Abstract
Purpose
Adequate adjustment to bodily changes during various phases of cancer treatment is important to patients’ emotional well-being. The Body Image Scale (BIS) is a widely used tool for assessment of body image concerns in different cancer types. However, a cut-point score indicative of clinically relevant body image concerns has not been established. The purpose of our study was to evaluate whether the previously suggested, but not validated, BIS cut-point score of ≥10 is an adequate indicator of psychological distress.
Methods
In a prospective cross-sectional study, 590 adult patients were recruited from a psychiatric oncology clinic (November 2017-March 2018). Patient-reported body image concerns, depression, anxiety, and emotional distress were assessed with the BIS, Patient Health Questionnaire-9, Generalized Anxiety Disorder Scale-7, and National Comprehensive Cancer Network Distress Thermometer, respectively.
Results
Almost half of the patients had a BIS score ≥10; these were more likely to be younger, female, Hispanic, and to have breast cancer than patients with a score <10. BIS scores were positively associated with depression, anxiety, and distress scores. A BIS score ≥10 was a significant predictor of moderate depression and anxiety (odds ratios= 3.555 [95% CI 2.478-5.102] and 3.655 [2.493-5.358]; p<0.001 for both).
Conclusion
To our knowledge, this is the first study to have assessed the validity of the previously suggested clinically relevant BIS cut-point score of ≥10 as an indicator of psychological distress. Our results suggest that a BIS score of ≥10 or higher should lead to follow-up on body image concerns and/or appropriate referral.
Keywords: Anxiety, body image, cancer, depression, distress, physical appearance
Introduction
In chronic illness, subjective evaluations of and emotional responses to bodily changes are influenced by perception of comfort secondary to altered sensory experience, evaluation of competence based on functional ability, assessment of appearance changes, and predictability of the physical change over time [1].Specific to the oncology setting, the diagnosis and treatment of cancer lead to various bodily changes, which include both physical and functional changes. These changes can be general, such as hair loss, nail discoloration, and weight loss/gain, or very specific, such as loss of a limb or breast, or need for a colostomy bag. As a result, patients are constantly adapting to bodily changes, both in the immediate postoperative phase [2] and in survivorship [3]. However, such adaptation can be difficult, sometimes associated with low mood or anxiety [4-6] and other times associated with problems in sexual functioning [7,8] or poor quality of life [9,10]. Body image concerns and adaptation may vary across different cancers [11,3,10]. Thus, body image adaptation is a vital aspect of cancer and the cancer treatment trajectory that deserves attention from the health professional.
While adjustment to body image is an important aspect of the cancer treatment trajectory, it may be difficult to assess body image concerns. Tools to assess body image may not capture all the dimensions of body image, and most tools are designed for a specific cancer type only [12-14]. The Body Image Scale (BIS) is widely used to assess body image concerns across different types of cancer [15]. The BIS is a brief questionnaire that yields a score on a continuous scale after summing all items. However, there is no information available on what cut-off value should warrant an alert for the clinicians [15]. Based on clinical experience, Hopwood and colleagues [16] considered a sum score of 10 or greater as an indicator of body image concerns. This cut-point has been used in a few studies [16-18]; however, it has not been validated as a clinically relevant threshold for body image concerns in cancer patients.
An additional limitation in our current understanding of body image concerns in cancer patients is their relation to psychological distress. Body image concerns are conceptualized from a cognitive behavioral perspective [19,20]. From the cognitive behavioral standpoint, interaction of the individual with the environment triggers emotional and behavioral consequences based on the individual’s appearance schema. Another helpful model is to consider body image concerns on a spectrum: some cancer patients may have no concerns about the bodily changes, while others may experience a severe degree of body image concerns, which may interfere with their functioning [21]. According to the body image continuum model, patients with severe body image concerns may experience psychosocial problems such as social withdrawal, depression, anxiety, or difficulty adjusting to expectancy outcomes [21]. Although studies have assessed association between body image and psychological distress in populations with specific cancer types [22,23,4,24], few studies have focused on populations with diverse cancer types, and these have been specific to various phases of cancer treatment, such as patients with advanced disease [18], cancer survivors [25], and newly diagnosed cancer patients [26]. Most of these studies assessed psychological distress broadly; one study instead evaluated the effect of hope (positive emotion) on body image. Finally, the diverse tools used to evaluate body image concerns make comparison between the studies difficult.
