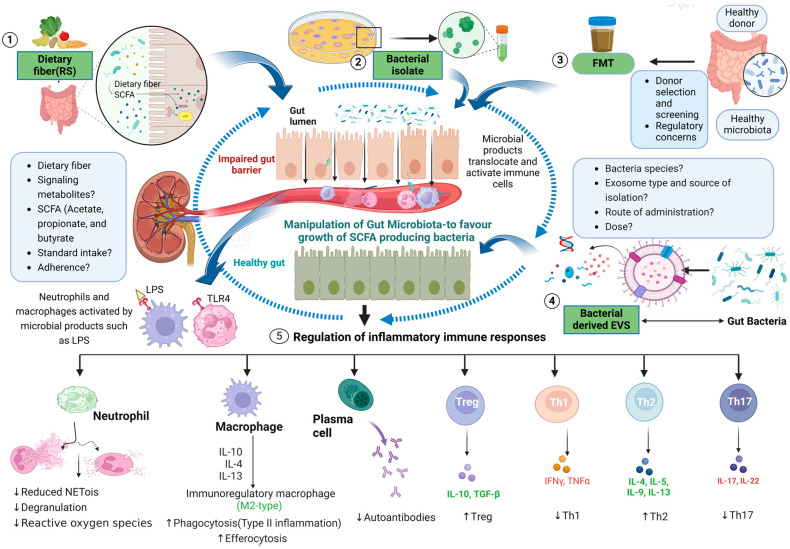
Figure 2.
Strategies for modulating the inflammatory response during autoimmune kidney disease. These include dietary fiber intake, SCFAs (namely acetate, propionate, and butyrate), the transfer of gut microbial isolate, faecal microbial transplantation, and gut bacterial EV therapy. (1) Dietary fibers and starches that are resistant to digestion in the small intestine promote gut microbiota, and the metabolized product (SCFAs) is in turn associated with gut microbiota homeostasis. (2) The transfer of immunomodulatory microbial isolate(s) can modulate inflammation and reduce the risk of introducing pathogenic bacteria. (3) Faecal microbiota transplantation from a healthy donor also introduces gut microbiota into the patient, thereby modulating inflammation. (4) Isolated and characterized EV from gut bacteria with known immunomodulatory properties can also serve as therapeutic targets. The yellow triangle shows when the innate sensor (TLR4) on the neutrophil cell surface detects bacterial LPS triggering subsequent adaptive immune responses. (5) As a result, all these potential targeted therapies could modulate CD4+ T cell differentiation, induce the activity of Treg responses, regulate B-cell activity, and regulate neutrophils and other immune cells, all dampening the host immune responses. Type 2 responses suppress Th1 responses against the disease and skew cytokine profiles, resulting in a dominant IL-4, IL-5, IL-9, and IL-13 response produced by expanded populations of alternatively activated macrophages. Abbreviations: FMT: faecal microbiota transplantation; IFNγ: interferon-gamma; IL: interleukin; LPS: lipopolysaccharide; M2: alternative-type macrophage; NETosis: formation of neutrophil extracellular traps; SCFA: short-chain fatty acids; TLR4: toll-like receptor 4; Th: helper T cell, TNFα: tumour necrosis factor alpha. This figure was created with Biorender.