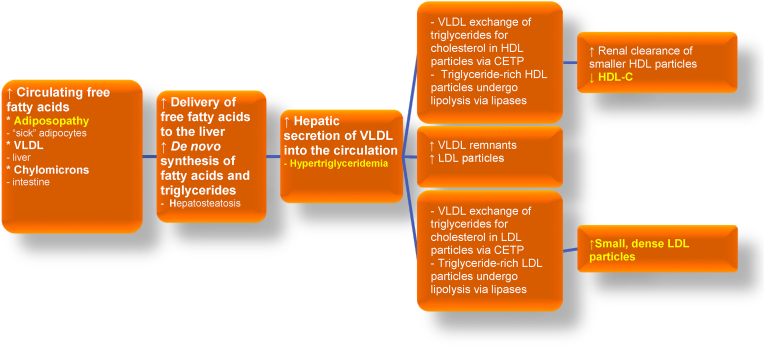
Fig. 9.
Adiposopathic dyslipidemia: Excess adiposity can contribute to hypertriglyceridemia, reduced blood HDL-C levels, and elevated smaller and more dense LDL particles. Terms that are similar to “adiposopathic dyslipidemia” include “atherogenic dyslipidemia” and/or “diabetes dyslipidemia,” all intended to reflect a lipid pattern found in many patients with obesity, as well as patients with type 2 diabetes mellitus and/or MASLD [137]. The origins of free fatty acid delivery to the liver include lipolysis of triglyceride-rich lipoproteins (e.g., VLDL originally from the liver and chylomicrons from the intestine), as well as the adiposopathic flux of fatty acids from adipose tissue as the result of insulin resistance. Finally, obesity can be associated with increased de novo synthesis of fatty acids [86]. A substantial contributor to adiposopathic dyslipidemia is CETP, which facilitates exchange of triglyceride and cholesteryl esters among circulating lipoproteins. CETP is increased with obesity, which may enhance the exchange of triglyceride from VLDL for cholesteryl esters from HDL. Similarly, CETP may facilitate the exchange of triglycerides from VLDL for cholesteryl esters in LDL. The action of body lipases on triglyceride-rich HDL particles results in smaller HDL particles that are more easily metabolized by the liver and kidney, resulting in reduced blood HDL-C levels. The action of body lipases on triglyceride-rich LDL particles results in smaller, more dense LDL particles. (Figure adapted with permission from Bays HE et al. Obesity Algorithm Slides, presented by the Obesity Medicine Association. www.obesityalgorithm.org. 2020). CETP: cholesteryl ester transfer protein; HDL-C: high-density lipoprotein cholesterol; LDL: low-density lipoprotein; MASLD: metabolic dysfunction-associated steatotic liver disease; VLDL: very-low-density lipoprotein.