To address these limitations in the assessment of body image and its association with psychological distress, we here report the results of a prospective cross-sectional study that included patients with a wide variety of cancer diagnoses seen at a psychiatric oncology clinic. The objective of the study was to assess whether a cut-point score of ≥10 on the BIS, is an adequate indicator of psychological distress.
Methods
Sample, setting, and study design
Adult patients (N=590) with a history of cancer diagnosis seen in an outpatient psychiatric oncology clinic (November 2017-March 2018) were approached for the study. The study population partially overlaps a previously reported sample evaluated for demoralization and depression [27]. Patient-reported data were collected as a part of routine clinical evaluation, but prior to the clinic visit patients provided informed consent for their data to be used for research purposes. Only patients who provided informed consent were included in the current analyses. Patients who refused to participate including their reason for refusal was not tracked. Similarly, whether consecutive patients were approached was not recorded.
The outpatient psychiatric oncology clinic is part of the main cancer hospital at an academic medical center, and patients are referred for evaluation of depression, anxiety, coping, substance use, and body image concerns. After the initial consultation by a psychiatrist, patients were followed up per their clinical situation. The data used for the current report were thus taken from either the initial consultation evaluation or from one of the subsequent visits.
Inclusion Criteria
Patients presenting to the psychiatric oncology clinic were considered eligible for inclusion if they were 21 years or older and if they had received treatment or were in active treatment for a cancer diagnosis. There were no other inclusion/exclusion criteria.
Ethical Approval Statement
The Institutional Review Board approved the study (protocol number PA14-0265), and all patients provided written informed consent.
Measures
Body image:
The Body Image Scale (BIS) was used for the assessment of body image concerns [15]. The BIS is a 10-item questionnaire with a score that ranges from 0 to 30. Items ask about the respondent’s perceptions (regarding, for example, physical and sexual attractiveness, femininity/masculinity, and self-consciousness about the body), level of dissatisfaction regarding the treatment effects (for example, feeling that treatment has left their body less whole and dissatisfaction with the treatment scar, and thoughts about their body when clothed), and presence of avoidance behavior related to the bodily changes. The items are scored 0 through 3, where 0=not at all, 1=a little, 2=quite a bit, and 3=very much, and a “not applicable” option is only available for the question about the effect of a scar. Item-scores are summed to compute a BIS sum-score, whereby “not applicable” answers for the scar-item were scored as 0. Patients saw both the value and the label when they filled out the scale in the study. Higher scores are associated with higher body image concerns [15]. The BIS has satisfactory structural validity for a single dimension, good internal consistency (Cronbach’s α=0.86-0.96), and fair test-retest reliability (1 month, 0.70) [28,29]. In our study, the BIS had good internal consistency (Cronbach’s α=0.927).
Depression:
The Patient Health Questionnaire-9 (PHQ-9) was used to evaluate depressive symptoms [30]. The PHQ-9 is a reliable and validated scale for assessment of depression per Diagnostic Statistical Manual IV criteria and includes nine items with a sum-score range from 0 to 27. Established cut-offs of 5, 10, 15, and 20 are indicative of mild, moderate, moderately severe, and severe depression, respectively [30,31]. The PHQ-9 was shown to have good reliability in a large sample of cancer patients (Cronbach’s α = 0.84) [32].
Anxiety:
The Generalized Anxiety Disorder scale-7 (GAD-7) was used to assess anxiety symptoms. The GAD-7 is a validated 7-item scale developed for evaluation of presence and severity of generalized anxiety disorder in clinical settings [33]. The sum score ranges from 0 to 21, with cut-offs of 5, 10, and 15 indicative of mild, moderate, and severe anxiety, respectively [33]. The scale has good psychometric properties, with Cronbach’s alpha values for internal consistency between 0.89 and 0.92 and excellent convergent reliability as indicated by strong correlations with other anxiety questionnaires (0.72-0.74) [33,34].
Distress:
The National Comprehensive Cancer Network (NCCN) Distress Thermometer (DT) is a validated, brief, quick screening tool for psychosocial distress in cancer patients, with a score range from 0 to 10 [35]. A distress score of 4 or more warrants further evaluation tailored based on the items checked on the problem list [35].
