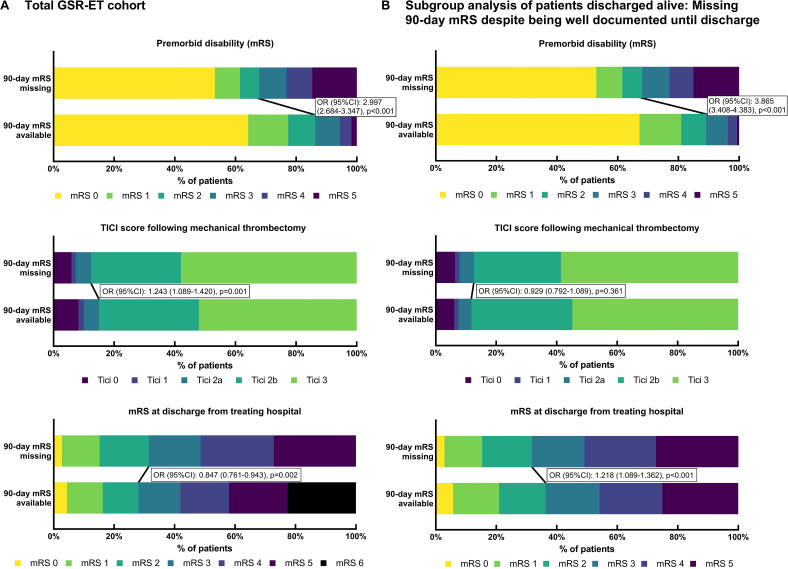
Figure 1.
Distribution of premorbid disability, recanalization status, and clinical outcome at discharge in cohorts of patients with 90 day missing clinical outcome data (MOD) versus those with data available. (A) Total German Stroke Registry-Endovascular Treatment (GSR-ET) cohort: MOD was associated with higher premorbid disability. Premorbid modified Rankin Scale (mRS) score was available in 10 195/10 502 (97.1%) patients with 90 day outcome available and in 1995/2580 (77.3%) patients with MOD. MOD was associated with successful recanalization (thrombolysis in cerebral infarction (TICI) scale score 2b–3); TICI was available in 10 173/10 502 (96.9%) patients with 90 day outcome available and in 2404/2580 (93.2%) patients with MOD. MOD was inversely associated with higher disability at discharge from the treating hospital as of mRS 3–6 versus 0–2; mRS at discharge was available in 9957/10 502 (94.8%) patients with 90 day outcome available and in 1858/2580 (72.0%) patients with MOD. (B) Subgroup analysis of patients discharged from hospital alive: comparison of patients with clinical outcome at 90 day follow-up available (n=7710) versus patients with MOD despite complete baseline documentation (age, sex, admission National Institutes of Health Stroke Scale score, intravenous thrombolysis, TICI, and mRS at discharge) (n=1706). MOD was associated with higher premorbid disability; premorbid mRS was available in 7606/7710 (98.7%) patients discharged from hospital alive with 90 day outcome available and in 1665/1706 (97.6%) patients with MOD despite complete baseline documentation. MOD was not significantly associated with successful recanalization (TICI 2b–3); TICI was available in 7537/7710 (97.8%) patients discharged from hospital alive with 90 day outcome available and in 1706/1706 (100.0%) patients with MOD despite complete baseline documentation. MOD was associated with higher disability at discharge from the treating hospital as of mRS 3–5 versus 0–2.