Abstract
The term hepatolithiasis describes the presence of biliary stones within the intrahepatic bile ducts, above the hilar confluence of the hepatic ducts. The disease is more prevalent in Asia, mainly owing to socioeconomic and dietary factors, as well as the prevalence of biliary parasites. In the last century, owing to migration, its global incidence has increased. The main pathophysiological mechanisms involve cholangitis, bile infection and biliary strictures, creating a self-sustaining cycle that perpetuates the disease, frequently characterised by recurrent episodes of bacterial infection referred to as syndrome of “recurrent pyogenic cholangitis”. Furthermore, long-standing hepatolithiasis is a known risk factor for development of intrahepatic cholangiocarcinoma. Various classifications have aimed at providing useful insight of clinically relevant aspects and guidance for treatment. The management of symptomatic patients and those with complications can be complex, and relies upon a multidisciplinary team of hepatologists, endoscopists, interventional radiologists and hepatobiliary surgeons, with the main goal being to offer relief from the clinical presentations and prevent the development of more serious complications. This comprehensive review provides insight on various aspects of hepatolithiasis, with a focus on epidemiology, new evidence on pathophysiology, most important clinical aspects, different classification systems and contemporary management.
Keywords: Cholelithiasis, Intrahepatic stones, Cholangiocarcinoma, Biliary parasites, Recurrent pyogenic cholangitis, Oriental cholangiohepatitis, Hepatectomy, Cholangioscopy, Liver transplant, Paediatric
Core Tip: Hepatolithiasis is a chronic disease, mostly prevalent in Asia, commonly characterised by recurrent episodes of cholangitis and relevant clinicopathological syndromes, while it constitutes a risk factor for development of intrahepatic cholangiocarcinoma. Its management in complex cases can be challenging and relies upon multidisciplinary input from hepatologists, endoscopists, interventional radiologists and hepatobiliary surgeons. This comprehensive review provides insight on various aspects of hepatolithiasis, with a main focus on the epidemiology, new evidence on pathophysiology, most important clinical aspects, different classification systems and contemporary management.
INTRODUCTION
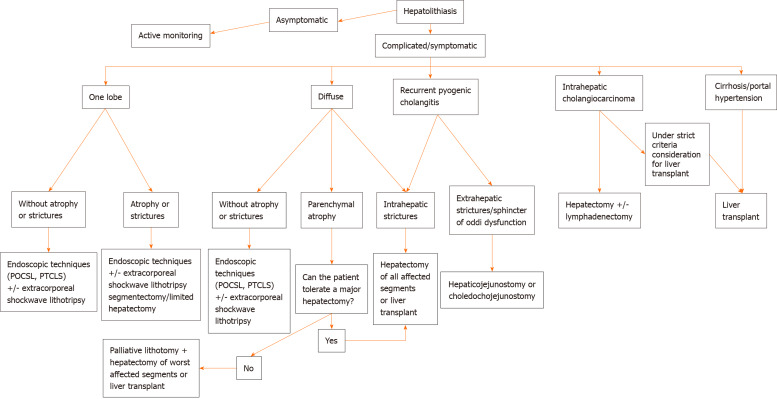
Cholelithiasis is the general term describing the presence of gallstones at any point along the biliary tree. Cholecystolithiasis is the precise term that describes the presence of gallstones within the gallbladder, even though in clinical practice, very often the terms cholelithiasis and gallstones are used for the same purpose, owing to the gallbladder being the predominant anatomical location of gallstones. The term choledocholithiasis refers to the presence of gallstones within the extrahepatic bile ducts, while hepatolithiasis describes the presence of gallstones within the intrahepatic bile ducts[1,2] (Figure 1).
Figure 1.
Topographic variations of cholelithiasis. The dashed line at the hilar ductal confluence delineates the level of differentiation between hepatolithiasis and choledocholithiasis.
More specifically, hepatolithiasis is characterised by the development of pigmented stones, mostly composed of calcium bilirubinate and less of cholesterol, in the intrahepatic bile ducts before their confluence into the common hepatic duct, irrespective of the coexistence of gallstones in the common bile duct (CBD) and/or gallbladder. The pathogenesis involves several mechanisms, including bile infection, cholestasis, hyperplasia of the biliary epithelium and bile duct strictures, all of which increase the risk of cholangiocarcinoma (CCA) in these patients[3,4]. In the case of primary hepatolithiasis, in the absence of extrahepatic biliary obstruction intrahepatic stones often cause chronic inflammation, mural fibrosis, and proliferation of peribiliary glands[5]. Frequently, hepatolithiasis is characterised by recurrent episodes of bacterial infections of the biliary system also referred to as “recurrent pyogenic cholangitis”[6]. The management of the disease currently relies on interventional procedures, to relieve cholestasis and extract impacted stones, as well as liver resection in cases of severe biliary strictures and hepatic parenchymal atrophy. This comprehensive review provides insight on various aspects of hepatolithiasis, with a focus on epidemiology, new evidence on the pathophysiology of the disease, most important clinical aspects, different classifications and contemporary management.
EPIDEMIOLOGY
The disease was described in Hong Kong in 1930[7], and is endemic to East and Southeast Asia, where its reported prevalence has been as high as 30%[8]. For these reasons, it has also been described as “oriental cholangiohepatitis”, “oriental cholangitis”, or “Hong Kong Disease”[9,10].
The incidence of hepatolithiasis varies greatly even within Asian countries, and Taiwan has the highest relative prevalence historically. Parasitic infections may play an important role in the development of hepatolithiasis[11]. In 1961, Fung[12] identified that among 262 patients treated with hepatolithiasis in Hong Kong, 30% also had liver fluke. More recently, economic development, improvements in the overall hygiene and introduction of a western diet richer in proteins and saturated fats, have led to a reduction in the incidence of the disease[13]. Nevertheless, a Taiwanese retrospective nationwide study in the early 90’s confirmed a high prevalence of hepatolithiasis among the 17182 patients included, with figures around 20%[14]. On the other hand, data available from Japan, showed a decrease in the incidence of hepatolithiasis in the past century, from 4.1% between 1970 and 1977 to 1.7% in 1995[10].
Glenn and Moody[15] reported in 1961 that patients of Asian descent living in the United States had a similar incidence of hepatolithiasis to the general American population, suggesting that the pathogenesis of the disease is mainly related to environmental, rather than genetic and ethnic factors. This also reinforces the theory that improved living standards and a change in the dietary habits play a major role in the decreased incidence.
Most systematic analyses of incidence and prevalence of hepatolithiasis come from Asia, although the disease is also prevalent among Latin Americans, and has been associated with lower socioeconomic status and rural environments[13,16]. A Brazilian group reported an incidence of 2.1% among patients referred to a tertiary centre for treatment of biliary stones[17].
In Western countries, the disease is rare and usually presents as secondary hepatolithiasis, i.e., associated with underlying conditions causing strictures on the bile ducts and/or stasis of the bile in the biliary tree, such as primary sclerosing cholangitis, malignancy, post-surgical complications, or choledochal cysts[16]. According to historical data, the prevalence of hepatolithiasis in the West is < 2%, although in the last century, migration has increased its global incidence overall[16]. A Swedish observational study on autopsies reported that among patients with gallstones, 1.9% had stones in the hepatic duct and 0.6% had intrahepatic stones[18]. The disease appears to be more frequent in women, and an age > 50 years has been reported as a risk factor[19].
PATHOPHYSIOLOGY AND RISK FACTORS
The pathophysiology of hepatolithiasis is complex and still uncertain. Cholestasis, biliary infection, abnormal bile duct anatomy, changes in bile metabolism, malnutrition and diet are factors that possibly drive and perpetuate the disease[3,20,21]. Patients with anatomical and functional changes in the biliary system have a higher risk of hepatolithiasis. Among these, congenital and/or acquired intrahepatic bile duct deformities (e.g., Caroli’s disease, primary sclerosing cholangitis, anastomotic stricture) are major risk factors. The presence of strictures creates non-linear trajectories of bile flow, thus facilitating the agglutination of crystals in the bile ducts and development of stones[22]. The left hepatic duct and the right posteroinferior bile duct are areas prone to the development of cholestasis when their angulation hinders the bile flow[23]. Moreover, a dysfunctional sphincter of Oddi has a negative effect on the homeostasis of the biliary tree. Once it has lost its one-way valve function, duodenal fluid can reflux into the ampulla of Vater and reach the CBD. This fluid will alter the biliary flora and cause inflammation on the bile ducts due to differences in the pH and the presence of pancreatic enzymes[22].
Studies have shown a possible association between bacterial translocation, bile infection and biliary stones[24,25]. Commensal microorganisms normally found in bile ducts are E. coli, S. typhimurium, B. cereus and L. monocytogenes[26]. Continuous bile flow, the sphincter of Oddi and the presence of immune cells in the biliary tree are natural mechanisms to keep these bacteria from triggering an infection. However, Xiao et al[27] observed that 40 Chinese patients with hepatolithiasis had a different bile flora when compared to the control group, with a larger population of Proteus and Streptomyces. Furthermore, microbiological studies observed that the diversity of bacteria in the biliary tract of patients with hepatolithiasis is smaller than the diversity in controls, thus suggesting an imbalance in the flora[27]. Biliary dysbiosis, specifically the increased presence of anaerobic bacteria, is related to changes in the bile homeostasis[28] leading to a higher risk of intrahepatic stones formation. Moreover, larger populations of lipopolysaccharide-producing bacteria trigger signalling pathways that lead to an increased production of mucin 5AC by cholangiocytes[29]. The higher concentration of mucin, in turn, promotes cholestasis and crystallisation of cholesterol[30,31]. In addition, bacteria produce beta-glucuronidase, or induce its production, leading to deposition of calcium bilirubinate and stone formation[22,32,33]. Finally, these microorganisms also produce phospholipases, responsible for breaking phosphatidylcholine into free fatty acids, consequently accelerating the deposition of fatty acid calcium and promoting further production of mucin by the cholangiocytes[27,34]. All of these mechanisms together create a self-sustaining cycle and promote stone formation.
