Abstract
Purpose
To perform a systematic review to assess the diagnostic and prognostic value of cardiac MRI after sudden cardiac arrest (SCA).
Materials and Methods
PubMed and Cochrane Library databases were systematically searched for studies investigating cardiac MRI after SCA in adult patients (≥18 years of age). The time frame of the encompassed studies spans from January 2012 to January 2023. The study protocol was preregistered in OSF Registries (www.osf.io/nxaev), and the systematic review was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The quality of the included studies was evaluated using the Newcastle-Ottawa quality assessment scale.
Results
Fourteen studies involving 1367 individuals, 1257 (91.9%) of whom underwent cardiac MRI, were included. Inconsistent findings were reported on the diagnostic value of cardiac MRI–specific findings. The included studies demonstrated the following main findings: (a) cardiac MRI led to a new or alternative diagnosis in patients with SCA; (b) cardiac MRI identified pathologic or arrhythmogenic substrates; (c) cardiac MRI helped detect myocardial edema (potentially reversible); (d) cardiac MRI provided evidence for the occurrence of adverse events; and (e) functional markers or ventricular dimensions were considered prognostically relevant in a few studies. Relevant challenges in this systematic review were the lack of comparators and reference standards relative to cardiac MRI as the index test and patient selection bias.
Conclusion
Cardiac MRI following SCA can contribute to the diagnostic process and offer supplementary information essential for treatment planning. Limitations of the review include studies with insufficient comparators and potential bias in patient selection.
Systematic review registration link: osf.io/nxaev
Keywords: Cardiac MRI, Cardiovascular Disease, Cardiomyopathy, Ischemia, Myocardial Edema, Sudden Cardiac Arrest
© RSNA, 2024
Keywords: Cardiac MRI, Cardiovascular Disease, Cardiomyopathy, Ischemia, Myocardial Edema, Sudden Cardiac Arrest
Summary
Cardiac MRI may serve as an important diagnostic tool in the setting of sudden cardiac arrest to confirm further cardiac diagnoses and to initiate essential therapeutic steps after successful resuscitation.
Key Points
■ Through a systematic review of 14 studies involving 1367 patients, it was demonstrated that cardiac MRI not only leads to new or alternative diagnoses after sudden cardiac arrest (SCA) but also helps detect pathologic substrates, arrhythmogenic factors, myocardial edema, and provides evidence for major adverse cardiovascular events and/or arrhythmia.
■ The Newcastle-Ottawa quality assessment scale used to evaluate the quality and risk of bias of the included studies highlights limitations that include a lack of comparative data, patient selection bias, and challenges in study comparability, thus limiting definitive conclusions about diagnostic accuracy.
■ The analysis emphasizes the necessity for standardized approaches in future studies on cardiac MRI for SCA, proposing consensus guidelines to address heterogeneity, enhance interpretability, and facilitate robust meta-analyses, while considering complexities in postcardiac arrest physiology.
Introduction
MRI is essential in cardiology, especially for the assessment of inflammatory heart disease, infiltrative and storage diseases, scarring, cardiomyopathic (CMP) diagnostics, and workup in myocardial infarction in the presence or absence of obstructive coronary artery disease (1,2). Sudden cardiac arrest (SCA) is defined as a sudden failure of heart activity without any apparent noncardiac cause, resulting in cessation of breathing and the human body showing no signs of circulation (3,4). Incidence rates vary between 40 and 100 persons per 100 000, with regional variety (5). However, etiology differs with age, sex, and ethnicity, with channelopathies, CMPs, or inflammatory heart disease frequently being causative for SCA in younger individuals (5). The most common cause of SCA in young adults, up to approximately 30 years of age, is hypertrophic CMP; whereas, with advancing age, ischemic CMP is the main cause.
In the primary evaluation of SCA, the standard clinical pathway involves a systematic exploration to determine the etiology. This typically includes essential modalities such as electrocardiography (ECG), coronary angiography with potential revascularization, and transthoracic echocardiography (TTE). These initial assessments aim to identify and address emergent causes of cardiac arrest, such as acute myocardial infarction due to obstructive coronary artery disease (6). Once these immediate etiologies are explored and, if possible, ruled out, attention can be directed toward cases where the cause of cardiac arrest remains undetermined. In situations where standard tests prove inconclusive, advanced imaging modalities, such as cardiac MRI, play a crucial role in the secondary evaluation.
Cardiac MRI offers valuable insights into factors such as tissue scarring (eg, late gadolinium enhancement) and reversibility (eg, myocardial edema), providing additional diagnostic and prognostic information and aiding in treatment planning (7,8). Despite its potential significance, there is a notable absence of comprehensive data from large multicenter studies and standardized recommendations from professional societies on the implementation of cardiac MRI in the diagnostic workup after survival of primary SCA. To address this gap, we conducted a systematic review of the diagnostic and prognostic value of cardiac MRI in patients with primary SCA.