Statistical Analyses:
All analyses were performed using IBM SPSS software version 24. Descriptive statistics were used for demographic and medical characteristics of the sample. Scatterplots were inspected for linearity of the associations between the BIS and measures of psychological distress.
Pearson’s r correlations were calculated to evaluate the relationship between body image concerns and measures of psychological distress. To examine the clinical validity of the BIS cut-off ≥10, means plots were created to visualize how this cut-point was associated with established cut-points on the PHQ-9, GAD-7, and DT. In addition, for the two subgroups of patients with scores below and above the suggested BIS cut-off, scores on the PHQ-9, GAD-7, and DT were compared using independent t-tests. Lastly, binary logistic regression models were calculated with moderate depression and anxiety as outcomes and BIS category as the predictor variable; age, sex, race/ethnicity, and cancer type were included as covariates. A p value of <0.05 was considered statistically significant.
Results
Sample characteristics
590 patients consented and were included in the study. Included patients were 54.3±12.9 (M±SD) years old, and the majority were female (69%), white (74%), and in a relationship (66%) [Table 1]. The most common cancer types were breast (36%), hematological (21%), and gastrointestinal (10%). In this sample, the mean BIS score was 9.3, and the mean PHQ-9 and GAD-7 scores were 8.5 and 7.3, respectively, indicative of mild depression and mild anxiety [Table 2].
Table 1.
Patient characteristics for the complete sample and for the groups with low vs. high BIS scores.
| Variable | N/% or Mean (SD) | p Value | ||
|---|---|---|---|---|
| Full Sample (N=590) | BIS <10 (N=345) | BIS ≥10 (N=245) | ||
| Age (years) | 54.3 (12.9) | 56.25 (13.31) | 51.66 (12.0) | <0.001 |
| Sex | <0.001 | |||
| Female | 409/69 | 219/63 | 190/78 | |
| Male | 181/31 | 126/37 | 55/22 | |
| Race | 0.001 | |||
| White | 438/74 | 270/78 | 168/69* | |
| Black | 71/12 | 34/10 | 37/15 | |
| Hispanic | 64/11 | 27/8 | 37/15* | |
| Othera | 17/3 | 14/4 | 3/1* | |
| Relationship | 0.634 | |||
| In a relationshipb | 387/66 | 229/66 | 158/65 | |
| Not in a relationshipc | 203/34 | 116/34 | 87/36 | |
| Cancer Type | <0.001d | |||
| Breast | 214/36 | 103/30 | 111/45 | |
| Hematological | 125/21 | 89/23 | 46/19 | |
| Gastrointestinal | 58/10 | 39/11 | 19/8 | |
| Genitourinary | 37/6 | 26/8 | 11/4 | |
| Head Neck Face | 33/6 | 23/7 | 10/4 | |
| Brain | 30/5 | 19/6 | 11/4 | |
| Gynecology | 27/5 | 15/4 | 12/5 | |
| Skin | 26/5 | 13/4 | 14/6 | |
| Lung | 15/2 | 11/3 | 4/2 | |
| Other | 12/2 | 7/2 | 5/2 | |
| Endocrine | 12/2 | 10/3 | 2/1 | |
| Treatment status | 0.244 | |||
| Patiente | 272/46 | 166/48 | 106/43 | |
| Survivorf | 318/54 | 179/52 | 139/57 | |
Including Asian (n=12), ‘other’ (n=3), American Indian (n=1), and not reported (n=1).
Including married (N=380), significant other (n=5), and together (n=2).
Including single (n=104), divorced (n=68), widowed (n=23), separated (n=4), and other/unknown (4).
Comparing breast cancer vs. other diagnoses combined.
active disease undergoing any treatment, including n=4 with active disease pending treatment onset.
completion of all primary treatment and currently no evidence of disease/in remission.
Statistically significant difference between BIS groups at p<0.05.
Table 2.
Sum scores on the BIS, PHQ-9, GAD-7, and DT for the complete sample and for the groups with low vs. high BIS scores (PHQ, GAD, and DT only). P values indicate t-test comparisons between BIS <10 and BIS ≥10.
| Scale | Full Sample (N=590) | BIS <10 (N=345) | BIS≥10 (N=245) | p Value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| BIS | 9.28 | 7.78 | |||||
| PHQ-9 | 8.49 | 5.65 | 6.77 | 5.17 | 10.9 | 5.41 | <0.001 |
| GAD-7 | 7.27 | 5.69 | 5.51 | 5.07 | 9.74 | 5.59 | <0.001 |
| DT | 4.38 | 3.01 | 3.50 | 2.90 | 5.63 | 2.70 | <0.001 |
Using the BIS cut-point of 10, 42% of patients had a BIS score suggested to be of clinical relevance [Table 1].