Parasite infection, mainly by Ascaris, Clonorchis sinensis, Opisthorchis viverrini, and Schistosoma, is also associated with hepatolithiasis. These organisms usually live in the intestines but are known for invading the biliary tree. Once parasites pass the sphincter of Oddi and reach the bile ducts, they incite various mechanisms to fight helminths, such as increased intestinal epithelial cell turnover[35], and a switch from production of Mucin 2 to Mucin 5AC in the gut[36]. Moreover, parasites might cause mechanical obstruction of the bile drainage and promote further cholestasis. Finally, calcium bilirubinate crystals attach to helminth eggs, which represent an ideal substrate for formation of biliary stones[37].
Metabolomic analyses observed that patients with hepatolithiasis have different serum levels of lipids and lipid-like molecules from healthy controls[38]. This reinforces previous findings that a dysregulated lipid metabolism is directly involved with the development of intrahepatic biliary stones[29,39,40]. Furthermore, mutations in ABCB4 and ABCB11, genes associated with bile production and mucin secretion, also have a role in the development of intrahepatic stones[22,41]. Cystic fibrosis (CF) is a common genetic disease caused by approximately 2000 mutations in the CFTR gene, the most prevalent of which is ΔF508. Notably, patients with the disease have a high incidence of cholelithiasis of 15–30% as opposed to an age-matched population incidence of 5%. CF is one of the very few diseases, which cause hepatolithiasis in children. Patients with large duct disease in particular, develop strictures, cholangiectasis, hepatolithiasis and recurrent infections[42].
The amount of protein and fat in the diet directly influences secretion of bile. East Asian populations tend to adopt low protein and low-fat dietary patterns, thus negatively affecting bile excretion and favouring cholestasis[22]. Low-protein diets also cause reduction of beta-glucuronidase inhibitors in the bile. Once cholestasis, biliary infection, anatomical abnormalities, and bile metabolism changes are in place, they create a vicious cycle of biliary injury. Recurrent damage to the bile ducts leads to activation of myofibroblasts, periductal lamellar fibrosis and hyperplastic epithelium, thus creating biliary strictures[43]. The hepatic parenchyma adjacent to impacted stones is usually marked with different degrees of atrophy and fibrosis according to the level of inflammation in that area. If biliary obstructions are left untreated, the chronic cholestasis can lead to biliary cirrhosis although it is not a common finding[43].
CLINICAL FEATURES
Clinical presentation
The signs and symptoms of hepatolithiasis are associated with the degree of cholestasis and presence of biliary infection. Patients will often complain about abdominal discomfort, nausea and vomiting, but may also present with cholangitis and the classic Charcot’s triad of abdominal pain, fever and jaundice[44]. Complicated cases can present with Reynold’s pentad (e.g., abdominal pain, fever, jaundice, confusion and hypotension), suggesting organ dysfunction, which is a marker of poor prognosis[20]. On the other hand, some patients can be oligo- or asymptomatic and receive a diagnosis of hepatolithiasis as an incidental finding during investigations for different conditions or due to non-specific abdominal symptoms[20].
Changes in the physical examination will depend on the underlying activity of cholangitis and biliary obstruction. Usual findings are epigastric discomfort on palpation and hepatomegaly[44].
Complications
Complex hepatolithiasis: One of the most common complications is the development of complex hepatolithiasis, when the disease affects both lobes and/or intrahepatic stones are associated with hilar stenosis/distortion[45]. If left untreated, biliary stenosis will lead to upstream chronic cholestasis, predispose the sedimentation of bile salts and formation of stones[22]. The treatment of hepatolithiasis, therefore, must involve the resolution of any bile duct strictures and promote normal bile flow.
Persistent cholangitis: Laxity of the sphincter of Oddi and biliary strictures increase the risk of infections in the biliary tree. The presence of bacteria also favours precipitation of bile salts and formation of stones[22], leading to a self-sustaining cycle of cholangitis, hyperplasia of the biliary epithelium, subsequent strictures, and further stone formation[43]. The biliary flora dysbiosis associated with a substrate that favours proliferation of pathogenic bacteria facilitates the recurrence of cholangitis, thus explaining why this disease is also called “recurrent pyogenic cholangitis”.
Biliary cirrhosis: Up to 14.1% of patients develop secondary biliary cirrhosis[3,46,47] and its complications, including portal hypertension and liver failure. Cirrhosis occurs as a consequence of the chronic inflammatory injury to the bile ducts, where the recurrent biliary sepsis may lead to periductal inflammation, fibrosis and portal thrombophlebitis[46]. The treatment includes management of the complications (ascites, portal hypertensive bleedings, hepatic encephalopathy, etc.) and, in the more advanced cases, orthotopic liver transplantation (OLT)[48,49].
CCA: Hepatolithiasis is a risk factor for intrahepatic CCA, which occurs in up to 21.2% of cases[3,50-52]. Intrahepatic CCA is an aggressive cancer with poor prognosis, particularly as complete surgical resection is only possible in less than a third of patients[53]. Patients with hepatolithiasis that develop intrahepatic CCA have higher levels of c-erbB2, epidermal growth factor, COX-2 and nuclear factor-kB, which are biomarkers of chronic inflammation[54-56]. Furthermore, tumour suppressor genes, namely p16 and DPC4/Smand4, are commonly inactivated in these patients, thus reinforcing the role of chronic inflammation in carcinogenesis, as seen in patients with primary sclerosing cholangitis.
The Japanese Hepatolithiasis Research Group followed 401 patients with hepatolithiasis for 18 years. This cohort had a 2.0% cumulative incidence of CCA at 5 years, 4.0% at 10 years and 6.2% at 15 years of follow-up[51]. Among these patients, independent risk factors for intrahepatic CCA were age ≥ 63 years (HR 3.334, 95%CI: 1.316-8.499), residual stones after treatment (HR 2.445, 95%CI: 1.047-5.711) and the occurrence/formation of biliary stricture during follow-up, (HR 4.350, 95%CI: 1.821-10.391). The incidence of CCA was higher in patients with three risk factors than in those with one or two risk factors[51]. Moreover, a Chinese retrospective study of 981 patients who underwent hepatectomy for hepatolithiasis, identified 55 cases with intrahepatic CCA over a median follow-up of 65 months. The authors reported that residual stones (HR 2.101, 95%CI: 1.150–3.839), formation of hepaticojejunostomy (HR 1.837, 95%CI: 1.077-3.133), and uniformity between extension of liver resection and stone-affected segments (i.e., whether all of the affected segments or less were resected) (HR 2.442, 95%CI: 1.205-4.948) are also independent factors for intrahepatic CCA[57]. In addition, a case-control study from China reported that smoking (OR = 1.931, 95%CI: 1.000-3.731), family history of cancer (OR= 5.175, 95%CI: 1.216-22.022) and symptoms for more than 10 years (OR= 2.348, 95%CI: 1.394-3.952) were independent risk factors for development of CCA in patients with hepatolithiasis[52].
Paediatric population
Data on aspects of hepatolithiasis in the paediatric population are extremely limited, particularly as primary hepatolithiasis is very rare in children. Yue[58] in 1974 was the first to publish a case series of 6 children with recurrent pyogenic cholangitis, treated between 1952 and 1972 at a single centre in Hong Kong, China, “with the main object of introducing this disease entity”. Four were males and 2 were females, with ages ranging from 7-14 years. In all cases soft pigment stones were found while in one case non-viable Ascaris lumbricoides was also detected. All patients received emergency surgical exploration, and 2 patients required re-operation. All patients were alive at a follow-up of 3-19 years. The author highlighted that the treatment of this entity in children is based on experience with adult patients[58].
Saing et al[59] in 1988 published their experience with 10 children treated with “recurrent pyogenic cholangitis”, at their hospital in Hong Kong, China, between 1973 and 1984. The presentation was uniformly acute with cholangitis, including features of septicaemia. Initial management included intravenous fluids and electrolytes, antibiotics against aerobic and anaerobic intestinal bacteria, and nasogastric suction, in all cases. While 4 of the 10 children responded well to conservative treatment, 3 of them subsequently required elective transduodenal sphincteroplasty. The remaining 6 patients required emergency surgery owing to poor response to conservative management after 24-48 h, and/or progression to septic shock. One patient required re-exploration. One death occurred following emergency sphincteroplasty owing to septicaemia, pulmonary complications, and pericardial effusion. At exploration, pigment stones and/or mud were found in the bile ducts in all cases. On two occasions Ascaris lumbricoides was found in the CBD. During follow-up over 3-12 years, the children remained well and continued to grow satisfactorily. Three patients required re-admissions for mild abdominal pain, which resolved with conservative measures[59].
As mentioned earlier, hepatolithiasis in childhood may also develop in patients with CF, particularly those with large duct disease[42].
A single-centre Spanish case-series from 1992 reported 7 paediatric patients with intrahepatic stones between 1981-1989, and retrospectively evaluated their radiological features. There were 6 female and 1 male patient in this cohort with a mean age of 3.6 years. Underlying causes were present, including CF in one case, immunodeficiency syndrome in a further case, 4 cases of extrahepatic biliary atresia treated with portoenterostomies, and a case following partial liver transplantation[60]. Of note, a recent retrospective study of 301 paediatric patients who underwent living donor liver transplantation over a 20-year period at a single centre in Japan, reported development of biliary strictures in 18%. During endoscopic treatment 23 patients (7%) were found to have developed hepatolithiasis and were managed with endoscopic techniques. However, a high recurrence rate of 30% was observed[61].