Materials and Methods
The systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (9). Meta-analysis was not deemed appropriate due to substantial heterogeneity among the included studies, with variations in study designs, the absence of direct comparisons, the descriptive nature of the included studies and outcome measures. To address this heterogeneity, we followed the Synthesis Without Meta-Analysis (SWiM) reporting guideline proposed by Campbell et al (10).
Literature Search
The systematic review was registered in advance (OSF Registries, www.osf.io/nxaev). A systematic literature search was conducted using the PubMed and Cochrane Library databases between September 28 and October 26, 2023, by two authors (R.R.–intensive care medicine, E.B.–cardiology) independently. We used the following as primary search terms: (“cardiac arrest” OR “resuscitation” OR “cardiac death”) AND (“MRI” OR “MRT” OR “magnetic resonance” OR “cardiac MRI”). “MRT” was used as an abbreviation for the less commonly used term “magnetic resonance tomography.” No automated search tools were used. To find unpublished reports, an additional search with the same keywords was performed in Social Science Research Network (SSRN). The time frame of the encompassed studies spans from January 2012 to January 2023.
Eligibility Criteria
Inclusion criteria for the studies were as follows: (a) a focus on cardiac MRI after SCA, (b) a relevant number of patients who underwent cardiac MRI included (>15 individuals), (c) randomized controlled trial or observational and/or cohort study (case reports and case series were excluded), (d) only human studies, (e) only adult patients (≥18 years of age), and (f) written in English or German language.
Study Selection and Data Extraction
All studies were screened at the title and abstract level, and further reading was performed on a full-text basis. All references of included studies were searched for further relevant studies. Duplicates were removed manually. Data were extracted by two authors (R.R., E.B.) independently. In case of disagreement between the two authors, a third author (B. Scharinger–radiology) was involved. Hereby, the authors achieved 100% agreement regarding the included literature and data extraction.
Quality Assessment
The Newcastle-Ottawa quality assessment scale was used to evaluate the quality and risk of bias of the involved studies and was independently performed by two different authors (B. Scharinger, S.H.–radiology) (11). In case of disagreement, a third author (K.H.–radiology) was consulted.
Data Analysis
The outcomes of interest encompassed a thorough examination of various factors related to cardiac MRI after SCA. The analysis of data involved the comprehensive assessment of diagnostic parameters, insights into treatment planning, and overall post-SCA patient outcomes. Additionally, the data analysis included the examination of diverse parameters such as cardiac function metrics, survival rates, and any adverse events or complications associated with the application of cardiac MRI in this context.
Results
Study Characteristics
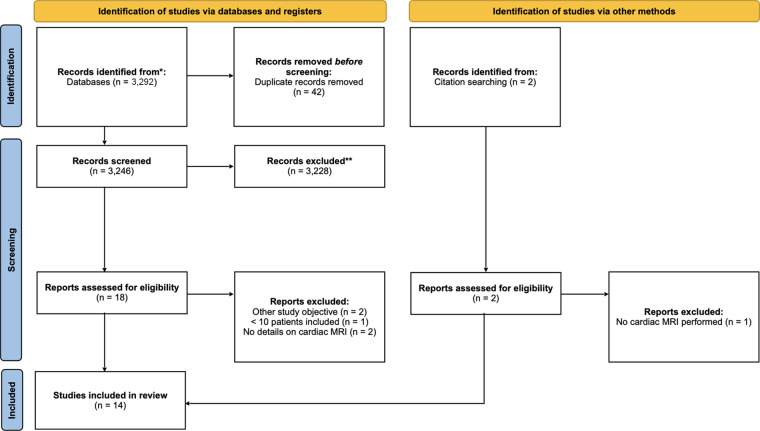
A total of 3292 studies were screened (3108 results from PubMed search, 182 results from Cochrane search, and two via additional sources). Among these, 14 studies were included in the final review (Figure); all studies were written in the English language. Of these, two studies were prospective, 11 studies used retrospective data, and one group of authors used both prospective and retrospective data in their work. None of the included studies achieved the status of a randomized controlled trial or case-control study. Four studies used patient data from more than one study center, with only one study including centers from two different countries. One work investigated the diagnostic pathway following survival of SCA in a developing country. A total of eight studies received funding, mostly public research grants.
Flow diagram shows the identification of studies according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. * = PubMed and Cochrane Library, ** = after abstracts were read.
