Editorial
To the editor: The sinuses of Valsalva are focal expansions forming the aortic root walls. Rupture of the sinus of Valsalva usually occurs secondary to aneurysms of the sinus.[1] A continuous murmur is often audible in patients with a rupture, and in approximately one-sixth of patients with a continuous murmur, the murmur is caused by a rupture.[2] We report two cases of rupture of the sinus of Valsalva without any aneurysmal dilation of the aortic root, showing fistulous connections with the cardiac chambers.
In our first case, a 46-year-old man presented with complaints of episodic chest pain and breathlessness for 6 months. He had recently been diagnosed with type 2 diabetes mellitus. On presentation, his blood pressure was 130/70 mmHg with a pulse rate of 78 bpm. On physical examination, a continuous murmur could be heard in the parasternal region. Laboratory values were normal, and the chest radiograph was unremarkable.
On transthoracic echocardiography, there was evidence of prolapse of the right coronary cusp of the sinus of Valsalva, with a 5 mm defect in the right sinus with turbulent continuous (systolic and diastolic) flow through it seen on colour Doppler ultrasound. These findings raised a strong suspicion of rupture of the right cusp of the sinus of Valsalva with a communication with the right ventricular outflow tract and a left-to-right shunt. The findings were accompanied by mild mitral regurgitation and tricuspid regurgitation. Echocardiography revealed that all the cardiac chambers were normal in size, and the ventricles showed normal contractility.
The patient then underwent a cardiac computed tomography (CT) scan with coronary angiography. The CT examination was performed with an Ingenuity Core 128-slice CT scanner (Philips, India). Images were obtained with a slice thickness of 0.6 mm in the axial planes using electrocardiogram (ECG) gating, and reconstruction was done with coronal and sagittal images on the console. The contrast-enhanced images were obtained after bolus administration of a contrast agent. The CT scan showed a defect of 5.5 mm in size along the left lateral margin of the right coronary cusp of the sinus of Valsalva (Fig. 1). It also demonstrated a tubular fistulous connection between the right coronary cusp and the right ventricle at the level of the right ventricular outflow tract. The rupture was classified as type I according to the modified Sakakibara classification.[3] Incidentally seen on the cardiac CT scan were two small tubular accessory appendages arising from the left atrial appendage, pointing towards the atrio-aortic groove. Surgical closure of the ruptured sinus of Valsalva was performed.
Fig. 1.
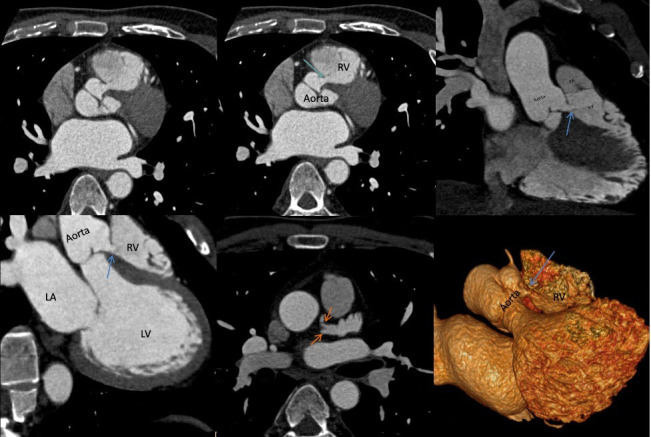
(A - D) CT coronary angiography images in axial and reconstructed coronal and oblique planes, showing a 5.5 mm defect along the left lateral margin of the right coronary cusp of the sinus of Valsalva with a tubular fistulous connection (arrows) between the right coronary cusp and the right ventricle at the level of the right ventricular outflow tract.
(E) CT angiography image in the axial plane with an incidental finding of two small tubular accessory appendages arising from the left atrial appendage, pointing towards the atrio-aortic groove (arrows).