Body Image Scale
Patients with a BIS score ≥10 were younger (t(588)=4.299, p <0.001), more often female (X2(1)=13.34, p <0.001), and less likely to be white and more likely to identify as Hispanic (Χ2(3)=16.073, p=0.001). These patients were also more likely to be breast cancer patient (vs. other cancer-site) (Χ2(1)=14.796, p<0.001). No other comparisons yielded significant results [Table 1].
Higher sum scores on the BIS were significantly correlated with more severe depression (r=.44, p <.0001), anxiety (r=.44, p <.0001), and distress (r=.41, p <.0001).
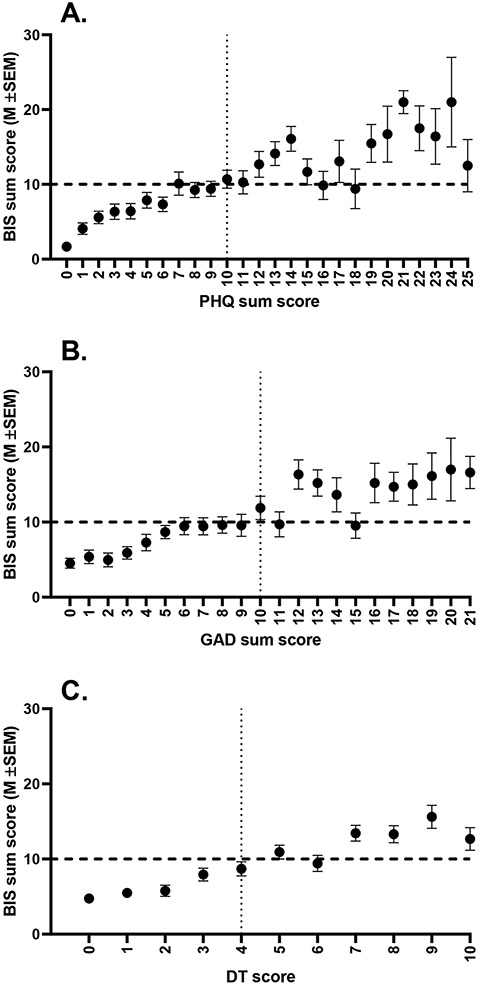
Means plots (Figure 1) indicated that a cut-point of ≥10 on the BIS distinguished moderate depression from mild depression, moderate anxiety from mild anxiety, and clinically relevant distress from not clinically relevant distress. Indeed, mean scores for depression, anxiety, and distress were significantly higher in patients with a BIS score ≥10 and corresponded with the established cut-points for moderate depression (PHQ ≥10), moderate anxiety (GAD ≥10), and clinically relevant distress (DT ≥4) [Table 2]. Furthermore, results of log linear regression models correcting for age, sex, and race/ethnicity indicated that having a BIS score ≥10 was significantly associated with a higher chance of having moderate depression or anxiety [Table 3]
Figure 1.
Means plots depicting BIS sum scores (mean ± SEM) in relation to sum scores on the PHQ-9 [A], GAD-7 [B], and DT [C]. Bold dotted lines indicate the suggested cut-off of 10 on the BIS; thin dotted lines indicate the suggested cut-offs for moderately severe depression [A], moderate anxiety [B], and clinically relevant distress [C].
Table 3.