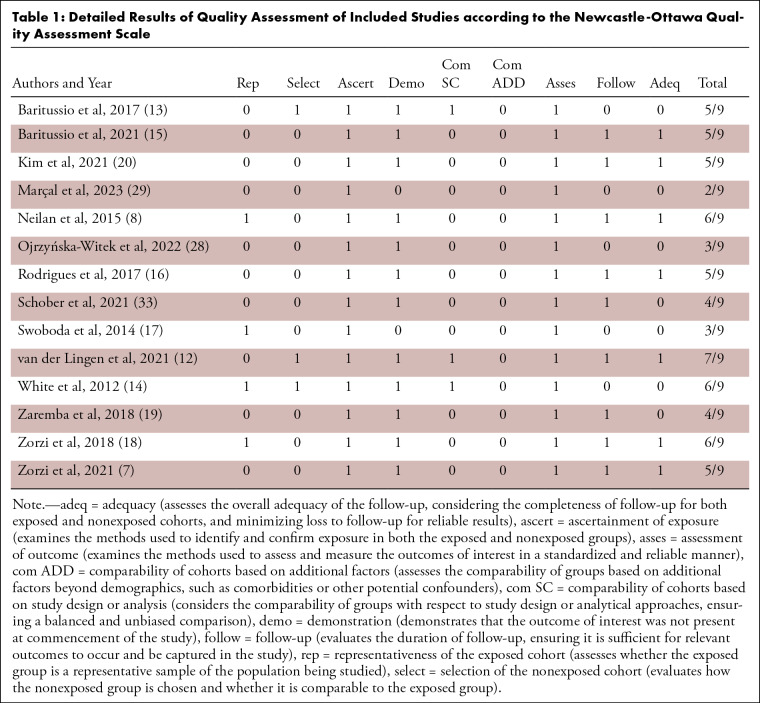
Quality of the Included Studies and Risk of Bias
According to the Newcastle-Ottawa scale, one of the 14 studies (7.1%) was scored as 2, two studies (14.2%) were scored as 3, two studies (14.2%) were scored as 4, five studies (35.7%) were scored as 5, three studies (21.4%) were scored as 6, and one study (7.1%) was scored as 7. The complete data for the Newcastle-Ottawa quality assessment are presented in Table 1.
Table 1:
Detailed Results of Quality Assessment of Included Studies according to the Newcastle-Ottawa Quality Assessment Scale
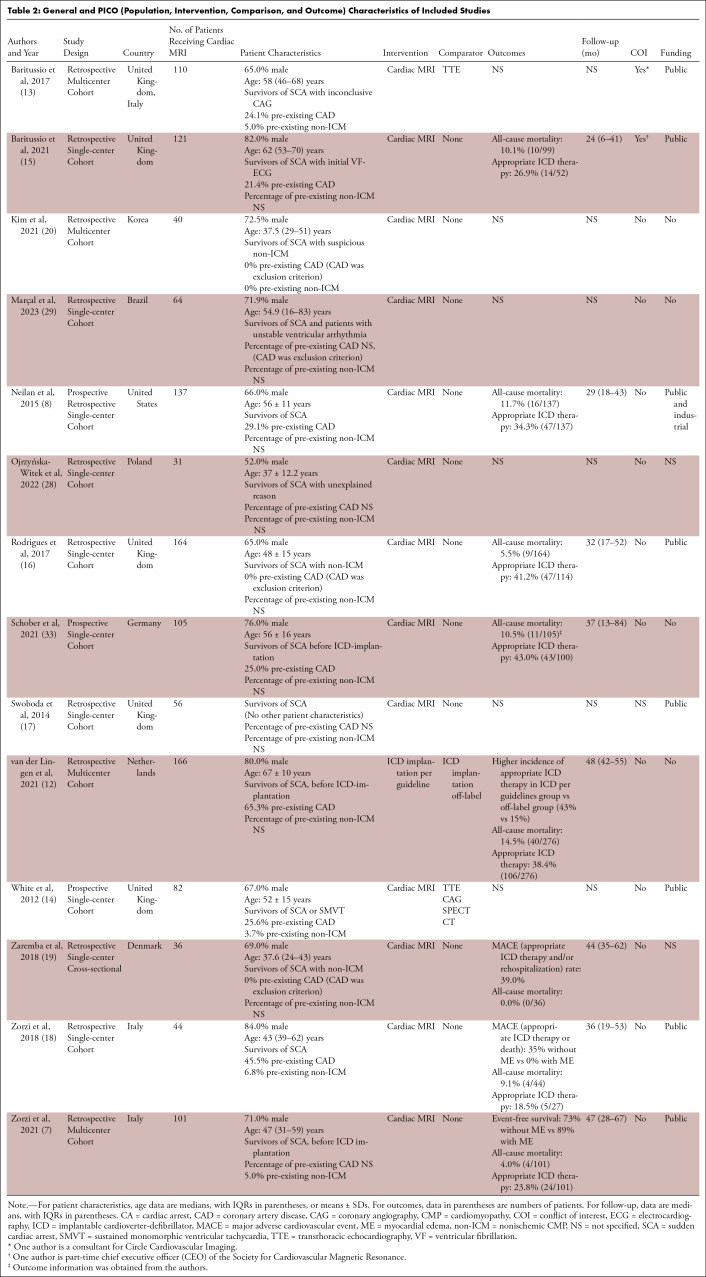
Patients, Interventions, Comparisons, and Outcomes
A total of 1367 individuals, 1257 (91.9%) of whom underwent cardiac MRI, were included in all 14 studies. Only three studies included additional patients with hemodynamically relevant ventricular tachycardia without the presence of cardiac arrest; all other studies included only patients after SCA. Similarly, only three studies included patient collectives outside of Europe (United States, Korea, and Brazil). The sex of study individuals was reported in 13 of 14 studies, with 72.0% of the included individuals from all studies being male. The median patient age varied widely between studies (range, 16–83 years). In 11 of 14 studies, no comparator group and/or reference standard was used (ie, cardiac MRI was the only intervention). One study (van der Lingen et al [12]) investigated implantable cardioverter-defibrillator placement per guidelines versus off-label use, where 166 of 276 patients (60%) underwent cardiac MRI. In all other studies, all included patients underwent cardiac MRI. Baritussio et al (13) performed TTE in 92 of 110 patients (84%). White et al (14) compared cardiac MRI versus noncardiac MRI. The reporting of outcomes (eg, all-cause mortality, major adverse cardiovascular events, rhythm events, or implantable cardioverter-defibrillator interventions) and follow-up varied widely across studies, with six reporting no outcome or follow-up data. Table 2 provides a general overview of the characteristics of the included studies.