Recently, a Chinese single-centre retrospective cohort study of 106 children with a discharge diagnosis of “lithiasis”, hospitalized between 2010-2021, that were diagnosed with primary hepatolithiasis, reported male preponderance, mean age at diagnosis of 9.3 ± 3.6 years, and a preferential involvement of the right liver lobe (75.5%). The estimated incidence of primary hepatolithiasis in children was approximately 1.7 per 10000 hospitalized patients. All patients were asymptomatic and had hepatolithiasis discovered randomly on abdominal ultrasound during their treatment of other diseases; however, 6 patients had undergone previous choledochal cyst excision. More than 25% of patients diagnosed with primary hepatolithiasis had elevated γ-GGT. The authors noted that most of the underlying diseases that resulted in hospitalisation required treatment with antibiotics or hormones, suggesting that the formation of intrahepatic stones in children might be related to the use of these drugs; however, the pathogenesis of hepatolithiasis in this age group remains to be clarified. All patients were managed conservatively under observation. During follow-up of approximately 8 years, none of the patients developed severe clinical symptoms or complications and no patient required surgical intervention in childhood[62].
INVESTIGATIONS
Laboratory tests are not very informative for hepatolithiasis apart from showing the levels of systemic inflammation, cholestasis and biliary/hepatic injury.
Imaging studies, however, are paramount to identify the location of stones, complications and determine the best treatment. Ultrasound and magnetic resonance cholangiopancreatography (MRCP) are the preferred methods because both can detect non-calcified stones. While ultrasound is usually the first investigation, MRCP offers a more accurate evaluation of the biliary tree and is better at detecting biliary strictures and dilations[10,63,64]. Non-calcified stones cannot be identified on computerised tomography, but the method is useful to locate abscesses and biliary dilations[10].
Biomarkers are not particularly useful for the diagnosis of hepatolithiasis. Recently, Wang et al[38] identified four metabolites, namely 18-β-Glycyrrhetinic acid, FMH, Rifampicin and PC (4:0/16:2), that are over-expressed in hepatolithiasis and had a good efficacy to discriminate patients with hepatolithiasis from healthy controls. However, the study only included 30 Chinese patients, thus these biomarkers need validation in larger and more heterogeneous populations before they are used in clinical practice.
CLASSIFICATION
Throughout the years, many classifications have been developed to distinguish between cases of hepatolithiasis. One of the most used is Dong’s classification, that proposes a treatment approach depending on the location of intrahepatic stones, hepatic atrophy, biliary changes, presence of extrahepatic stones and sphincter of Oddi function[65]. Both Nakayama’s classification and the Tsunoda classification focus on describing the disease based on location of stones, presence and location of biliary stricture and dilation[66,67]. Finally, the recently proposed LHO system[68] divides patients according to their capacity to tolerate an anatomical hepatectomy, the presence of hilar strictures and changes at the sphincter of Oddi. A summary of the criteria in each of these classifications are presented in Table 1.
Table 1.
Main classifications of hepatolithiasis and criteria accounted for
|
Classification
|
Criteria
|
Advises on treatment
|
| Dong’s classification[65] | Location of stones | Yes |
| Presence of hepatic atrophy | ||
| Presence of biliary strictures | ||
| Cirrhosis | ||
| Function of the sphincter of Oddi | ||
| Nakayama’s classification[66] | Type of stones | No, entirely descriptive |
| Location of stones | ||
| Presence of biliary stenosis, severity, and location | ||
| Presence of biliary dilation, severity, and location | ||
| Presence of stones inside the gallbladder | ||
| Function of the sphincter of Oddi | ||
| Previous operations | ||
| Tsunoda classification[67] | Primary or secondary lithiasis | Yes |
| Location of stones | ||
| Presence of biliary strictures | ||
| Presence of biliary dilation | ||
| LHO classification system[68] | Tolerance to anatomical hepatectomy | Yes |
| Distribution of stones | ||
| Presence of parenchymal atrophy | ||
| Presence of hilar stricture | ||
| Function of the sphincter of Oddi |
Dong’s classification
Feng et al[65] reported results from a cohort of 2000 patients being treated for hepatolithiasis in 2012. They proposed a classification method based on location of the stones, presence of hepatic atrophy, biliary stricture, cirrhosis, and the function of the sphincter of Oddi.
Hepatolithiasis type I is characterised by localised stones and is subdivided into Ia, when stones are in one lobe, and Ib, when stones are in both lobes. Type II is defined by diffuse disease and has three subtypes: type IIa has no hepatic atrophy or bile duct stenosis, type IIb has segmental atrophy and/or biliary strictures, and type IIc has biliary cirrhosis and portal hypertension. Type E is used to characterise disease with extrahepatic stones and is divided into Ea, when the sphincter of Oddi has normal function, Eb when there is relaxation of the sphincter, and Ec when there is stenosis of the sphincter of Oddi.
Nakayama’s classification
In 1982, Nakayama reported his classification criteria for hepatolithiasis[66]. This is solely based on a thorough and objective description of the type of stones, location of stones, presence of biliary stenosis, its severity and site, and presence of biliary dilation, its severity and location. This classification also includes whether the gallbladder contains stones, whether there is dysfunction of sphincter of Oddi and whether the patient has undergone previous operations.
The severity of biliary stenosis is graded as S0 when there is none, S1 when the related bile duct’s diameter is more than 2 mm (mild stricture), and S2 when the bile duct’s diameter is less than 2 mm (marked stricture). Biliary dilation is graded using D0 for absence, D1 for dilation less than 20 mm, and D2 for dilation more than 20 mm.
Although being informative and profoundly descriptive, it has to be noted that this method may be difficult to interpret to those that are not often exposed to patients with hepatolithiasis. Furthermore, the classification does not suggest the preferred method of treatment which could guide surgeons with less expertise in hepatolithiasis.
Tsunoda classification
Tsunoda et al[67], in 1985, published a method to classify patients with hepatolithiasis. These criteria divided patients based on primary and secondary hepatolithiasis, the location of stones, the presence of biliary strictures and/or dilations. According to each classification, they recommended which operation would lend the best surgical outcomes.
Patients with type I have small stones and no dilation of bile ducts, while patients with type II have diffuse dilation of intrahepatic ducts with or without an obstructive lesion on the CBD. Both types are associated with concomitant choledocholithiasis. The Tsunoda classification suggests that these patients might develop hepatolithiasis due to an extrahepatic factor and called both types as secondary intrahepatic stones. Type III is characterised by unilateral cystic lesions with or without strictures, and type IV is represented by diffuse disease occupying both lobes.
LHO Classification System
The most recent classification method was published by Wang et al[68] in 2023. They named it LHO Classification System, where each letter indicates one of the three key points assessed to formulate an effective surgical plan and standardize the treatment of patients with hepatolithiasis. The first letter, L, assesses the distribution of the stones in the segmental bile ducts, the presence of hepatic atrophy and patient’s tolerance to anatomical hepatectomy. H refers to the presence or absence of stones at the hilum or hilar strictures, and O indicates whether or not there is dysfunction of the sphincter of Oddi.
With regards to the subtypes of type L, L0 refers to the absence of obvious stones in the segmental bile ducts or obvious atrophy of the hepatic parenchyma, along with normal liver function. In subtype L1, there are stones in the segmental bile ducts and/or parenchymal atrophy and the patient can tolerate hepatectomy. Type L2 is also defined as complex hepatolithiasis, as it indicates diffuse disease and atrophy, without feasibility for anatomical hepatectomy of all the affected segments within the safe limits of resectability according to the criteria of the University of Zurich[69].
Type H refers to strictures and obstructive stones at the liver hilum. These need to be removed to prevent chronic cholestasis and recurrent cholangitis/stone formation. H0 indicates the absence of hilar stones or strictures. Subtype H1 means that there are stones but no strictures around the hepatic hilum, while H2, instead, refers to the presence of both stones and hilar strictures and includes cases that are usually more difficult to manage.
Type O varies according to the functionality of the sphincter of Oddi, as its insufficiency may lead to duodenal fluid reflux into the biliary tree and recurrent cholangitis. Subtype O0 indicates normally functioning sphincter, in subtype O1 there is relaxation of the sphincter and subtype O2 refers to patients with a stricture of the sphincter of Oddi.
MANAGEMENT
Treatment of hepatolithiasis follows a stepwise approach and depends on symptoms and extension of hepatic/biliary involvement. Asymptomatic patients usually get diagnosed during investigations for other conditions. If there are no signs of cholangitis, biliary stricture and hepatic atrophy, as well as no history of biliary reconstruction, these patients can undergo active monitoring with regular follow-up using non-invasive imaging (e.g., ultrasound and magnetic resonance imaging)[70].
Symptomatic patients and those with complications should be managed by a multidisciplinary team involving hepatologists, hepatobiliary endoscopists, interventional radiologists and hepatobiliary surgeons[64]. If there is evidence of biliary strictures or history of biliary reconstruction, these patients require a more aggressive management, including invasive methods to remove stones and dilate stenotic ducts. Cases where hepatic atrophy is present should ideally undergo hepatectomy[71]. The most important goals during treatment of hepatolithiasis are removal of stones, resolution of strictures and prevention of cholangitis to hinder progression of the disease and development of CCA[72].
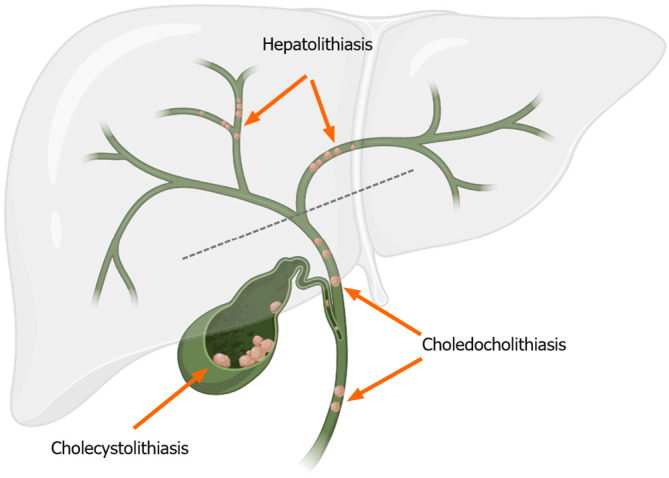
A schematic summary of the main treatments of hepatolithiasis according to clinical presentation is shown in Figure 2.
Figure 2.