(F) Volume-rendered 3D CT image showing a defect in the right coronary cusp of the sinus of Valsalva with a tubular fistulous connection (arrow) between the right coronary cusp and the right ventricle.
CT = computed tomography
RV = right ventricle
PA = pulmonary artery
LA = left atrium
LV = left ventricle
In our second case, a 61-year-old man presented with complaints of breathlessness for 4 months. This was not associated with any chest pain. He did not report any existing comorbidities. On physical examination, the blood pressure was 135/78 mmHg with a pulse rate of 75 bpm. On auscultation a continuous murmur was heard in the parasternal region, and transthoracic two-dimensional echocardiography revealed a 7 mm defect in the non-coronary cusp of the aortic valve, which was seen to be communicating with the right atrium through a tunnel. CT aortography was then performed to visualise the defect in greater detail and detect any coexisting vascular abnormalities. After bolus administration of a contrast agent, images with a slice thickness of 1 mm were obtained in the axial planes with reconstruction to coronal and sagittal sequences done on the console. A defect in the non-coronary cusp of the aortic valve was seen to be communicating with the dilated right atrium (Fig. 2). The rupture was classified as type IV according to the modified Sakakibara classification.[3] Contrast reflux was visualised in the form of early enhancement of the inferior vena cava and hepatic veins in the arterial phase. No other abnormalities were seen in the thoracic or abdominal aorta or the other great vessels. The cardiac chambers appeared normal without any evidence of dilation or wall hypertrophy. Surgical closure of the ruptured sinus of Valsalva was performed.
Fig. 2.
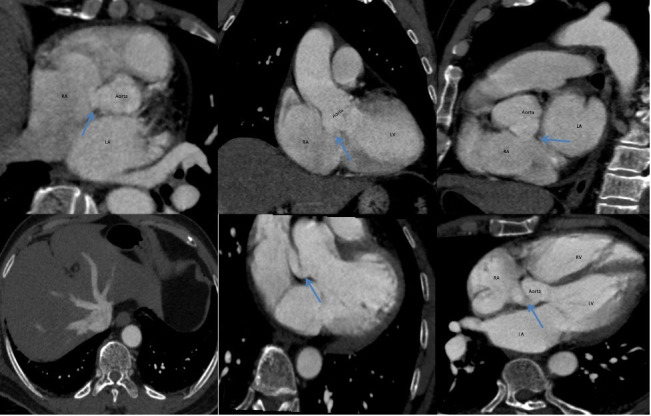
(A - C) CT aortography images in the axial and reconstructed coronal and oblique planes showing a defect in the non-coronary cusp of the aortic valve that communicates with the dilated right atrium (arrows).
(D) CT aortography image at the level of the abdominal aorta show contrast reflux in the form of early enhancement of the inferior vena cava and hepatic veins in the arterial phase.
(E and F) Reconstructed CT aortography images showing the defect visualised in the non-coronary cusp of the aortic valve communicating with the dilated right atrium (arrows).
CT = computed tomography
RA = right atrium
LA = left atrium
LV = left ventricle
RV = right ventricle
The aortic root is made up of the aortic valve leaflets, the commissures, the sinus of Valsalva, the sinotubular junction, and the annulus.[4] There are three sinuses of the aortic root, lying between the superior attachment formed by the sinotubular junction, which is a relatively constricted segment between the aortic root and the ascending aorta, and inferiorly by the aortic valve leaflets, which separate the aorta from the left ventricle. The right coronary sinus is the origin of the right coronary artery and the left coronary sinus is the origin of the left coronary artery. The non-coronary sinus does not give rise to any coronary artery. The attachment of the aortic valve leaflets into the aortic root wall in a semilunar fashion gives rise to a three-dimensional ring known as the aortic annulus.[4,5] Previous studies have shown the normal mean (standard deviation) end-diastole diameter of the sinus of Valsalva to be 3.2 (0.6) cm for men and 2.9 (0.5) cm for women.[4] These sinuses play an important role in aortic valve function by providing space to prevent blocking of the orifices of the coronary arteries from the aortic leaflets.