Table 2:
General and PICO (Population, Intervention, Comparison, and Outcome) Characteristics of Included Studies
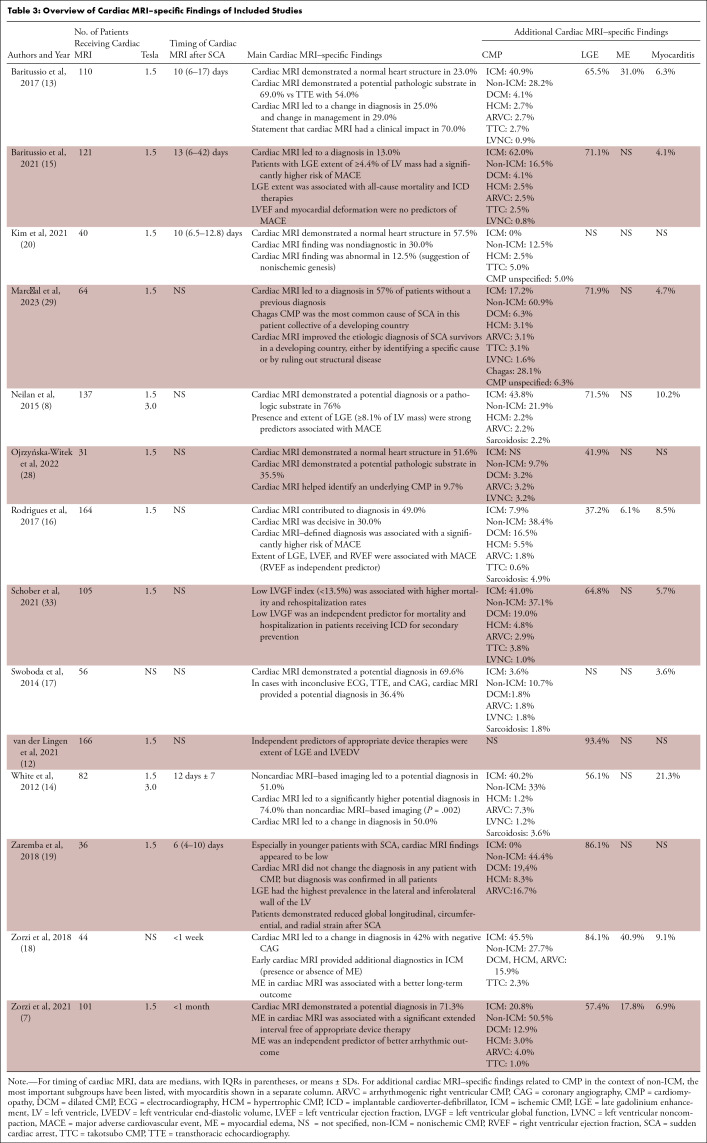
MRI-specific Findings
From a technical perspective, most studies used 1.5-T MRI scanners (10 of 14), whereas two studies also used 3-T scanners. Two author groups did not specify technical details on the MRI scanners used. Regarding the timing of cardiac MRI, two studies performed cardiac MRI within the first week after SCA, four studies performed it within the second week, and one study performed it within the first month after SCA. One study specified the timing as “during the index stay,” and six studies did not specify the timing of cardiac MRI.
The included studies demonstrated the following main cardiac MRI–specific findings: (a) cardiac MRI led to a new or alternate diagnosis in patients who had survived SCA, secondarily influencing the management of patients; (b) cardiac MRI identified pathologic or arrhythmogenic substrates; (c) cardiac MRI helped detect myocardial edema (a potentially reversible finding); (d) cardiac MRI provided evidence for the occurrence of adverse events, such as a major adverse cardiovascular event and/or arrhythmia; and (e) functional markers or ventricular dimensions were found to be prognostically relevant in only a few studies.