Schematic summary of the main treatments of hepatolithiasis according to clinical presentation. POCSL: Peroral cholangioscopy with lithotomy; PTCSL: Percutaneous transhepatic cholangioscopic lithotomy.
Pharmacotherapy
Pharmacological treatment for hepatolithiasis lacks large controlled prospective studies, hence it is not recommended. Ursodeoxycholic acid (UDCA) decreases the secretion of cholesterol in the bile and inhibits intestinal reabsorption of cholesterol, while it facilitates bile flow via stimulation of hepatobiliary secretory function[73]. It has been used to prevent gallstone formation in cases of cholelithiasis/choledocholithiasis, as well as in cases of hepatolithiasis due to Caroli’s syndrome[74]. In primary hepatolithiasis, however, stones are commonly composed of calcium bilirubinate rather than cholesterol[75]. Even though it addresses part of the mechanism of stone formation, UDCA does not tackle the mechanisms leading to the deposition of bile crystals and formation of calcium bilirubinate stones.
Interventional management
Interventional treatment for hepatolithiasis involves various techniques, such as peroral cholangioscopy (POCS)[76], percutaneous transhepatic cholangioscopic lithotomy (PTCSL)[77], and percutaneous transhepatic balloon dilation[78].
POCS, associated or not with lithotomy has gained increased importance in the treatment of hepatolithiasis[79,80]. In a recent study evaluating the efficacy and safety of POCS (SpyGlass), technical success was achieved in 71.4% and clinical success in 57% of cases[81]. Similar results were previously reported in a larger retrospective study comparing the outcomes of hepatectomy (n = 90), PTCSL (n = 97) and POCS (n = 49)[46]. Complete stone clearance was achieved in 83.3% of hepatectomies, 63.9% of PTCSL, and 57.1% of POCS patients. PTCSL has a higher success rate, achieving complete stone removal in up to 85% of the cases, but with a recurrence rate reaching more than 50%[46,82-85]. Moreover, both POCS and PTCSL can also be used in association with extracorporeal shockwave lithotripsy to improve stone clearance rates to 90%[86,87]. It is important to highlight, however, that the presence of hepatic atrophy and/or biliary strictures hinders the success of these therapies, with complete stone removal rates of only 58%[88].
Surgical management
Hepatectomy reduces the risk of stone recurrence and progression to CCA[21,89]. Hence, in patients with bilateral disease, hepatic atrophy and who can tolerate a more major operation, anatomical resection of all liver segments affected by the disease is the ideal treatment. The surgical access (open vs minimally invasive) will depend mainly on whether the patient can tolerate pneumoperitoneum, as well as the expertise of the surgeon. There is evidence supporting non-inferiority of a laparoscopic approach on mortality, and superiority on acute endpoints like length of hospital stay and blood loss[90-94].
In 2021, Kim et al[95] developed and validated a difficulty scoring system (DSS) for laparoscopic liver resection. This considers location of the stone, atrophy of the hepatic parenchyma, extent of liver resection, ductal stricture within 1 cm of the bifurcation and combined choledochoscopic examination for remnant intrahepatic ducts. The score ranges between 3 and 12 points, with highest scores indicating increased level of surgical difficulty. When patients were divided into three subgroups according to DSS (DSS 3-5, DSS 6-8, and DSS 9-12), hospital stay (P = 0.05), operation time (P < 0.001) and blood loss (P = 0.004) were significantly different between the three subgroups.
Complicated hepatolithiasis is commonly characterised by intrahepatic stones with hepatic atrophy and hilar stenosis/distortion[45] It is essential that a multidisciplinary team gets involved in the treatment. Often patients will present with persistent stones after hepatic resection and almost 70% will also present with extrahepatic stones[5,96]. Therefore, it is important that hepatobiliary endoscopists, interventional radiologists and hepatobiliary surgeons define the best line of action to achieve complete stone removal as well as resolution of biliary strictures and resection of atrophic segments. These cases can be managed with a combination of peroral, or percutaneous lithotomy associated with hepatectomy of the most affected segments. Jiang et al[97] used laser lithotripsy combined with or without hepatectomy, achieving a final stone clearance rate of 93.3%. In very complex cases, patients might need to be considered for liver transplantation. Up to 15.6% of patients will require bile duct exploration after hepatectomy, due to incomplete stone clearance[98,99] and as many as 38.5% can present with recurrent hepatolithiasis[100]. These patients are also at high risk of developing biliary cancer, with as many as 9.7% been diagnosed with concomitant CCA[101], and up to 12.2% developing subsequent CCA during follow-up[102-104].
Malnutrition, which is associated with the pathogenesis of hepatolithiasis[3], is also associated with sarcopenia and obesity. Sarcopenia is a prognostic marker in chronic diseases, such as liver failure[105], as well as an independent risk factor for poor prognosis in malignancies[106]. In a large Chinese multicentre cohort, sarcopenia and sarcopenic obesity were associated with worse short-term outcomes after hepatectomy for hepatolithiasis. Patients with sarcopenia had a more difficult perioperative recovery period and a longer hospital stay (P < 0.001), along with higher rates of pneumonia (P = 0.017), bile leakage (P = 0.03), and rate of intensive care unit requirement (P = 0.004). Sarcopenic and obese patients had considerably worst intra- and post-operative outcomes, with a higher rate of blood loss (P < 0.001), longer operation time (P < 0.001), longer hospital stay (P < 0.001) and a higher incidence of post-operative major complications (P = 0.024)[107].
Dong, Tsunoda and LHO are the classification systems which also suggest the best treatment plan depending on the characteristics of hepatic and biliary involvement. For patients with localised disease and those with diffuse disease with parenchymal atrophy, the Dong and LHO criteria agree that the best outcomes are with hepatectomy. Nevertheless, it is important to take into consideration the Zurich criteria[69] for safe limits of resectability, which highlight that in the presence of normal liver function, the future liver remnant should be at least 30% of the total liver volume, while in cirrhotic patients with Child–Pugh grade A but without portal hypertension, this should be at least 50% of the total liver volume. Portal hypertension or Child–Pugh grade B/C are considered prohibitive for consideration of hepatectomy. Patients that could not tolerate an extensive hepatic resection should be treated with palliative lithotomy and hepatectomy of the smallest area possible. Some of these cases should be discussed with the transplant team to assess feasibility of OLT.
For patients that have concurrent biliary strictures and/or features associated with recurrent cholangitis and bile stasis, the classification systems have different recommendations. The Tsunoda classification argues that there is no difference in outcomes between different biliary reconstruction approaches (i.e., papilloplasty, hepaticoduodenostomy or hepaticojejunostomy) in patients with localised disease. However, this system discourages the use of choledochoduodenostomy and papilloplasty in cases with diffuse disease affecting both hepatic lobes due to the risk of ascending cholangitis. In these cases, Dong’s classification advocates for a hepaticojejunostomy. The LHO classification system, on the other hand, suggests that cases of intrahepatic strictures should be treated with hepatectomy of the affected segment. For hilar strictures, it suggests cholangiolithotomy and strictureplasty, leaving hepaticojejunostomy or choledochojejunostomy reserved to cases where the sphincter of Oddi is compromised.
In cases where hepatolithiasis has been complicated by development of intrahepatic CCA, curative-intent treatment can be pursued in the absence of metastatic disease, in the form of radical hepatic resection with or without lymphadenectomy, depending on individual circumstances[108-110]. Depending on the location and size of the tumour, the extend of the required hepatectomy varies from minor to major and, of course the Zurich criteria[66] need to be taken into account, with particular attention to the state of the future liver remnant, in the context of hepatolithiasis.
Liver transplantation
As long-standing hepatolithiasis may be characterised by repeated episodes of cholangitis, liver abscesses and liver atrophy, it can consequentially lead to secondary biliary cirrhosis with portal hypertension and liver failure[49,111]. In this setting, OLT is an option, even though relevant experience is scarce, with no more than 30 cases reported[49,111-113]. However, all patients transplanted for hepatolithiasis had favourable long-term outcomes, with the majority having developed secondary biliary cirrhosis prior to OLT[49,111-113]. Postoperative complications were not uncommon, but no mortality has been recorded[49,111-113]. In 2008, Chen et al[112] published their experience with 15 patients who underwent OLT for hepatolithiasis. All recipients had at least one biliary operation prior to OLT. Hepaticojejunostomy was used in all 15 cases for biliary reconstruction. All recipients had significantly improved health status, disability, and psychological wellness at 1-year post-transplant, and improved quality of life overall. Based on their successful experience, Chen et al[112] proposed two categories of patients with hepatolithiasis suitable for treatment with OLT: (1) Those with decompensated secondary biliary cirrhosis with liver failure; and (2) those with compensated secondary biliary cirrhosis or even absence of cirrhosis, with frequent episodes of cholangitis and diffuse bilateral intrahepatic calculi that are not suitable for treatment with hepatectomy, hepaticojejunostomy, and choledochoscopic intervention.
Notably, it must be mentioned that even though OLT is largely considered contraindicated for the management of intrahepatic CCA, in recent years, there has been a number of studies with excellent outcomes. Consequently, the European Network for the study of CCA issued a consensus statement recommendation that OLT should be considered especially in patients with very early stage unresectable intrahepatic CCA (≤ 2 cm) and underlying cirrhosis, as a potentially curative option[109,114]. It appears plausible that such cases may indeed arise in the context of hepatolithiasis.
