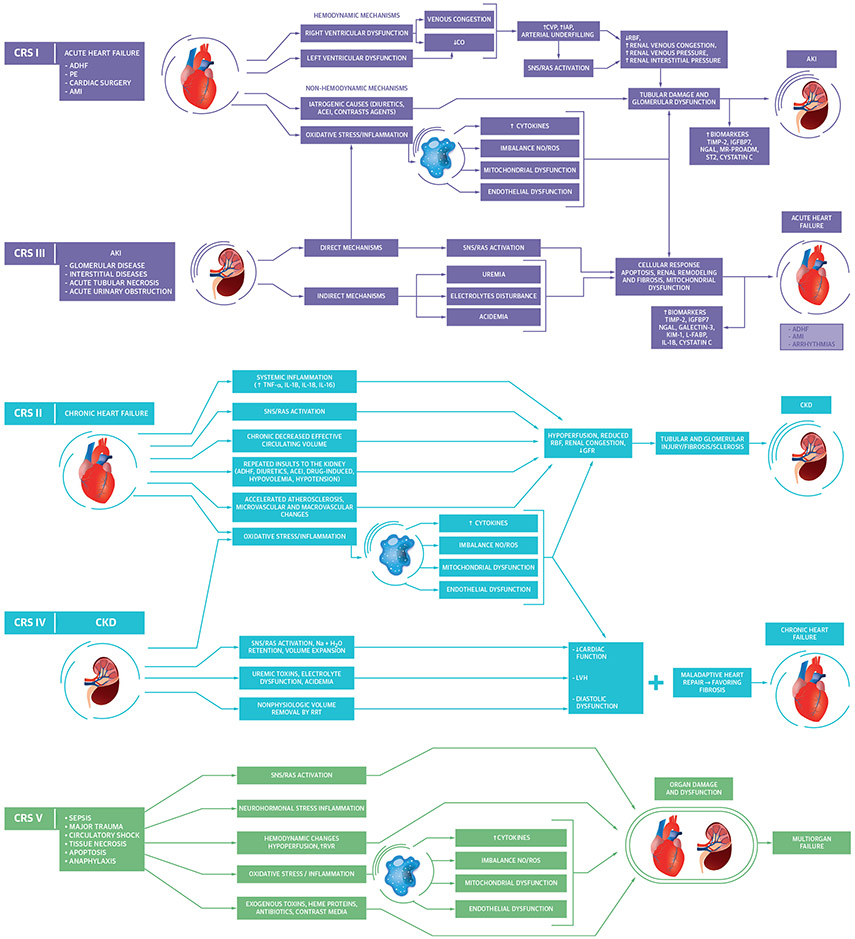
FIGURE 1. Pathophysiological Interactions Between the Heart and Kidney in CRS.
Acute cardiorenal syndrome (CRS) (types 1 and 3) occurs when acutely worsening heart or kidney function, respectively, leads to worsening function of the other organ. Chronic CRS (types 2 and 4) occurs when chronic heart or kidney dysfunction, respectively, leads to worsening dysfunction of the other organ. Secondary CRS (type 5) occurs when a systemic process leads to simultaneous heart and kidney dysfunction (28,34). ACEI = angiotensin-converting enzyme inhibitor; ADHF = acute decompensated heart failure; AKI = acute kidney injury; AMI = acute myocardial infarction; CKD = chronic kidney disease; CO = cardiac output, CVP = central venous pressure; GFR = glomerular filtration rate; H2O = water; IAP = intra-abdominal pressure; IGFBP7 = insulin-like growth factor binding protein 7; IL = interleukin; KIM-1 = kidney injury molecule 1; L-FABP = liver-type fatty acid binding protein; LVH = left ventricular hypertrophy; MR-PROADM = mid regional pro adrenomedullin; Na = sodium; N-GAL = neutrophil gelatinase-associated lipocalin; NO/ROS = nitric oxide/reactive oxygen species; PE = pulmonary embolism; RBF = renal blood flow; RRT = renal replacement therapy; RVR = renal venous resistance; SNS/RAS = sympathetic nervous system/renin angiotensin system; ST2 = suppression tumorigenicity 2; TIMP-2 = tissue inhibitor of metalloproteinase 2; TNF = tumor necrosis factor.