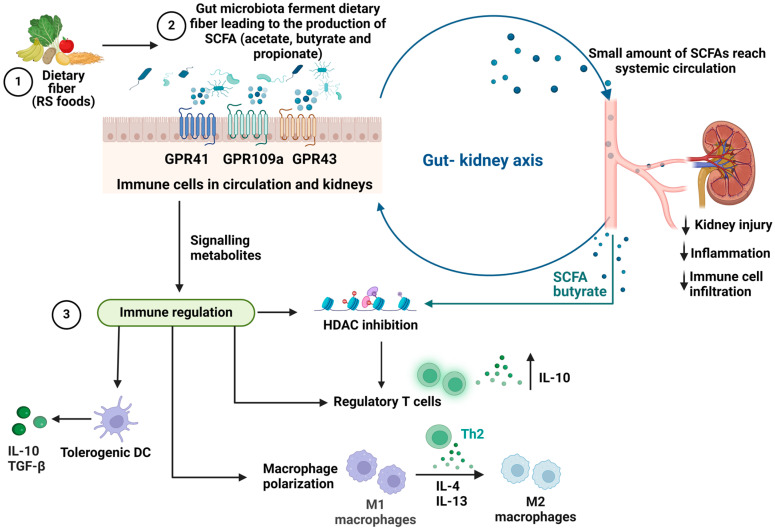
Figure 1.
The mechanism of the effects of SCFAs on the gut–kidney axis and immune cells. (1) Dietary fiber is made up of insoluble and soluble components. (2) The uptake of dietary fiber by intestinal microbiota increases the concentration of SCFAs in the intestine and encourages the growth of SCFA-producing bacteria. Acetate, butyrate, and propionate are the most abundant SCFAs produced by gut bacteria in the large intestine, with a molar ratio of 60:20:20 respectively [13]. (3) Renal cells, immune cells, and intestinal epithelial cells have SCFA-sensing GPCR, and upon binding can alter metabolic pathways (tricarboxylic acid cycle, β-oxidation, oxidative phosphorylation), epigenetic changes through histone deacetylase (HDAC) inhibition, phenotypes (M0 to M2 macrophages), and expression of inflammatory cytokines. SCFA butyrate is also known to act directly as an HDAC inhibitor, resulting in increased histone acetylation, influencing gene expression and cellular function, hence contributing to anti-inflammatory properties [14]. SCFAs may indirectly induce renoprotection through their immunomodulatory properties such as reducing leukocyte recruitment, inflammation, and kidney injury. This figure was created with Biorender.