The diagnostic yield of cardiac MRI after SCA was reported inconsistently across studies. Several authors reported a change in diagnosis in 13%–50% of cases (13–16). Rodrigues et al (16) further stated that cardiac MRI was “crucial” for the diagnosis in 30% of cases. In another study, Swoboda et al (17) described that cardiac MRI enabled the correct diagnosis in 36.4% of cases where other imaging modalities were nondiagnostic. Other studies found that cardiac MRI was diagnostic in more than 70% of all cases yet lacked a comparator group (8,18). In turn, Zaremba et al (19) reported that cardiac MRI did not yield any new diagnoses, and Kim et al (20) found cardiac MRI after SCA not useful in their study overall.
Regarding additional MRI-specific findings, it should be noted that in 323 of 1060 patients (30.5%), ischemic CMP was diagnosed using cardiac MRI. Regarding nonischemic CMPs, 296 of 1091 patients (27.1%) presented with dilated CMP, hypertrophic CMP, arrhythmogenic right ventricular CMP, takotsubo CMP, or myocarditis. Only one study did not provide information on the presence of CMP. Myocarditis, the largest group of nonischemic CMP, was diagnosed in 78 of 984 patients (7.9%). A total of four studies did not report any information on the presence of myocarditis. Late gadolinium enhancement was observed in 771 of 1161 patients (66.4%). Two studies did not report any information on late gadolinium enhancement. Myocardial edema was found in 64 of 367 patients (17.4%; range, 6%–41%), while 10 studies did not report the presence or absence of myocardial edema. Table 3 summarizes the cardiac MRI–specific findings of the included studies.
Table 3:
Overview of Cardiac MRI–specific Findings of Included Studies
Discussion
In this systematic review of 14 studies including 1367 individuals with SCA, cardiac MRI demonstrated potential as a pivotal diagnostic tool. However, findings on its efficacy were inconsistent, revealing both the potential for new diagnoses and challenges such as patient selection bias. Despite these nuances, the relevance of cardiac MRI in treatment planning is evident, especially in patients with inconclusive prior diagnostics (ECG, TTE, coronary angiography).
Regarding the diagnostic workup of patients after SCA, ECG and TTE play a decisive role. ECG is crucial, as it may be indicative of the triggering cause of SCA (21,22). Beyond the essential value in diagnosing acute (eg, ST-elevation myocardial infarction) or chronic ischemia, ECG may provide important clues for the presence of an underlying CMP, such as hypertrophic CMP or arrhythmogenic right ventricular CMP (23,24). Moreover, surface ECG is crucial for the diagnosis of primary electrical disorders, such as inherited channelopathies (eg, Brugada syndrome, long and short QT syndrome, or other ionopathies) and Wolff-Parkinson-White syndrome (22). TTE is the first imaging modality used to find the presumed cause of SCA and a guide in the further diagnostic workup. When interpreted by an experienced provider, TTE indicates functional performance, serves as the reference standard for evaluating progression of valvular disease, and can establish the diagnosis of different CMPs such as dilated CMP, hypertrophic CMP, or takotsubo CMP. It is also a useful diagnostic tool for quickly recognizing and treating emergency situations, such as pericardial tamponade.
Nevertheless, there are indications for the use of cardiac MRI in the detailed workup of structural heart diseases and various cardiomyopathies, including ischemic CMP and hypertrophic CMP, as well as inflammatory heart diseases and cardiac storage diseases. One distinct advantage of cardiac MRI is its capability to provide detailed visualization of changes in myocardial texture and subepicardial structures, surpassing that of TTE. This is particularly relevant in the assessment of conditions, such as arrhythmogenic left ventricular CMP (25), where precise characterization of myocardial abnormalities is crucial for accurate diagnosis and subsequent management. Expanding our focus to ischemic CMP, cardiac MRI proves invaluable in delineating regions of myocardial ischemia and infarction. The high spatial resolution of the technique allows for the identification of myocardial scar tissue and assessment of perfusion abnormalities, contributing substantially to the understanding of ischemic heart diseases (26). In the realm of inflammatory CMP, the diagnostic capability of cardiac MRI extends beyond mere visualization. It enables the assessment of inflammation, tissue edema, and myocardial involvement with a level of detail that is essential for accurate diagnosis and tailored treatment strategies. Furthermore, in the evaluation of cardiac storage diseases, such as amyloidosis, sarcoidosis, or other infiltrative conditions, cardiac MRI provides critical insights into the structural changes and tissue composition of the myocardium. The ability to identify and quantify myocardial infiltration is crucial for guiding therapeutic decisions and understanding disease progression (27). The synergy of TTE and cardiac MRI substantially enriches the overall cardiac assessment, enabling a more comprehensive understanding of the patient's cardiac health (28). This combined approach enhances clinical decision-making and elevates the standard of patient care by providing a holistic view of cardiac structure, function, and tissue composition, thereby facilitating more informed diagnostic and therapeutic strategies for patients with various cardiomyopathies.
