Supplementary Figure 2.
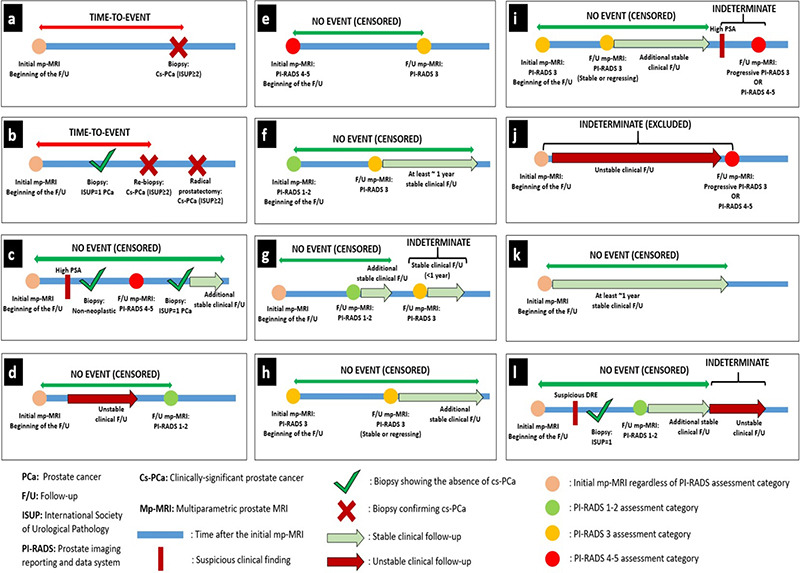
Illustrative case examples explaining follow-up evaluation. (a, b) The time-to-event was calculated considering the first detection time of cs-PCa (ISUP ≥2). (c) Cases without cs-PCa diagnosis during follow-up were considered cs-PCa-diagnosis-free at the points where histopathological examination results indicated non-neoplastic pathology or ISUP = 1 PCa, regardless of interim clinical or radiological follow-up findings. After biopsy, the final censoring time was determined based on additional clinical and/or radiological stability, if available. In the absence of any histopathological examination during an evaluated follow-up interval or in the subsequent follow-up period after a histopathological examination confirming the absence of cs-PCa, radiological stability was examined first and then clinical stability was considered to determine the final censoring time. (d) Cases with follow-up PI-RADS category 1–2 were considered cs-PCa diagnosis-free at the time of the follow-up mp-MRI, independent of previous clinical follow-up findings. After mp-MRI, the final censoring time was determined based on additional clinical and radiological follow-up, if available.
(e-i) The approach to cases with follow-up PI-RADS category 3 was determined based on the previous PI-RADS. (e) Cases with a PI-RADS downgrade from PI-RADS 4–5 to PI-RADS 3 were considered cs-PCa diagnosis-free at the time of follow-up mp-MRI. The final censoring time was determined based on additional clinical and radiological follow-up, if available. (f) Cases with a PI-RADS upgrade from PI-RADS 1–2 to PI-RADS 3 were evaluated for the presence of at least 1-year stable subsequent clinical follow-up or further radiological stability to be considered as cs-PCa diagnosis-free. (g) PI-RADS 3 cases that did not meet these criteria were considered indeterminate at the end of follow-up. Censoring was done based on the stable clinical and/or radiological follow-up interval between the first mp- MRI and the indeterminate follow-up interval. Cases without such a stable follow-up interval were excluded from survival analysis. (h) PI-RADS 3 cases that did not show any PI-RADS change and radiological progression in the follow-up mp-MRI were considered as cs-PCa-diagnosis-free at the time of follow-up mp-MRI. The final censoring time was determined based on additional clinical and radiological follow-up, if available. (i) Cases with progressive PI-RADS 3 lesion(s) or follow-up PI-RADS category of 4–5 were considered indeterminate regardless of interim clinical follow-up, unless a subsequent histopathological examination was performed. Censoring was done based on the stable clinical and/or radiological follow-up interval between the first mp-MRI and the indeterminate follow-up interval. (j) Cases without such a follow-up interval were excluded from survival analysis. (k) In the absence of histopathological or radiological examination during the evaluated follow-up interval or in the subsequent follow-up period after these examinations, clinical stability was evaluated to determine the final censoring time. Cases showing at least 1 year of clinical stability, regardless of baseline PI-RADS category, were censored as cs-PCa diagnosis-free. (l) Cases where the criteria for clinical stability were not met during a certain time interval were considered indeterminate. Censoring was done based on the stable clinical interval between the first mp- MRI and the indeterminate follow-up interval. cs-PCa, clinically significant prostate cancer; ISUP, International Society of Urological Pathology; PCa, prostate cancer; PI-RADS, Prostate Imaging Reporting and Data System; mp-MRI, multiparametric prostate magnetic resonance imaging