PROGNOSIS
Particularly when hepatolithiasis becomes a recurrently symptomatic disease, clinicians need appropriate strategies to assess prognosis and choose the adequate treatment for these patients. Suzuki et al[115] used a Japanese cohort followed up for 18 years, to develop a severity classification system for hepatolithiasis. The authors identified liver cirrhosis, intrahepatic CCA, age ≥ 65 years and jaundice occurring for ≥ 1 wk during follow-up as independent prognostic factors in patients with hepatolithiasis. The group then divided these risk factors in major (including intrahepatic CCA and cirrhosis), and minor (including age ≥ 65 years and jaundice at ≥ 1 wk during follow-up). Their system considers these four criteria and divides patients into three groups according to the presence of these factors (i.e., Grade 1 - no factors, Grade 2 - only minor factors, one or both, Grade 3 - one or both major factors). The 5-year survival for patients considered Grade 1 is 97.6%, while it drops to 89.2% and 57.1% for Grade 2 and Grade 3, respectively. Pu et al[100] recently created a nomogram with good accuracy to predict the prognosis of patients with recurrent hepatolithiasis after biliary surgery. The variables used in this algorithm include previous surgery for hepatolithiasis, bilateral intrahepatic stones, lack of immediate clearance after operation, neutrophil to lymphocyte ratio ≥ 2.462 and albumin to globulin ratio ≤ 1.5, as independent risk factors for poor prognosis. This nomogram demonstrated superior accuracy than previous models used for prognosis assessment.
Deng et al[116], in a prospective cohort study, divided 121 patients who underwent liver resection for intrahepatic CCA into four groups, namely sarcopenia and hepatolithiasis (S-HL), sarcopenia without hepatolithiasis (S-NHL), non-sarcopenia with hepatolithiasis (NS-HL) and non-sarcopenia without hepatolithiasis (NS-NHL). They observed that the first group had the worse prognosis with overall survival 11.5 months (P < 0.001). The assessment of recurrence-free survival detected significant differences between the S-HL group and the NS-HL group (P = 0.005), and between the S-HL group and the NS-NHL group (P < 0.001), both in favour of the absence of sarcopenia, but no significant difference between the S-HL group and the S-NHL group (P = 0.054). Authors also identified age, hepatolithiasis, psoas muscle index, and diabetes as independent prognostic factors for overall survival, while age, hepatolithiasis and psoas muscle index are independent prognostic factors for recurrence-free survival.
Nevertheless, these prognostic factors and risk-stratification system require validation in larger and international cohorts.
CONCLUSION
Hepatolithiasis seems to be dependent on environmental, rather than genetic and ethnic factors. Its clinical manifestations involve a wide spectrum and severity, and complex cases can be challenging to treat. Such cases require input from a multidisciplinary team of hepatologists, endoscopists, interventional radiologists and hepatobiliary surgeons. Classification systems aim to provide useful insight of clinically relevant aspects and guidance for treatment but can be occasionally complex and require further validation. Accumulating expertise with endoscopic and interventional radiology techniques may further expand their application in treating a greater number and more challenging cases. However, the most complex cases require surgical input, alone or in combination with interventional approaches. Surgical or combined treatment should be aggressive and aim, where possible, to remove all affected segments and intrahepatic stones, to reduce the risk of recurrence and development of CCA.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interests for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: General Medical Council (UK), 7451513; Royal College of Surgeons of England, 9092145; American College of Surgeons, 03340060; International College of Surgeons, M21313; Faculty of Surgical Trainers of Edinburgh, Royal College of Surgeons of Edinburgh, 188646; Hellenic Surgical Society, 1974; Athens Medical Association, 061331; Institute of Clinical Research, 002934; and Society of Surgical Oncology, 132496.
Peer-review started: January 31, 2024
First decision: February 8, 2024
Article in press: March 13, 2024
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papadopoulos VP, Greece; Sintusek P, Thailand S-Editor: Lin C L-Editor: A P-Editor: Yu HG
Contributor Information
Rodrigo V. Motta, Translational Gastroenterology and Liver Unit, Nuffield Department of Medicine, University of Oxford, Oxford OX3 9DU, United Kingdom
Francesca Saffioti, Department of Gastroenterology and Hepatology, Oxford University Hospitals NHS Foundation Trust, John Radcliffe Hospital, Oxford OX3 9DU, United Kingdom; UCL Institute for Liver and Digestive Health and Sheila Sherlock Liver Unit, Royal Free Hospital and University College London, London NW3 2QG, United Kingdom.
Vasileios K Mavroeidis, Department of HPB Surgery, Bristol Royal Infirmary, University Hospitals Bristol and Weston NHS Foundation Trust, Bristol BS2 8HW, United Kingdom; Department of Transplant Surgery, North Bristol NHS Trust, Southmead Hospital, Bristol BS10 5NB, United Kingdom; Department of Gastrointestinal Surgery, North Bristol NHS Trust, Southmead Hospital, Bristol BS10 5NB, United Kingdom. vasileios.mavroeidis@nhs.net.
References
- 1. Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. London: National Institute for Health and Care Excellence (NICE); 2014 Oct- [PubMed] [Google Scholar]
- 2.Kim IS, Myung SJ, Lee SS, Lee SK, Kim MH. Classification and nomenclature of gallstones revisited. Yonsei Med J. 2003;44:561–570. doi: 10.3349/ymj.2003.44.4.561. [DOI] [PubMed] [Google Scholar]
- 3.Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, Park JJ, Byun KS, Bak YT. Hepatolithiasis and intrahepatic cholangiocarcinoma: A review. World J Gastroenterol. 2015;21:13418–13431. doi: 10.3748/wjg.v21.i48.13418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.You MS, Lee SH, Kang J, Choi YH, Choi JH, Shin BS, Huh G, Paik WH, Ryu JK, Kim YT, Jang DK, Lee JK. Natural Course and Risk of Cholangiocarcinoma in Patients with Recurrent Pyogenic Cholangitis: A Retrospective Cohort Study. Gut Liver. 2019;13:373–379. doi: 10.5009/gnl18339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsui WM, Lam PW, Lee WK, Chan YK. Primary hepatolithiasis, recurrent pyogenic cholangitis, and oriental cholangiohepatitis: a tale of 3 countries. Adv Anat Pathol. 2011;18:318–328. doi: 10.1097/PAP.0b013e318220fb75. [DOI] [PubMed] [Google Scholar]
- 6.COOK J, HOU PC, HO HC, McFADZEAN AJ. Recurrent pyogenic cholangeitis. Br J Surg. 1954;42:188–203. doi: 10.1002/bjs.18004217211. [DOI] [PubMed] [Google Scholar]
- 7.Digby KH. Common-duct stones of liver origin. Brit J Surg. 1930;17:578–591. [Google Scholar]
- 8.Sakpal SV, Babel N, Chamberlain RS. Surgical management of hepatolithiasis. HPB (Oxford) 2009;11:194–202. doi: 10.1111/j.1477-2574.2009.00046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mage S, Morel AS. Surgical experience with cholangiohepatitis (hong kong disease) in canton chinese. Ann Surg. 1965;162:187–190. doi: 10.1097/00000658-196508000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mori T, Sugiyama M, Atomi Y. Gallstone disease: Management of intrahepatic stones. Best Pract Res Clin Gastroenterol. 2006;20:1117–1137. doi: 10.1016/j.bpg.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Huang MH, Chen CH, Yen CM, Yang JC, Yang CC, Yeh YH, Chou DA, Yueh SK, Yang YY, Nien CK. Relation of hepatolithiasis to helminthic infestation. J Gastroenterol Hepatol. 2005;20:141–146. doi: 10.1111/j.1440-1746.2004.03523.x. [DOI] [PubMed] [Google Scholar]
- 12.Fung J. Liver fluke infestation and cholangio-hepatitis. Br J Surg. 1961;48:404–415. doi: 10.1002/bjs.18004821009. [DOI] [PubMed] [Google Scholar]
- 13.Lo CM, Fan ST, Wong J. The changing epidemiology of recurrent pyogenic cholangitis. Hong Kong Med J. 1997;3:302–304. [PubMed] [Google Scholar]
- 14.Su CH, Lui WY, P'eng FK. Relative prevalence of gallstone diseases in Taiwan. A nationwide cooperative study. Dig Dis Sci. 1992;37:764–768. doi: 10.1007/BF01296436. [DOI] [PubMed] [Google Scholar]
- 15.Glenn F, Moody FG. Intrahepatic calculi. Ann Surg. 1961;153:711–724. doi: 10.1097/00000658-196105000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Sukhni W, Gallinger S, Pratzer A, Wei A, Ho CS, Kortan P, Taylor BR, Grant DR, McGilvray I, Cattral MS, Langer B, Greig PD. Recurrent pyogenic cholangitis with hepatolithiasis--the role of surgical therapy in North America. J Gastrointest Surg. 2008;12:496–503. doi: 10.1007/s11605-007-0398-2. [DOI] [PubMed] [Google Scholar]
