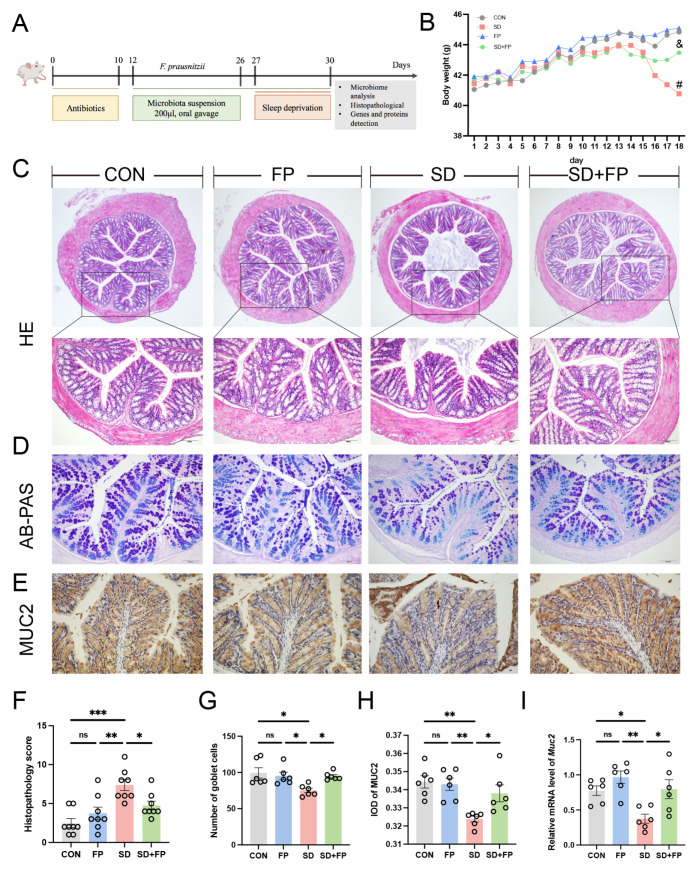
Figure 1.
Faecalibacterium prausnitzii colonization alleviated intestinal mucosal barrier disruption induced by SD. (A) Diagram showing the layout of the experiment. (B) Body weight. (C) Hematoxylin and eosin (H&E) staining, Bar = 100 μm. (D) Alcian blue, and periodic acid-Schiff (AB-PAS) staining, Bar = 100 μm. (E) Representative captures of immunohistochemical of MUC2 in colon, Bar = 100 μm. (F) Histologic scores (n = 8). (G) The number of goblet cells per crypt (n = 6). (H) IOD of MUC2 in the intestinal tissue from each treatment group (n = 6). (I) The mRNA levels of Muc2 in the colon (n = 6). One-way ANOVA was utilized to evaluate variances. The study included a control group (CON), a group colonized with Faecalibacterium prausnitzii (FP), a group subjected to sleep deprivation (SD), and a group experiencing sleep deprivation with Faecalibacterium prausnitzii colonization (SD + FP). The outcome indicates the average value plus or minus the standard error. *, p < 0.05; **, p < 0.01; ***, p < 0.001 compared with the control group. ns, non-significance. # p < 0.05 vs. the CON group; & p < 0.05 vs. the SD group.