It has been found that rupture of the sinus of Valsalva is more common in men than in women, and in Asians than in other ethnic groups.[6] Congenital causes of rupture are deficiency of elastic tissue, as seen in Marfan syndrome or Ehlers-Danlos syndrome, or focal weakness of the elastic laminae between the aorta and the annulus fibrosus. Acquired causes are atherosclerosis, cystic medial necrosis, tuberculosis, bacterial endocarditis or cardiac complications of syphilis, and trauma. Iatrogenic causes such as a pseudoaneurysm resulting from haematoma formation after aortic valve replacement have been reported.[6]
Ruptures of the sinus of Valsalva are associated with other cardiac anomalies such as bicuspid aortic valve, ventricular septal defects, and other coronary artery anomalies. The aneurysms most commonly arise from the right coronary sinus and non-coronary sinuses and can rupture into the adjacent right ventricle, right atrium, left atrium, or rarely the interventricular septum.[7]
These aneurysms can cause complications and rupture later in life. Non-ruptured aneurysms may remain asymptomatic or manifest acutely as a result of a mass effect on adjacent structures. Asymptomatic aneurysms may present with a continuous murmur. Rupture of these aneurysms can lead to chest pain, dyspnoea, congestive heart failure, and cardiac arrest in extreme cases.[6] Untreated ruptured aneurysms may result in cardiac tamponade and eventually death in a few cases. One of the common complications of both ruptured and unruptured aneurysms is aortic regurgitation.[6] A continuous murmur is often audible in patients with a ruptured sinus of Valsalva and must be seen as a warning sign.[2]
The prevalence of the aortocardiac fistulas seen in our cases has not been studied extensively.[8] They can be congenital or acquired. If acquired, they can be due to trauma, iatrogenic causes such as cardiac or aortic surgery, or non-traumatic causes such as rupture of a sinus of Valsalva aneurysm, infective endocarditis or aortic dissection. A study showed that many patients with aorto-cardiac fistulas presented with symptoms of heart failure, with few of them experiencing chest pain or other symptoms.[8] Asymptomatic patients accounted for only 9% of the studied group, with a continuous murmur on auscultation being the only demonstrable finding.
Most ruptures of the sinus of Valsalva are initially seen on colour Doppler echocardiography, but the diagnosis is usually confirmed on angiography. Both CT and magnetic resonance imaging (MRI) have an additional role in diagnosing rupture of sinus of Valsalva aneurysms, as they are used in emergency settings.[6] ECG-gated contrast-enhanced CT provides better spatial resolution than other imaging modalities, and also gives detailed anatomical information on the surrounding structures. It is also possible to identify an aorto-cardiac shunt if present, and to identify a ruptured sinus of Valsalva and its connection to adjacent cardiac chambers. The surgeon can also be provided with three-dimensional representations, which are useful in deciding on the surgical approach. MRI has an advantage of accurate assessment of the origin and size of aneurysms and the surrounding anatomical structures. It is also helpful in identifying accompanying aortic regurgitation and in evaluating the haemodynamic pattern of the left ventricle.[6]
In this case report we have classified the sinus of Valsalva ruptures on the basis of the modified Sakakibara classification.[3] The first case was classified as type I, which is rupture into the right ventricle just below the pulmonary valve, and the second case was classified as type IV, in which there is protrusion and rupture into the right atrium.
