FIG. 1.
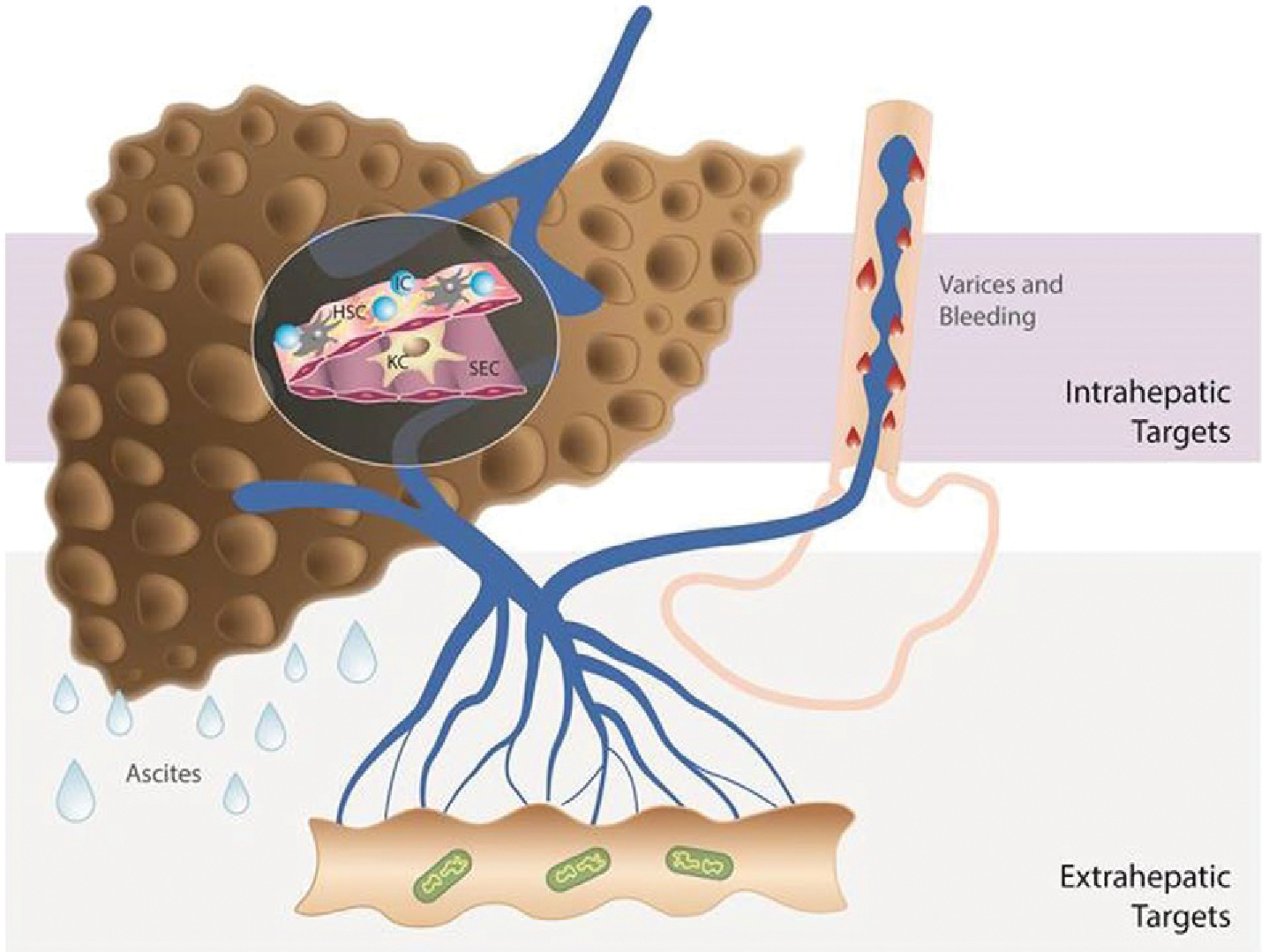
Different approaches to treat PH in cirrhosis. Strategies to decrease PP include drugs that act on intrahepatic targets: fibrosis, endothelial dysfunction, and inflammation and drugs that act on decreasing portal flow: splanchnic vasculature, microbiome, and others such as the nervous system, fat, etc., as recently reviewed.(109,110) A single drug may be able to affect more than one target (multitargeted approach): either two or more intrahepatic targets (e.g., statins) or one intrahepatic and one extrahepatic target (e.g., carvedilol). If a multitargeted drug is associated with unfavorable effects, the selective delivery either to the intrahepatic or to the extrahepatic circulation may be preferable. Drug therapy should also be tailored to the stage of cirrhosis. In compensated cirrhosis, the main treatment should target the underlying cause of cirrhosis in order to prevent progression of disease (or even to induce regression). Additionally, antifibrotic strategies together with drugs to decrease PP (if significant PH is present) are beneficial in compensated cirrhosis, given that fibrosis and PH are also self-maintaining processes. In decompensated cirrhosis (ascites, variceal hemorrhage), the main and short-/mid-term goal should be reduction in PP and prevention of further complications, given that antifibrotic and etiological therapies, although also important, might not have the necessary short-term impact. Abbreviations: IC, inflammatory cells; KC, Kupffer cells; SEC, sinusoidal endothelial cells. Additional references (#109 and #110) are provided as Supporting Information.