In developing countries, where health care resources and infrastructure may be limited, cardiac MRI plays an increasingly crucial role in patients with SCA. While access to advanced diagnostic tools can be challenging, cardiac MRI provides a noninvasive and comprehensive assessment of cardiac structure and function, aiding in the identification of underlying pathologies. Its ability to pinpoint reversible conditions, such as ischemic heart disease, myocarditis, or Chagas CMP, can be particularly valuable when treatment decisions are constrained by resource availability. Additionally, cardiac MRI can assist in risk stratification and guide therapeutic strategies, making it a promising tool to improve patient outcomes and reduce the burden of SCA in resource-limited settings (29).
It is important to highlight that the primary focus of this review was cardiac MRI examinations in patients who survived SCA. MRI performed postmortem was not included, although such imaging plays a pivotal role in advancing our understanding of SCA. Postmortem cardiac MRI offers invaluable insights into the complex interplay of cardiac pathology; contributes to the establishment of a more comprehensive standard of truth; and provides an unparalleled opportunity to visualize cardiac structures, identify anomalies, assess tissue characteristics, and investigate potential arrhythmogenic substrates. By examining myocardial infarctions, fibrosis, hypertrophic cardiomyopathies, and other structural abnormalities, postmortem cardiac MRI enables clinicians to pinpoint pathologic changes that may have precipitated SCA (30). Furthermore, the noninvasive nature of cardiac MRI minimizes the ethical concerns associated with postmortem studies and can facilitate the identification of SCA-related risk factors (31,32). Incorporating postmortem cardiac MRI data into SCA research is paramount, as it not only enhances the accuracy of cause-of-death determinations but also guides the development of effective prevention and intervention strategies, ultimately striving to reduce the burden of SCA in our communities.
This systematic review was intended to focus specifically on the role of cardiac MRI after SCA and to provide only a brief overview of its application in the field of cardiology. In discussing the findings of this systematic review, it is imperative to acknowledge the limitations identified. Notably, the majority of the included studies contained only descriptive characteristics regarding the diagnostic value of cardiac MRI after survival of SCA. In 11 of 14 studies, the comparison between the index test (ie, cardiac MRI) and other clinical-diagnostic standards, such as TTE or a combination of clinical imaging, ECG, and coronary angiography, is missing. Therefore, the rating in the Newcastle-Ottawa scale regarding selection of the nonexposed cohort and comparability was low because the potential diagnostic superiority of cardiac MRI over TTE, for example, was not directly investigated. In addition, this review had a relevant nonnegligible risk regarding patient selection bias. Even the studies presented here, which were most often purely descriptive, were difficult to compare with each other because some study protocols included all patients with SCA (8,14,17,18), whereas others included only patients with planned implantable cardioverter-defibrillator placement (7,12,33) or with nonischemic CMP (16,19,20). Additional noteworthy constraints encompassed the omission of pediatric patients, defined as younger than 18 years. This significantly narrows the scope of the review, potentially overlooking unique aspects of cardiomyopathies in the pediatric population. The restriction to English- and German-language studies introduces the possibility of language bias, potentially excluding valuable research conducted in other languages. The potential for patient overlap among studies with common authors and institutions raises considerations, despite efforts to cross-reference inclusion criteria and study populations. Most studies lacked randomization, limiting the internal validity of conclusions, and the absence of relevant comparators hinders definitive conclusions about the diagnostic accuracy of cardiac MRI. The heterogeneity in study designs prevented meaningful meta-analysis, limiting the ability of this review to provide a quantitative summary of evidence.
Finally, the analysis of existing data on cardiac MRI for SCA reveals a notable heterogeneity that presently impedes definitive conclusions about the additive value of cardiac MRI in this critical population. We propose a constructive pathway forward for future research in the secondary assessment of patients after cardiac arrest using cardiac MRI. It is imperative to recognize the need for standardized approaches in future studies. To address the existing heterogeneity, we recommend establishing consensus guidelines for imaging timing, study protocols, and the inclusion of key cardiac MRI findings, such as late gadolinium enhancement and myocardial edema, to ensure a uniform and comparable data set across studies. This harmonization will not only enhance the interpretability of results but also facilitate the aggregation of data for robust meta-analyses. Moreover, given the complexities of postcardiac arrest physiology, it is essential to consider potential confounding variables in study design. For instance, delineating myocardial edema resulting from the resuscitation process from other pathologic edematous states will be pivotal in refining the specificity of cardiac MRI findings.
In conclusion, this systematic review underscores the growing clinical value of cardiac MRI in the context of SCA evaluation. By synthesizing the findings from 14 studies involving 1367 individuals, we observed that cardiac MRI has the potential to make substantial contributions to clinical decision-making. It may lead to the identification of new diagnoses, reveal crucial pathologic or arrhythmogenic substrates, and help detect potentially reversible myocardial edema. Additionally, cardiac MRI offers insights into the occurrence of adverse events and provides prognostic information through functional markers and ventricular dimensions. However, the variability in reported findings and the absence of standardized comparators to cardiac MRI pose challenges. Furthermore, the review highlights the need to address patient selection bias. Nonetheless, the findings of this study demonstrate that the use of cardiac MRI after resuscitation shows promise as a valuable tool for enhancing treatment planning in cases of unclear SCA etiology.