- 17.Herman P, Bacchella T, Pugliese V, Montagnini AL, Machado MA, da Cunha JE, Machado MC. Non-Oriental primary intrahepatic lithiasis: experience with 48 cases. World J Surg. 2005;29:858–62; discussion 863. doi: 10.1007/s00268-005-7759-3. [DOI] [PubMed] [Google Scholar]
- 18.Lindström CG. Frequency of gallstone disease in a well-defined Swedish population. A prospective necropsy study in Malmö. Scand J Gastroenterol. 1977;12:341–346. doi: 10.3109/00365527709180938. [DOI] [PubMed] [Google Scholar]
- 19.Gupta A, Simo K. Recurrent Pyogenic Cholangitis. 2022 Oct 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan- [PubMed] [Google Scholar]
- 20.Lorio E, Patel P, Rosenkranz L, Patel S, Sayana H. Management of Hepatolithiasis: Review of the Literature. Curr Gastroenterol Rep. 2020;22:30. doi: 10.1007/s11894-020-00765-3. [DOI] [PubMed] [Google Scholar]
- 21.Suzuki Y, Mori T, Yokoyama M, Nakazato T, Abe N, Nakanuma Y, Tsubouchi H, Sugiyama M. Hepatolithiasis: analysis of Japanese nationwide surveys over a period of 40 years. J Hepatobiliary Pancreat Sci. 2014;21:617–622. doi: 10.1002/jhbp.116. [DOI] [PubMed] [Google Scholar]
- 22.Ran X, Yin B, Ma B. Four Major Factors Contributing to Intrahepatic Stones. Gastroenterol Res Pract. 2017;2017:7213043. doi: 10.1155/2017/7213043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen G, Wu J, Xiao L, Wen Y, Yang T, Wang S. Right posteroinferior bile duct angulation correlates with bile duct stone occurrence in patients with hepatolithiasis. Abdom Radiol (NY) 2020;45:3103–3108. doi: 10.1007/s00261-020-02444-3. [DOI] [PubMed] [Google Scholar]
- 24.Liang T, Su W, Zhang Q, Li G, Gao S, Lou J, Zhang Y, Ma T, Bai X. Roles of Sphincter of Oddi Laxity in Bile Duct Microenvironment in Patients with Cholangiolithiasis: From the Perspective of the Microbiome and Metabolome. J Am Coll Surg. 2016;222:269–280.e10. doi: 10.1016/j.jamcollsurg.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Su Y, Wu S, Fan Y, Jin J, Zhang Z. The preliminary experimental and clinical study of the relationship between the pigment gallstone and intestinal mucosal barrier. J Gastroenterol Hepatol. 2009;24:1451–1456. doi: 10.1111/j.1440-1746.2009.05842.x. [DOI] [PubMed] [Google Scholar]
- 26.Merritt ME, Donaldson JR. Effect of bile salts on the DNA and membrane integrity of enteric bacteria. J Med Microbiol. 2009;58:1533–1541. doi: 10.1099/jmm.0.014092-0. [DOI] [PubMed] [Google Scholar]
- 27.Xiao Z, Huang Z, Gao J, Wang J, Lei J, Zhou F, Yin X, Liao W, Wu L. The imbalance of biliary microflora in hepatolithiasis. Microb Pathog. 2021;157:104966. doi: 10.1016/j.micpath.2021.104966. [DOI] [PubMed] [Google Scholar]
- 28.Litvak Y, Byndloss MX, Tsolis RM, Bäumler AJ. Dysbiotic Proteobacteria expansion: a microbial signature of epithelial dysfunction. Curr Opin Microbiol. 2017;39:1–6. doi: 10.1016/j.mib.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Liu Z, Tian F, Feng X, He Y, Jiang P, Li J, Guo F, Zhao X, Chang H, Wang S. LPS increases MUC5AC by TACE/TGF-α/EGFR pathway in human intrahepatic biliary epithelial cell. Biomed Res Int. 2013;2013:165715. doi: 10.1155/2013/165715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LaMorte WW, LaMont JT, Hale W, Booker ML, Scott TE, Turner B. Gallbladder prostaglandins and lysophospholipids as mediators of mucin secretion during cholelithiasis. Am J Physiol. 1986;251:G701–G709. doi: 10.1152/ajpgi.1986.251.5.G701. [DOI] [PubMed] [Google Scholar]
- 31.Afdhal NH, Ostrow JD, Koehler R, Niu N, Groen AK, Veis A, Nunes DP, Offner GD. Interaction of bovine gallbladder mucin and calcium-binding protein: effects on calcium phosphate precipitation. Gastroenterology. 1995;109:1661–1672. doi: 10.1016/0016-5085(95)90656-8. [DOI] [PubMed] [Google Scholar]
- 32.Nakano T, Yanagisawa J, Nakayama F. Phospholipase activity in human bile. Hepatology. 1988;8:1560–1564. doi: 10.1002/hep.1840080615. [DOI] [PubMed] [Google Scholar]
- 33.Stewart L, Oesterle AL, Erdan I, Griffiss JM, Way LW. Pathogenesis of pigment gallstones in Western societies: the central role of bacteria. J Gastrointest Surg. 2002;6:891–903; discussion 903. doi: 10.1016/s1091-255x(02)00035-5. [DOI] [PubMed] [Google Scholar]
- 34.Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic) Best Pract Res Clin Gastroenterol. 2006;20:1075–1083. doi: 10.1016/j.bpg.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 35.Cliffe LJ, Humphreys NE, Lane TE, Potten CS, Booth C, Grencis RK. Accelerated intestinal epithelial cell turnover: a new mechanism of parasite expulsion. Science. 2005;308:1463–1465. doi: 10.1126/science.1108661. [DOI] [PubMed] [Google Scholar]
- 36.Hasnain SZ, Evans CM, Roy M, Gallagher AL, Kindrachuk KN, Barron L, Dickey BF, Wilson MS, Wynn TA, Grencis RK, Thornton DJ. Muc5ac: a critical component mediating the rejection of enteric nematodes. J Exp Med. 2011;208:893–900. doi: 10.1084/jem.20102057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alam S, Mustafa G, Rahman S, Kabir SA, Rashid HO, Khan M. Comparative study on presentation of biliary ascariasis with dead and living worms. Saudi J Gastroenterol. 2010;16:203–206. doi: 10.4103/1319-3767.65200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang C, Yang J, Li E, Luo S, Sun C, Liao Y, Li M, Ge J, Lei J, Zhou F, Wu L, Liao W. Metabolic signatures of hepatolithiasis using ultra-high performance liquid chromatography-tandem mass spectrometry. Metabolomics. 2022;18:69. doi: 10.1007/s11306-022-01927-2. [DOI] [PubMed] [Google Scholar]
- 39.Pan S, Li X, Jiang P, Jiang Y, Shuai L, He Y, Li Z. Variations of ABCB4 and ABCB11 genes are associated with primary intrahepatic stones. Mol Med Rep. 2015;11:434–446. doi: 10.3892/mmr.2014.2645. [DOI] [PubMed] [Google Scholar]
- 40.Shoda J, Inada Y, Osuga T. Molecular pathogenesis of hepatolithiasis--a type of low phospholipid-associated cholelithiasis. Front Biosci. 2006;11:669–675. doi: 10.2741/1826. [DOI] [PubMed] [Google Scholar]
- 41.Yang L, Junmin S, Hong Y, Shuodong W. PGE(2) induces MUC2 and MUC5AC expression in human intrahepatic biliary epithelial cells via EP4/p38MAPK activation. Ann Hepatol. 2013;12:479–486. [PubMed] [Google Scholar]
- 42.Kelly T, Buxbaum J. Gastrointestinal Manifestations of Cystic Fibrosis. Dig Dis Sci. 2015;60:1903–1913. doi: 10.1007/s10620-015-3546-7. [DOI] [PubMed] [Google Scholar]
- 43.Tsui WM, Chan YK, Wong CT, Lo YF, Yeung YW, Lee YW. Hepatolithiasis and the syndrome of recurrent pyogenic cholangitis: clinical, radiologic, and pathologic features. Semin Liver Dis. 2011;31:33–48. doi: 10.1055/s-0031-1272833. [DOI] [PubMed] [Google Scholar]
- 44.Lim JH. Oriental cholangiohepatitis: pathologic, clinical, and radiologic features. AJR Am J Roentgenol. 1991;157:1–8. doi: 10.2214/ajr.157.1.2048504. [DOI] [PubMed] [Google Scholar]
- 45.Shu J, Wang XJ, Li JW, Bie P, Chen J, Zheng SG. Robotic-assisted laparoscopic surgery for complex hepatolithiasis: a propensity score matching analysis. Surg Endosc. 2019;33:2539–2547. doi: 10.1007/s00464-018-6547-8. [DOI] [PubMed] [Google Scholar]
- 46.Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009;146:843–853. doi: 10.1016/j.surg.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 47.Chijiiwa K, Yamashita H, Yoshida J, Kuroki S, Tanaka M. Current management and long-term prognosis of hepatolithiasis. Arch Surg. 1995;130:194–197. doi: 10.1001/archsurg.1995.01430020084016. [DOI] [PubMed] [Google Scholar]
- 48.Kwan KEL, Shelat VG, Tan CH. Recurrent pyogenic cholangitis: a review of imaging findings and clinical management. Abdom Radiol (NY) 2017;42:46–56. doi: 10.1007/s00261-016-0953-y. [DOI] [PubMed] [Google Scholar]
- 49.Strong RW, Chew SP, Wall DR, Fawcett J, Lynch SV. Liver transplantation for hepatolithiasis. Asian J Surg. 2002;25:180–183. doi: 10.1016/S1015-9584(09)60170-6. [DOI] [PubMed] [Google Scholar]
- 50.Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014;383:2168–2179. doi: 10.1016/S0140-6736(13)61903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suzuki Y, Mori T, Momose H, Matsuki R, Kogure M, Abe N, Isayama H, Tazuma S, Tanaka A, Takikawa H, Sakamoto Y. Predictive factors for subsequent intrahepatic cholangiocarcinoma associated with hepatolithiasis: Japanese National Cohort Study for 18 years. J Gastroenterol. 2022;57:387–395. doi: 10.1007/s00535-022-01868-6. [DOI] [PubMed] [Google Scholar]
- 52.Liu ZY, Zhou YM, Shi LH, Yin ZF. Risk factors of intrahepatic cholangiocarcinoma in patients with hepatolithiasis: a case-control study. Hepatobiliary Pancreat Dis Int. 2011;10:626–631. doi: 10.1016/s1499-3872(11)60106-9. [DOI] [PubMed] [Google Scholar]