Logistic regression models for BIS <10 vs. BIS ≥10 predicting moderately severe depression (Model 1) or moderate anxiety (Model 2). Age, sex, race, and cancer type (breast vs. other) were included as covariates.
| Model 1. Moderately severe depression (PHQ-9 ≥10) as dependent variable | |||||
|---|---|---|---|---|---|
| Variable | B | S.E. | Exp(B) | 95% CI for Exp(B) | p Value |
| Age | 0.001 | 0.007 | 1.001 | 0.987 – 1.015 | 0.89 |
| Sexa | 0.036 | 0.221 | 1.036 | 0.672 – 1.597 | 0.87 |
| Raceb | 0.363 | 0.203 | 1.438 | 0.966 – 2.139 | 0.073 |
| Cancer type c | 0.282 | 0.212 | 1.326 | 0.874 – 2.010 | 0.19 |
| BIS d | 1.268 | 0.184 | 3.555 | 2.478 – 5.102 | <0.001 |
| Constant | −1.319 | 0.444 | 0.267 | 0.003 | |
| Model 2. Moderate anxiety (GAD-7 ≥10) as dependent variable | |||||
| Age | −0.001 | 0.008 | 0.999 | 0.985 – 1.015 | 0.94 |
| Sexa | −0.649 | 0.244 | 0.522 | 0.324 – 0.843 | 0.008 |
| Raceb | 0.686 | 0.210 | 1.985 | 1.314 – 2.997 | 0.001 |
| Cancer type c | 0.384 | 0.221 | 1.468 | 0.953 – 2.263 | 0.082 |
| BIS d | 1.296 | 0.195 | 3.655 | 2.493 – 5.358 | <0.001 |
| Constant | −1.620 | 0.481 | 0.198 | 0.001 | |
Female is reference.
White is reference.
Breast cancer is reference.
BIS score <10 is reference.
Discussion
In this study, we evaluated the value of a previously suggested BIS cut-off score of ≥10 as an indicator of psychological distress and found that 42% of the patients in our sample had body image concerns meeting this cutoff. Those with a BIS score ≥10 were three and a half times more likely to have moderate depression and/or moderate anxiety, even after adjustment for age, sex, and race/ethnicity. Establishing the relevance of a BIS cut-off score in relation to moderate psychological distress will help clinicians to identify the extent of body image concerns more effectively, thus enabling early identification of the problem and offering of appropriate treatment in a timely fashion.
Comparisons of our results with other mixed-cancer sample studies [18,25,26] are limited by the use of different tools. Nonetheless, our results are consistent with and extend the findings of Rhondali et al[18] who compared advanced cancer patients with low and high BIS scores (<10 and ≥10, respectively) using different measures of psychological distress, i.e. the Hospital Anxiety and Depression Scale (HADS) and Edmonton Symptom Assessment System (ESAS). They found that a BIS cut-point of ≥10 distinguished patients with normal to borderline clinical depression and anxiety from those with borderline to abnormal ranges of depression and anxiety [18]. In our study, since depression and anxiety symptoms were a subset of the psychological distress measures we were able to extend the valuable findings of the HADS scale and replicate the positive association between higher body image concern and moderate depression and moderate anxiety with the help of clinically validated questionnaires. Additionally, we expand the findings of Rhondali et al. with the larger sample size in our report. Similarly, DeFrank and colleagues found an association between body image and general mental health concerns [25]. Unlike Rhondali et al., we assessed psychosocial distress with the DT, but found a similar positive association between psychosocial distress and higher body image score. Our results differ from Rhondali et al in that our average BIS score was slightly lower than noted in their study [18]. Patients in our study sample were at various stages of cancer treatment, whereas their study population consisted of advanced cancer patients only, potentially explaining the lower degrees of symptom burden and corresponding body image concerns in our sample.
Our results differ from Rhondali et al, in that our average BIS score was slightly lower than noted in their study [18]. Patients in our study sample were either receiving cancer treatment or had completed cancer treatment, which is different from their study population of advanced cancer patients who had completed their cancer treatment, potentially explaining the variability in symptom burden and corresponding body image concerns in our sample. Our results differ from those of Liu et al in that our mean BIS score was higher than that of their group of newly diagnosed cancer patients[26].
This difference is, again, likely because our sample was representative of patients who were in different phases of cancer treatment.
The association of body image concerns with depression and anxiety remained significant after adjusting for age, sex, and race/ethnicity. This emphasizes the importance of body image concerns are prominent not only in younger patients with cancer [11], but also in older patients with cancer [36], and our data suggest that psychological distress as a result of body image concerns will be seen in both age groups. Similarly, concerns related to body image should be considered in both sexes although their bodily concerns may vary due to the specific cancer type but these concerns could easily go unrecognized. Limited studies have evaluated the adjustment to physical changes in oncology among different ethnic minorities[37]. Our results highlight the need to evaluate body image concerns in more detail in such groups.