B.S. and E.B. contributed equally to this work.
Authors declared no funding for this work.
Disclosures of conflicts of interest: B. Scharinger No relevant relationships. E.B. No relevant relationships. R.R. No relevant relationships. S.H. No relevant relationships. S.W. No relevant relationships. T.W. No relevant relationships. M.L. Lecture payments from Bayer, Novo Nordisk, Novartis, and Boehringer Ingelheim; meeting and/or travel support from Bayer and Pfizer. U.C.H. No relevant relationships. K.H. No relevant relationships. B.W. No relevant relationships. B. Strohmer No relevant relationships. R.K. No relevant relationships.
Abbreviations:
- CMP
- cardiomyopathy
- ECG
- electrocardiography
- SCA
- sudden cardiac arrest
- TTE
- transthoracic echocardiography
References
- 1. Tamis-Holland JE , Jneid H , Reynolds HR , et al . Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association . Circulation 2019. ; 139 ( 18 ): e891 – e908 . [DOI] [PubMed] [Google Scholar]
- 2. Rabbat MG , Kwong RY , Heitner JF , et al . The Future of Cardiac Magnetic Resonance Clinical Trials . JACC Cardiovasc Imaging 2021. ; 15 : 2127 – 2138 . [DOI] [PubMed] [Google Scholar]
- 3. European Heart Rhythm Association; Heart Rhythm Society ; Zipes DP , et al . ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) . J Am Coll Cardiol 2006. ; 48 ( 5 ): e247 – e346 . [DOI] [PubMed] [Google Scholar]
- 4. Al-Khatib SM , Stevenson WG , Ackerman MJ , et al . 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society . Heart Rhythm 2018. ; 15 ( 10 ): e190 – e252 . [Published correction appears in Heart Rhythm 2018;15(11):e278–e281.] [DOI] [PubMed] [Google Scholar]
- 5. Hayashi M , Shimizu W , Albert CM . The spectrum of epidemiology underlying sudden cardiac death . Circ Res 2015. ; 116 ( 12 ): 1887 – 1906 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nolan JP , Sandroni C , Böttiger BW , et al . European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care . Intensive Care Med 2021. ; 47 ( 4 ): 369 – 421 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zorzi A , Mattesi G , Baldi E , et al . Prognostic Role of Myocardial Edema as Evidenced by Early Cardiac Magnetic Resonance in Survivors of Out-of-Hospital Cardiac Arrest: A Multicenter Study . J Am Heart Assoc 2021. ; 10 ( 22 ): e021861 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Neilan TG , Farhad H , Mayrhofer T , et al . Late gadolinium enhancement among survivors of sudden cardiac arrest . JACC Cardiovasc Imaging 2015. ; 8 ( 4 ): 414 – 423 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Page MJ , McKenzie JE , Bossuyt PM , et al . The PRISMA 2020 statement: an updated guideline for reporting systematic reviews . BMJ 2021. ; 372 ( 71 ): n71 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Campbell M , McKenzie JE , Sowden A , et al . Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline . BMJ 2020. ; 368 : l6890 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wells G , Shea B , O'Connell D , et al . The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses . Ottawa, Canada: : Ottawa Health Research Institute; , 2000. . [Google Scholar]
- 12. van der Lingen ACJ , Becker MAJ , Kemme MJB , et al . Reversible Cause of Cardiac Arrest and Secondary Prevention Implantable Cardioverter Defibrillators in Patients With Coronary Artery Disease: Value of Complete Revascularization and LGE-CMR . J Am Heart Assoc 2021. ; 10 ( 8 ): e019101 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baritussio A , Zorzi A , Ghosh Dastidar A , et al . Out of hospital cardiac arrest survivors with inconclusive coronary angiogram: Impact of cardiovascular magnetic resonance on clinical management and decision-making . Resuscitation 2017. ; 116 : 91 – 97 . [DOI] [PubMed] [Google Scholar]
- 14. White JA , Fine NM , Gula L , et al . Utility of cardiovascular magnetic resonance in identifying substrate for malignant ventricular arrhythmias . Circ Cardiovasc Imaging 2012. ; 5 ( 1 ): 12 – 20 . [DOI] [PubMed] [Google Scholar]
- 15. Baritussio A , Biglino G , Scatteia A , et al . Long-term outcome of myocardial scarring and deformation with cardiovascular magnetic resonance in out of hospital cardiac arrest survivors . Eur Heart J Cardiovasc Imaging 2021. ; 22 ( 10 ): 1149 – 1156 . [DOI] [PubMed] [Google Scholar]