- 53.Borakati A, Froghi F, Bhogal RH, Mavroeidis VK. Stereotactic radiotherapy for intrahepatic cholangiocarcinoma. World J Gastrointest Oncol. 2022;14:1478–1489. doi: 10.4251/wjgo.v14.i8.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aishima S, Kubo Y, Tanaka Y, Oda Y. Histological features of precancerous and early cancerous lesions of biliary tract carcinoma. J Hepatobiliary Pancreat Sci. 2014;21:448–452. doi: 10.1002/jhbp.71. [DOI] [PubMed] [Google Scholar]
- 55.Zhou Q, Gong Y, Huang F, Lin Q, Zeng B, Li Z, Chen R. Expression levels and significance of nuclear factor-κB and epidermal growth factor receptor in hepatolithiasis associated with intrahepatic cholangiocarcinoma. Dig Surg. 2013;30:309–316. doi: 10.1159/000354341. [DOI] [PubMed] [Google Scholar]
- 56.Saffioti F, Mavroeidis VK. Review of incidence and outcomes of treatment of cholangiocarcinoma in patients with primary sclerosing cholangitis. World J Gastrointest Oncol. 2021;13:1336–1366. doi: 10.4251/wjgo.v13.i10.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Meng ZW, Han SH, Zhu JH, Zhou LY, Chen YL. Risk Factors for Cholangiocarcinoma After Initial Hepatectomy for Intrahepatic Stones. World J Surg. 2017;41:835–843. doi: 10.1007/s00268-016-3752-2. [DOI] [PubMed] [Google Scholar]
- 58.Yue PC. Recurrent pyogenic cholangitis in children. Aust N Z J Surg. 1974;44:53–56. doi: 10.1111/j.1445-2197.1974.tb06521.x. [DOI] [PubMed] [Google Scholar]
- 59.Saing H, Tam PK, Choi TK, Wong J. Childhood recurrent pyogenic cholangitis. J Pediatr Surg. 1988;23:424–429. doi: 10.1016/s0022-3468(88)80440-8. [DOI] [PubMed] [Google Scholar]
- 60.Enriquez G, Lucaya J, Allende E, Garcia-Peña P. Intrahepatic biliary stones in children. Pediatr Radiol. 1992;22:283–286. doi: 10.1007/BF02019861. [DOI] [PubMed] [Google Scholar]
- 61.Sanada Y, Sakuma Y, Onishi Y, Okada N, Hirata Y, Horiuchi T, Omameuda T, Lefor AK, Sata N. Hepatolithiasis After Living Donor Liver Transplantation in Pediatric Patients: Mechanism, Diagnosis, Treatment, and Prognosis. Transpl Int. 2022;35:10220. doi: 10.3389/ti.2022.10220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yan J, Zhang Z, Guo J, Lv C, Chen Y. Clinical characteristics and prognosis of primary hepatolithiasis in hospitalized children. Eur J Pediatr. 2023;182:3195–3202. doi: 10.1007/s00431-023-05003-2. [DOI] [PubMed] [Google Scholar]
- 63.Kim TK, Kim BS, Kim JH, Ha HK, Kim PN, Kim AY, Lee MG. Diagnosis of intrahepatic stones: superiority of MR cholangiopancreatography over endoscopic retrograde cholangiopancreatography. AJR Am J Roentgenol. 2002;179:429–434. doi: 10.2214/ajr.179.2.1790429. [DOI] [PubMed] [Google Scholar]
- 64.European Association for the Study of the Liver (EASL) EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65:146–181. doi: 10.1016/j.jhep.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 65.Feng X, Zheng S, Xia F, Ma K, Wang S, Bie P, Dong J. Classification and management of hepatolithiasis: A high-volume, single-center's experience. Intractable Rare Dis Res. 2012;1:151–156. doi: 10.5582/irdr.2012.v1.4.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nakayama F. Intrahepatic calculi: a special problem in East Asia. World J Surg. 1982;6:802–804. doi: 10.1007/BF01655381. [DOI] [PubMed] [Google Scholar]
- 67.Tsunoda T, Tsuchiya R, Harada N, Yoshino R, Noda T, Izawa K, Yamaguchi T, Yamamoto K. Long-term results of surgical treatment for intrahepatic stones. Jpn J Surg. 1985;15:455–462. doi: 10.1007/BF02470091. [DOI] [PubMed] [Google Scholar]
- 68.Wang W, Yang C, Wang J, Chen W. Hepatolithiasis Classification Based on Anatomical Hepatectomy. J Gastrointest Surg. 2023;27:914–925. doi: 10.1007/s11605-022-05572-x. [DOI] [PubMed] [Google Scholar]
- 69.Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007;356:1545–1559. doi: 10.1056/NEJMra065156. [DOI] [PubMed] [Google Scholar]
- 70.Tazuma S, Unno M, Igarashi Y, Inui K, Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, Ryozawa S, Nimura Y, Fujita N, Kubota K, Shoda J, Tabata M, Mine T, Sugano K, Watanabe M, Shimosegawa T. Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol. 2017;52:276–300. doi: 10.1007/s00535-016-1289-7. [DOI] [PubMed] [Google Scholar]
- 71.Miyazaki T, Shinkawa H, Takemura S, Tanaka S, Amano R, Kimura K, Ohira G, Nishio K, Kinoshita M, Tsuchi J, Ishihara A, Eguchi S, Shirai D, Yamamoto T, Wakasa K, Kawada N, Kubo S. Precancerous Lesions and Liver Atrophy as Risk Factors for Hepatolithiasis-Related Death after Liver Resection for Hepatolithiasis. Asian Pac J Cancer Prev. 2020;21:3647–3654. doi: 10.31557/APJCP.2020.21.12.3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T, Tanaka S, Kubo S. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009;198:199–202. doi: 10.1016/j.amjsurg.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 73.Wang HH, Portincasa P, de Bari O, Liu KJ, Garruti G, Neuschwander-Tetri BA, Wang DQ. Prevention of cholesterol gallstones by inhibiting hepatic biosynthesis and intestinal absorption of cholesterol. Eur J Clin Invest. 2013;43:413–426. doi: 10.1111/eci.12058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ros E, Navarro S, Bru C, Gilabert R, Bianchi L, Bruguera M. Ursodeoxycholic acid treatment of primary hepatolithiasis in Caroli's syndrome. Lancet. 1993;342:404–406. doi: 10.1016/0140-6736(93)92817-d. [DOI] [PubMed] [Google Scholar]
- 75.Shoda J, Tanaka N, Osuga T. Hepatolithiasis--epidemiology and pathogenesis update. Front Biosci. 2003;8:e398–e409. doi: 10.2741/1091. [DOI] [PubMed] [Google Scholar]
- 76.Kalaitzakis E, Webster GJ, Oppong KW, Kallis Y, Vlavianos P, Huggett M, Dawwas MF, Lekharaju V, Hatfield A, Westaby D, Sturgess R. Diagnostic and therapeutic utility of single-operator peroral cholangioscopy for indeterminate biliary lesions and bile duct stones. Eur J Gastroenterol Hepatol. 2012;24:656–664. doi: 10.1097/MEG.0b013e3283526fa1. [DOI] [PubMed] [Google Scholar]
- 77.Chen C, Huang M, Yang J, Yang C, Yeh Y, Wu H, Chou D, Yueh S, Nien C. Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis. Surg Endosc. 2005;19:505–509. doi: 10.1007/s00464-004-8125-5. [DOI] [PubMed] [Google Scholar]
- 78.Liu B, Cao PK, Wang YZ, Wang WJ, Tian SL, Hertzanu Y, Li YL. Modified percutaneous transhepatic papillary balloon dilation for patients with refractory hepatolithiasis. World J Gastroenterol. 2020;26:3929–3937. doi: 10.3748/wjg.v26.i27.3929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Troncone E, Mossa M, De Vico P, Monteleone G, Del Vecchio Blanco G. Difficult Biliary Stones: A Comprehensive Review of New and Old Lithotripsy Techniques. Medicina (Kaunas) 2022;58 doi: 10.3390/medicina58010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video) Gastrointest Endosc. 2007;65:832–841. doi: 10.1016/j.gie.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 81.Mansilla-Vivar R, Alonso-Lázaro N, Argüello-Viudez L, Ponce-Romero M, Bustamante-Balen M, Pons-Beltrán V. New management of hepatolithiasis: Can surgery be avoided? (with video) Gastroenterol Hepatol. 2020;43:188–192. doi: 10.1016/j.gastrohep.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 82.Yeh YH, Huang MH, Yang JC, Mo LR, Lin J, Yueh SK. Percutaneous trans-hepatic cholangioscopy and lithotripsy in the treatment of intrahepatic stones: a study with 5 year follow-up. Gastrointest Endosc. 1995;42:13–18. doi: 10.1016/s0016-5107(95)70236-9. [DOI] [PubMed] [Google Scholar]
- 83.Tao H, Wang P, Sun B, Li K, Zhu C. One-Step Multichannel Percutaneous Transhepatic Cholangioscopic Lithotripsy Applied in Bilateral Hepatolithiasis. World J Surg. 2020;44:1586–1594. doi: 10.1007/s00268-020-05368-7. [DOI] [PubMed] [Google Scholar]
- 84.Huang MH, Chen CH, Yang JC, Yang CC, Yeh YH, Chou DA, Mo LR, Yueh SK, Nien CK. Long-term outcome of percutaneous transhepatic cholangioscopic lithotomy for hepatolithiasis. Am J Gastroenterol. 2003;98:2655–2662. doi: 10.1111/j.1572-0241.2003.08770.x. [DOI] [PubMed] [Google Scholar]
- 85.Tripathi N, Mardini H, Koirala N, Raissi D, Emhmed Ali SM, Frandah WM. Assessing the utility, findings, and outcomes of percutaneous transhepatic cholangioscopy with Spyglass(TM) Direct visualization system: a case series. Transl Gastroenterol Hepatol. 2020;5:12. doi: 10.21037/tgh.2019.11.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ellis RD, Jenkins AP, Thompson RP, Ede RJ. Clearance of refractory bile duct stones with extracorporeal shockwave lithotripsy. Gut. 2000;47:728–731. doi: 10.1136/gut.47.5.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sackmann M, Holl J, Sauter GH, Pauletzki J, von Ritter C, Paumgartner G. Extracorporeal shock wave lithotripsy for clearance of bile duct stones resistant to endoscopic extraction. Gastrointest Endosc. 2001;53:27–32. doi: 10.1067/mge.2001.111042. [DOI] [PubMed] [Google Scholar]