The strengths of our study are a large sample size with the population not restricted to one specific type of cancer type or stage, and the use of validated instruments to assess body image, depression, anxiety, and distress. To our knowledge, this is the first study to assess the recommended cut-off score for BIS and evaluate the association with depression, anxiety, and distress in detail.
Limitations
Some limitations warrant mentioning. First, while our results suggest that body image concerns might differ between races or ethnicities, the majority of our sample was white, thereby limiting the interpretability of our results for other races and ethnicities. Second, since this was a cross-sectional study, causality of the relation between body image concerns and psychological distress cannot be established. Longitudinal studies are needed to clarify the trajectory of body image problems as a function of cancer treatment and their causal relation with psychological distress. Third, our study participants were recruited from a psychiatric oncology clinic where the reason for referral is psychiatric symptoms, so the data may not be representative of a general population of cancer patients. However, scores on the psychological distress measures did include the complete range of possible sum scores, thereby making this a valid data set to establish the validity of the BIS cut-off score in relation to psychological distress.
Conclusion and Clinical Implications
In summary, we showed that the clinically relevant cut-off score of ≥10 on the BIS is indeed associated with moderate depression and anxiety as well as with clinically relevant distress. This suggests that a score of ≥10 or more on the BIS should inform the health professional that follow-up on body image concerns is needed.
Acknowledgments:
We would like to acknowledge Sunita Patterson, for the editorial assistance with this manuscript.
Funding:
The Hackett Family provided funding for this research. Also supported by the National Institutes of Health/National Cancer Institute under award number P30CA016672 (used the Clinical Trials Office).
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board (protocol number PA14-0265) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.Vamos M (1993) Body Image in Chronic Illness--a Reconceptualization. International journal of psychiatry in medicine 23 (2):163–178. doi: 10.2190/bll4-eval-49y3-4g66 [DOI] [PubMed] [Google Scholar]
- 2.Dropkin MJ (1989) Coping with Disfigurement and Dysfunction after Head and Neck Cancer Surgery: A Conceptual Framework. Seminars in oncology nursing 5 (3):213–219 [DOI] [PubMed] [Google Scholar]
- 3.Falk Dahl CA, Reinertsen KV, Nesvold IL, Fossa SD, Dahl AA (2010) A Study of Body Image in Long-Term Breast Cancer Survivors. Cancer 116 (15):3549–3557. doi: 10.1002/cncr.25251 [DOI] [PubMed] [Google Scholar]
- 4.Ju HB, Kang EC, Jeon DW, Kim TH, Moon JJ, Kim SJ, Choi JM, Jung DU (2018) Associations among Plasma Stress Markers and Symptoms of Anxiety and Depression in Patients with Breast Cancer Following Surgery. Psychiatry investigation 15 (2):133–140. doi: 10.30773/pi.2017.07.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sherman KA, Woon S, French J, Elder E (2017) Body Image and Psychological Distress in Nipple-Sparing Mastectomy: The Roles of Self-Compassion and Appearance Investment. Psycho-Oncology 26 (3):337–345. doi: 10.1002/pon.4138 [DOI] [PubMed] [Google Scholar]
- 6.Bisseling KC, Kondalsamy-Chennakesavan S, Bekkers RL, Janda M, Obermair A (2009) Depression, Anxiety and Body Image after Treatment for Invasive Stage One Epithelial Ovarian Cancer. The Australian & New Zealand journal of obstetrics & gynaecology 49 (6):660–666. doi: 10.1111/j.1479-828X.2009.01074.x [DOI] [PubMed] [Google Scholar]