An aggressive approach to a ruptured sinus of Valsalva is advisable, to prevent clinical deterioration and progression to severe cardiac failure. Operative procedures may include patch repair and aortic root or valve replacement if the rupture is accompanied by significant aortic or other valvular regurgitation. Reports suggest perioperative mortality of up to 3.9%, especially in the setting of pre-existing sepsis or endocarditis, so there is a need for strict endocarditis prophylaxis. After the surgical repair, patients’ life expectancy is similar to that of the healthy population. Recent advances include percutaneous transcatheter closure of ruptured sinus of Valsalva aneurysms using a duct occluder. [9] Percutaneous closure may be a better choice than surgical repair in critically ill patients with poor cardiac function and no associated anomalies that may require surgical repair, because of its advantages of less trauma and haemorrhage and rapid post-procedural recovery.[10]
In conclusion, our cases were unique as in both patients the rupture of the sinus of Valsalva was not accompanied by any aneurysmal dilation of the aortic root, which is commonly reported in the literature. In our cases, CT was useful in accurately depicting rupture of the right coronary cusps and non-coronary cusps of the aortic root at the sinus of Valsalva and their fistulous communications with the cardiac chambers, which demonstrates that CT can provide superior anatomical details of the sinus of Valsalva and the surrounding structures in comparison with other available imaging modalities.
References
- 1.Marroush TS, Boshara AR, Botros B, et al. Rupture of sinus of Valsalva aneurysm: Two case reports and a concise review of the literature. Heart Lung. 2018;47(2):131–135. doi: 10.1016/j.hrtlng.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Morch JE, Greenwood WF. Rupture of the sinus of Valsalva: A study of eight cases with discussion on the differential diagnosis of continuous murmurs. Am J Cardiol. 1966;18(6):827–836. doi: 10.1016/0002-9149(66)90426-7. [DOI] [PubMed] [Google Scholar]
- 3.Xin-Jin L, Xuan L, Bo P, et al. Modified Sakakibara classification system for ruptured sinus of Valsalva aneurysm. J Thorac Cardiovasc Surg. 2013;146(4):874–878. doi: 10.1016/j.jtcvs.2012.12.059. [DOI] [PubMed] [Google Scholar]
- 4.Hanna MF, Malguria N, Saboo SS, et al. Cross-sectional imaging of sinus of Valsalva aneurysms: Lessons learned. Diagn Interv Radiol. 2017;23(5):339–346. doi: 10.5152/dir.2017.16522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Troupis JM, Nasis A, Pasricha S, Patel M, Ellims AH, Seneviratne S. Sinus Valsalva aneurysm on cardiac CT angiography: Assessment and detection. J Med Imaging Radiat Oncol. 2013;57(4):444–447. doi: 10.1111/j.1754-9485.2012.02467.x. [DOI] [PubMed] [Google Scholar]
- 6.Bricker AO, Avutu B, Mohammed TL, et al. Valsalva sinus aneurysms: Findings at CT and MR imaging. Radiographics. 2010;30(1):99–110. doi: 10.1148/rg.301095719. [DOI] [PubMed] [Google Scholar]
- 7.Pampapati P, Rao HTA, Radhesh S, Anand HK, Praveen LS. Multislice CT imaging of ruptured left sinus of Valsalva aneurysm with fistulous track between left sinus and right atrium. J Radiol Case Rep. 2011;5(8):14–21. doi: 10.3941/jrcr.v5i8.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foster TJ, Amin AH, Busu T, et al. Aorto-cardiac fistula etiology, presentation, and management: A systematic review. Heart Lung. 2020;49(3):317–323. doi: 10.1016/j.hrtlng.2019.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moreels S, Dymarkowski S, de Ridder S. Ruptured sinus of Valsalva in an asymptomatic patient – a case report. Eur Cardiol. 2012;8(2):139–141. doi: 10.15420/ecr.2012.8.2.139. [DOI] [Google Scholar]
- 10.Yang K, Wei MD, Geng WL, et al. Safety and efficacy of percutaneous closure of ruptured sinus of Valsalva aneurysm. EuroIntervention. 2018;14(12):e1288–e1294. doi: 10.4244/EIJ-D-18-00294. [DOI] [PubMed] [Google Scholar]