- 88.Lee SK, Seo DW, Myung SJ, Park ET, Lim BC, Kim HJ, Yoo KS, Park HJ, Joo YH, Kim MH, Min YI. Percutaneous transhepatic cholangioscopic treatment for hepatolithiasis: an evaluation of long-term results and risk factors for recurrence. Gastrointest Endosc. 2001;53:318–323. doi: 10.1016/s0016-5107(01)70405-1. [DOI] [PubMed] [Google Scholar]
- 89.Torres OJM, Linhares MM, Ramos EJB, Amaral PCG, Belotto M, Lucchese AM, Neiva RF, Freitas TM, Santana R, Vieira JP, Freire JS, Torres CCS, Kalil AN. Liver resection for non-oriental hepatolithiasis. Arq Bras Cir Dig. 2019;32:e1463. doi: 10.1590/0102-672020190001e1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li H, Zheng J, Cai JY, Li SH, Zhang JB, Wang XM, Chen GH, Yang Y, Wang GS. Laparoscopic VS open hepatectomy for hepatolithiasis: An updated systematic review and meta-analysis. World J Gastroenterol. 2017;23:7791–7806. doi: 10.3748/wjg.v23.i43.7791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lei J, Huang J, Yang X, Zhang Y, Yao K. Minimally invasive surgery versus open hepatectomy for hepatolithiasis: A systematic review and meta analysis. Int J Surg. 2018;51:191–198. doi: 10.1016/j.ijsu.2017.12.038. [DOI] [PubMed] [Google Scholar]
- 92.Yao D, Wu S. Application of Laparoscopic Technique in the Treatment of Hepatolithiasis. Surg Laparosc Endosc Percutan Tech. 2020;31:247–253. doi: 10.1097/SLE.0000000000000871. [DOI] [PubMed] [Google Scholar]
- 93.Liu X, Min X, Ma Z, He X, Du Z. Laparoscopic hepatectomy produces better outcomes for hepatolithiasis than open hepatectomy: An updated systematic review and meta-analysis. Int J Surg. 2018;51:151–163. doi: 10.1016/j.ijsu.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 94.Wang X, Chen A, Fu Q, Cai C. Comparison of the Safety and Efficacy of Laparoscopic Left Lateral Hepatectomy and Open Left Lateral Hepatectomy for Hepatolithiasis: A Meta-Analysis. Front Surg. 2021;8:749285. doi: 10.3389/fsurg.2021.749285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kim J, Cho JY, Han HS, Yoon YS, Choi Y, Lee JS, Lee B, Kim J. Validation of a difficulty scoring system for laparoscopic liver resection in hepatolithiasis. Surg Endosc. 2021;35:1148–1155. doi: 10.1007/s00464-020-07479-7. [DOI] [PubMed] [Google Scholar]
- 96.Hu MG, Zhao GD, Ouyang CG, Xu DB, Liu R. Lithotomy using cholangioscopy via the left hepatic duct orifice versus the common bile duct in laparoscopic treatment of left-sided hepatolithiasis: a comparative study. J Laparoendosc Adv Surg Tech A. 2013;23:332–338. doi: 10.1089/lap.2012.0397. [DOI] [PubMed] [Google Scholar]
- 97.Jiang ZJ, Chen Y, Wang WL, Shen Y, Zhang M, Xie HY, Zhou L, Zheng SS. Management hepatolithiasis with operative choledochoscopic FREDDY laser lithotripsy combined with or without hepatectomy. Hepatobiliary Pancreat Dis Int. 2013;12:160–164. doi: 10.1016/s1499-3872(13)60026-0. [DOI] [PubMed] [Google Scholar]
- 98.Wen XD, Wang T, Huang Z, Zhang HJ, Zhang BY, Tang LJ, Liu WH. Step-by-step strategy in the management of residual hepatolithiasis using post-operative cholangioscopy. Therap Adv Gastroenterol. 2017;10:853–864. doi: 10.1177/1756283X17731489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liang L, Zhuang D, Feng X, Zhang K, Zhi X. The postoperative choledochoscopy in the management of the residual hepatolithiasis involving the caudate lobe: A retrospective study. Medicine (Baltimore) 2021;100:e26996. doi: 10.1097/MD.0000000000026996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pu T, Chen JM, Li ZH, Jiang D, Guo Q, Li AQ, Cai M, Chen ZX, Xie K, Zhao YJ, Wang C, Hou H, Lu Z, Geng XP, Liu FB. Clinical online nomogram for predicting prognosis in recurrent hepatolithiasis after biliary surgery: A multicenter, retrospective study. World J Gastroenterol. 2022;28:715–731. doi: 10.3748/wjg.v28.i7.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen DW, Tung-Ping Poon R, Liu CL, Fan ST, Wong J. Immediate and long-term outcomes of hepatectomy for hepatolithiasis. Surgery. 2004;135:386–393. doi: 10.1016/j.surg.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 102.Kim HJ, Kang TU, Swan H, Kang MJ, Kim N, Ahn HS, Park SM. Incidence and Prognosis of Subsequent Cholangiocarcinoma in Patients with Hepatic Resection for Bile Duct Stones. Dig Dis Sci. 2018;63:3465–3473. doi: 10.1007/s10620-018-5262-6. [DOI] [PubMed] [Google Scholar]
- 103.Kim HJ, Kim JS, Suh SJ, Lee BJ, Park JJ, Lee HS, Kim CD, Bak YT. Cholangiocarcinoma Risk as Long-term Outcome After Hepatic Resection in the Hepatolithiasis Patients. World J Surg. 2015;39:1537–1542. doi: 10.1007/s00268-015-2965-0. [DOI] [PubMed] [Google Scholar]
- 104.Lin CC, Lin PY, Chen YL. Comparison of concomitant and subsequent cholangiocarcinomas associated with hepatolithiasis: Clinical implications. World J Gastroenterol. 2013;19:375–380. doi: 10.3748/wjg.v19.i3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kim G, Kang SH, Kim MY, Baik SK. Prognostic value of sarcopenia in patients with liver cirrhosis: A systematic review and meta-analysis. PLoS One. 2017;12:e0186990. doi: 10.1371/journal.pone.0186990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Voron T, Tselikas L, Pietrasz D, Pigneur F, Laurent A, Compagnon P, Salloum C, Luciani A, Azoulay D. Sarcopenia Impacts on Short- and Long-term Results of Hepatectomy for Hepatocellular Carcinoma. Ann Surg. 2015;261:1173–1183. doi: 10.1097/SLA.0000000000000743. [DOI] [PubMed] [Google Scholar]
- 107.Wang T, Chen X, Liao C, Wang D, Huang L, Li G, Chen J, Lin C, Wang L, Pan J, Zhang C, Zhou S, Qiu F, Wang Y, Zhang Z, Chen Y, Zheng X, Tian Y, Chen S. Impact of sarcopenia on the surgical outcomes in patients with hepatolithiasis: A multicenter 10-year experience. Surgery. 2022;172:1712–1721. doi: 10.1016/j.surg.2022.09.007. [DOI] [PubMed] [Google Scholar]
- 108.Atif M, Borakati A, Mavroeidis VK. Role of routine lymph node dissection alongside resection of intrahepatic cholangiocarcinoma: Systematic review and meta-analysis. World J Gastrointest Oncol. 2023;15:2017–2032. doi: 10.4251/wjgo.v15.i11.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Saffioti F, Mavroeidis VK. Primary sclerosing cholangitis and cholangiocarcinoma: the 2023 practice guidance and future perspectives. Hepatobiliary Surg Nutr. 2024;13:172–175. doi: 10.21037/hbsn-23-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.McClements J, Valle JW, Blackburn L, Brooks A, Prachalias A, Dasari BVM, Jones C, Harrison E, Malik H, Prasad KR, Sodergren M, Silva M, Kumar N, Shah N, Bhardwaj N, Nunes Q, Bhogal RH, Pandanaboyana S, Aroori S, Hamady Z, Gomez D UK HPB Research Collaborative Group. Variation in treatment of intrahepatic cholangiocarcinoma: a nationwide multicentre study. Br J Surg. 2023;110:1673–1676. doi: 10.1093/bjs/znad259. [DOI] [PubMed] [Google Scholar]
- 111.Pan GD, Yan LN, Li B, Lu SC, Zeng Y, Wen TF, Zhao JC, Cheng NS, Ma YK, Wang WT, Yang JY, Li ZH. Liver transplantation for patients with hepatolithiasis. Hepatobiliary Pancreat Dis Int. 2005;4:345–349. [PubMed] [Google Scholar]
- 112.Chen ZY, Yan LN, Zeng Y, Wen TF, Li B, Zhao JC, Wang WT, Yang JY, Xu MQ, Ma YK, Wu H. Preliminary experience with indications for liver transplantation for hepatolithiasis. Transplant Proc. 2008;40:3517–3522. doi: 10.1016/j.transproceed.2008.07.142. [DOI] [PubMed] [Google Scholar]
- 113.Feng LB, Xia D, Yan LN. Liver transplantation for hepatolithiasis: Is terminal hepatolithiasis suitable for liver transplantation? Clin Transplant. 2016;30:651–658. doi: 10.1111/ctr.12731. [DOI] [PubMed] [Google Scholar]
- 114.Borakati A, Froghi F, Bhogal RH, Mavroeidis VK. Liver transplantation in the management of cholangiocarcinoma: Evolution and contemporary advances. World J Gastroenterol. 2023;29:1969–1981. doi: 10.3748/wjg.v29.i13.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Suzuki Y, Mori T, Yokoyama M, Kim S, Momose H, Matsuki R, Kogure M, Abe N, Isayama H, Nakazawa T, Notohara K, Tanaka A, Tsuyuguchi T, Tazuma S, Takikawa H, Sugiyama M. A proposed severity classification system for hepatolithiasis based on an analysis of prognostic factors in a Japanese patient cohort. J Gastroenterol. 2018;53:854–860. doi: 10.1007/s00535-017-1410-6. [DOI] [PubMed] [Google Scholar]
- 116.Deng L, Wang Y, Zhao J, Tong Y, Zhang S, Jin C, Chen K, Bao W, Yu Z, Chen G. The prognostic value of sarcopenia combined with hepatolithiasis in intrahepatic cholangiocarcinoma patients after surgery: A prospective cohort study. Eur J Surg Oncol. 2021;47:603–612. doi: 10.1016/j.ejso.2020.09.002. [DOI] [PubMed] [Google Scholar]