- 7.Reese JB, Finan PH, Haythornthwaite JA, Kadan M, Regan KR, Herman JM, Efron J, Diaz LA Jr., Azad NS (2014) Gastrointestinal Ostomies and Sexual Outcomes: A Comparison of Colorectal Cancer Patients by Ostomy Status. Support Care Cancer 22 (2):461–468. doi: 10.1007/s00520-013-1998-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hazewinkel MH, Laan ET, Sprangers MA, Fons G, Burger MP, Roovers JP (2012) Long-Term Sexual Function in Survivors of Vulvar Cancer: A Cross-Sectional Study. Gynecologic oncology 126 (1):87–92. doi: 10.1016/j.ygyno.2012.04.015 [DOI] [PubMed] [Google Scholar]
- 9.Boquiren VM, Esplen MJ, Wong J, Toner B, Warner E (2013) Exploring the Influence of Gender-Role Socialization and Objectified Body Consciousness on Body Image Disturbance in Breast Cancer Survivors. Psychooncology 22 (10):2177–2185. doi: 10.1002/pon.3271 [DOI] [PubMed] [Google Scholar]
- 10.Harrington JM, Badger TA (2009) Body Image and Quality of Life in Men with Prostate Cancer. Cancer Nurs 32 (2):E1–7. doi: 10.1097/NCC.0b013e3181982d18 [DOI] [PubMed] [Google Scholar]
- 11.Fingeret MC, Yuan Y, Urbauer D, Weston J, Nipomnick S, Weber R (2012) The Nature and Extent of Body Image Concerns among Surgically Treated Patients with Head and Neck Cancer. Psychooncology 21 (8):836–844. doi: 10.1002/pon.1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ (2001) Functional Outcome, Quality of Life, Body Image, and Cosmesis in Patients after Laparoscopic-Assisted and Conventional Restorative Proctocolectomy: A Comparative Study. Diseases of the colon and rectum 44 (12):1800–1807. doi: 10.1007/bf02234458 [DOI] [PubMed] [Google Scholar]
- 13.Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA (1998) Cosmesis and Body Image after Laparoscopic-Assisted and Open Ileocolic Resection for Crohn's Disease. Surgical endoscopy 12 (11):1334–1340 [DOI] [PubMed] [Google Scholar]
- 14.Dalton EJ, Rasmussen VN, Classen CC, Grumann M, Palesh OG, Zarcone J, Kraemer HC, Kirshner JJ, Colman LK, Morrow GR, Spiegel D (2009) Sexual Adjustment and Body Image Scale (Sabis): A New Measure for Breast Cancer Patients. The breast journal 15 (3):287–290. doi: 10.1111/j.1524-4741.2009.00718.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hopwood P, Fletcher I, Lee A, Al Ghazal S (2001) A Body Image Scale for Use with Cancer Patients. European journal of cancer (Oxford, England : 1990) 37 (2):189–197 [DOI] [PubMed] [Google Scholar]
- 16.Hopwood P, Lee A, Shenton A, Baildam A, Brain A, Lalloo F, Evans G, Howell A (2000) Clinical Follow-up after Bilateral Risk Reducing ('Prophylactic') Mastectomy: Mental Health and Body Image Outcomes. Psychooncology 9 (6):462–472 [DOI] [PubMed] [Google Scholar]
- 17.Graboyes EM, Hill EG, Marsh CH, Maurer S, Day TA, Sterba KR (2019) Body Image Disturbance in Surgically Treated Head and Neck Cancer Patients: A Prospective Cohort Pilot Study. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 161 (1):105–110. doi: 10.1177/0194599819835534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rhondali W, Chisholm GB, Filbet M, Kang DH, Hui D, Cororve Fingeret M, Bruera E (2015) Screening for Body Image Dissatisfaction in Patients with Advanced Cancer: A Pilot Study. J Palliat Med 18 (2):151–156. doi: 10.1089/jpm.2013.0588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White CA (2000) Body Image Dimensions and Cancer: A Heuristic Cognitive Behavioural Model. Psychooncology 9 (3):183–192 [DOI] [PubMed] [Google Scholar]
- 20.Donald A Williamson TMS, Marney A White, Emily York-Crowe. (2002) An Information-Processing Perspective on Body Image. In: Thomas F Cash TP (ed) Body Image. A Handbook of Theory, Research, and Clinical Practice. The Guilford Press, New York and London, pp 47–54 [Google Scholar]
- 21.Rhoten B (2018) Theoretical Foundations of Body Image. In: Michelle Cororve Fingeret IT (ed) Body Image Care for Cancer Patients:Principles and Practices. Oxford University Press, New York., pp 28–29 [Google Scholar]
