-2249.2001.01640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]