- 16. Rodrigues P , Joshi A , Williams H , et al . Diagnosis and Prognosis in Sudden Cardiac Arrest Survivors Without Coronary Artery Disease: Utility of a Clinical Approach Using Cardiac Magnetic Resonance Imaging . Circ Cardiovasc Imaging 2017. ; 10 ( 12 ): e006709 . [DOI] [PubMed] [Google Scholar]
- 17. Swoboda PP , Kidambi A , Uddin A , et al . The utility of cardiovascular magnetic resonance in the investigation of aborted sudden cardiac death . J Cardiovasc Magn Reson 2014. ; 16 ( S1 ): O31 . [Google Scholar]
- 18. Zorzi A , Susana A , De Lazzari M , et al . Diagnostic value and prognostic implications of early cardiac magnetic resonance in survivors of out-of-hospital cardiac arrest . Heart Rhythm 2018. ; 15 ( 7 ): 1031 – 1041 . [DOI] [PubMed] [Google Scholar]
- 19. Zaremba T , Brøndberg AK , Jensen HK , Kim WY . Cardiac magnetic resonance characteristics in young survivors of aborted sudden cardiac death . Eur J Radiol 2018. ; 105 : 141 – 147 . [DOI] [PubMed] [Google Scholar]
- 20. Kim SM , Youn CS , Lee GT , et al . Cardiac Magnetic Resonance Imaging for Nonischemic Cardiac Disease in Out-of-Hospital Cardiac Arrest Survivors Treated with Targeted Temperature Management: A Multicenter Retrospective Analysis . J Clin Med 2021. ; 10 ( 4 ): 794 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Soar J , Böttiger BW , Carli P , et al . European Resuscitation Council Guidelines 2021: Adult advanced life support . Resuscitation 2021. ; 161 : 115 – 151 . [Published correction appears in Resuscitation 2021;167:105-106.] [DOI] [PubMed] [Google Scholar]
- 22. Conte G , Belhassen B , Lambiase P , et al . Out-of-hospital cardiac arrest due to idiopathic ventricular fibrillation in patients with normal electrocardiograms: results from a multicentre long-term registry . Europace 2019. ; 21 ( 11 ): 1670 – 1677 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gandjbakhch E , Redheuil A , Pousset F , Charron P , Frank R . Clinical Diagnosis, Imaging, and Genetics of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: JACC State-of-the-Art Review . J Am Coll Cardiol 2018. ; 72 ( 7 ): 784 – 804 . [DOI] [PubMed] [Google Scholar]
- 24. Dumont CA , Monserrat L , Soler R , et al . Interpretation of electrocardiographic abnormalities in hypertrophic cardiomyopathy with cardiac magnetic resonance . Eur Heart J 2006. ; 27 ( 14 ): 1725 – 1731 . [DOI] [PubMed] [Google Scholar]
- 25. Casella M , Gasperetti A , Sicuso R , et al . Characteristics of Patients With Arrhythmogenic Left Ventricular Cardiomyopathy: Combining Genetic and Histopathologic Findings . Circ Arrhythm Electrophysiol 2020. ; 13 ( 12 ): e009005 . [DOI] [PubMed] [Google Scholar]
- 26. Scatteia A , Dellegrottaglie S . Cardiac magnetic resonance in ischemic cardiomyopathy: present role and future directions . Eur Heart J Suppl 2023. ; 25 ( Suppl C ): C58 – C62 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ferreira VM , Schulz-Menger J , Holmvang G , et al . Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations . J Am Coll Cardiol 2018. ; 72 ( 24 ): 3158 – 3176 . [DOI] [PubMed] [Google Scholar]
- 28. Ojrzyńska-Witek N , Marczak M , Mazurkiewicz Ł , et al . Sudden cardiac arrest: Focus on cardiac magnetic resonance . Kardiol Pol 2022. ; 80 ( 1 ): 87 – 89 . [DOI] [PubMed] [Google Scholar]
- 29. Marçal PC , Braggion-Santos MF , Wada DT , et al . Cardiac Magnetic Resonance as an Etiological Diagnosis Tool in Recovered Sudden Cardiac Death or Unstable Ventricular Arrhythmia Patients . Arq Bras Cardiol 2023. ; 120 ( 4 ): e20220411 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Aquaro GD , Guidi B , Emdin M , et al . Post-Mortem Cardiac Magnetic Resonance in Explanted Heart of Patients with Sudden Death . Int J Environ Res Public Health 2022. ; 19 ( 20 ): 13395 . [Published correction appears in Int J Environ Res Public Health 2023;20(9):5734.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jackowski C , Schwendener N , Grabherr S , Persson A . Post-mortem cardiac 3-T magnetic resonance imaging: visualization of sudden cardiac death? J Am Coll Cardiol 2013. ; 62 ( 7 ): 617 – 629 . [DOI] [PubMed] [Google Scholar]
- 32. Puranik R , Gray B , Lackey H , et al . Comparison of conventional autopsy and magnetic resonance imaging in determining the cause of sudden death in the young . J Cardiovasc Magn Reson 2014. ; 16 ( 1 ): 44 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schober AL , Jungbauer C , Poschenrieder F , et al . Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention . J Clin Med 2021. ; 10 ( 21 ): 4980 . [DOI] [PMC free article] [PubMed] [Google Scholar]