- 22.Rhoten BA, Deng J, Dietrich MS, Murphy B, Ridner SH (2014) Body Image and Depressive Symptoms in Patients with Head and Neck Cancer: An Important Relationship. Support Care Cancer 22 (11):3053–3060. doi: 10.1007/s00520-014-2312-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saini A, Berruti A, Cracco C, Sguazzotti E, Porpiglia F, Russo L, Bertaglia V, Picci RL, Negro M, Tosco A, Campagna S, Scarpa RM, Dogliotti L, Furlan PM, Ostacoli L (2013) Psychological Distress in Men with Prostate Cancer Receiving Adjuvant Androgen-Deprivation Therapy. Urologic oncology 31 (3):352–358. doi: 10.1016/j.urolonc.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 24.Gomez-Campelo P, Bragado-Alvarez C, Hernandez-Lloreda MJ (2014) Psychological Distress in Women with Breast and Gynecological Cancer Treated with Radical Surgery. Psychooncology 23 (4):459–466 [DOI] [PubMed] [Google Scholar]
- 25.DeFrank JT, Mehta CC, Stein KD, Baker F (2007) Body Image Dissatisfaction in Cancer Survivors. Oncology nursing forum 34 (3):E36–41 [DOI] [PubMed] [Google Scholar]
- 26.Liu J, Griva K, Lim HA, Tan JYS, Mahendran R (2017) Longitudinal Study of the Protective Effect of Hope on Reducing Body Image Distress in Cancer Patients. Journal of psychosocial oncology 35 (1):77–89. doi: 10.1080/07347332.2016.1221490 [DOI] [PubMed] [Google Scholar]
- 27.Ignatius J, De La Garza R 2nd (2019) Frequency of Demoralization and Depression in Cancer Patients. General hospital psychiatry 60:137–140. doi: 10.1016/j.genhosppsych.2019.04.013 [DOI] [PubMed] [Google Scholar]
- 28.Annunziata MA, Giovannini L, Muzzatti B (2012) Assessing the Body Image: Relevance, Application and Instruments for Oncological Settings. Support Care Cancer 20 (5):901–907. doi: 10.1007/s00520-011-1339-x [DOI] [PubMed] [Google Scholar]
- 29.Melissant HC, Neijenhuijs KI, Jansen F, Aaronson NK, Groenvold M, Holzner B, Terwee CB, van Uden-Kraan CF, Cuijpers P, Verdonck-de Leeuw IM (2018) A Systematic Review of the Measurement Properties of the Body Image Scale (Bis) in Cancer Patients. Support Care Cancer 26 (6):1715–1726. doi: 10.1007/s00520-018-4145-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JBW (2001) The Phq-9: Validity of a Brief Depression Severity Measure. Journal of General Internal Medicine 16 (9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manea L, Gilbody S, McMillan D (2012) Optimal Cut-Off Score for Diagnosing Depression with the Patient Health Questionnaire (Phq-9): A Meta-Analysis. CMAJ : Canadian Medical Association Journal 184 (3):E191–E196. doi: 10.1503/cmaj.110829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hinz A, Mehnert A, Kocalevent RD, Brähler E, Forkmann T, Singer S, Schulte T (2016) Assessment of Depression Severity with the Phq-9 in Cancer Patients and in the General Population. BMC Psychiatry 16 (1). doi: 10.1186/s12888-016-0728-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JB, Lowe B (2006) A Brief Measure for Assessing Generalized Anxiety Disorder: The Gad-7. Archives of internal medicine 166 (10):1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 34.Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, Herzberg PY (2008) Validation and Standardization of the Generalized Anxiety Disorder Screener (Gad-7) in the General Population. Medical care 46 (3):266–274. doi: 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- 35.Holland JC, Bultz BD (2007) The Nccn Guideline for Distress Management: A Case for Making Distress the Sixth Vital Sign. JNCCN Journal of the National Comprehensive Cancer Network 5 (1):3–7 [PubMed] [Google Scholar]
- 36.Ayalon R, Bachner YG (2019) Medical, Social, and Personal Factors as Correlates of Quality of Life among Older Cancer Patients with Permanent Stoma. European journal of oncology nursing : the official journal of European Oncology Nursing Society 38:50–56. doi: 10.1016/j.ejon.2018.11.010 [DOI] [PubMed] [Google Scholar]
- 37.Christie KM, Meyerowitz BE, Maly RC (2010) Depression and Sexual Adjustment Following Breast Cancer in Low-Income Hispanic and Non-Hispanic White Women. Psycho-Oncology 19 (10):1069–1077. doi: 10.1002/pon.1661 [DOI] [PMC free article] [PubMed] [Google Scholar]