Abstract
Despite the common occurrence of radial head fractures, there is still a lack of consensus on which radial head fractures should be treated surgically.
The radial head is an important secondary stabilizer in almost all directions. An insufficient radial head can lead to increased instability in varus–valgus and posterolateral rotatory directions, especially in a ligament-deficient elbow.
The decision to perform surgery is often not dictated by the fracture pattern alone but also by the presence of associated injury. Comminution of the radial head and complete loss of cortical contact of at least one fracture fragment are associated with a high occurrence of associated injuries.
Nondisplaced and minimally displaced radial head fractures can be treated non-operatively with early mobilization. Displacement (>2 mm) of fragments in radial head fractures without a mechanical block to pronation/supination is not a clear indication for surgery.
Mechanical block to pronation/supination and comminution of the fracture are indications for surgery.
The following paper reviews the current literature and provides state-of-the-art guidance on which radial head fractures should be treated surgically.
Keywords: radial head fractures, open reduction internal fixation, radial head excision, arthroplasty
Introduction
A radial head fracture is a common injury and the most common elbow fracture in adults. The estimated incidence of radial head fractures is 2.5−2.8 per 10 000 inhabitants per year (1, 2). On average, female patients are significantly older than male patients, with a mean age varying between 50 and 60 years for females and between 30 and 40 years for males (2). The explanation for this typical age distribution is a correlation with the presence of osteoporosis in females above 50 years and high-energy trauma in males (2, 3). Typically, the injury occurs when someone falls on an outstretched hand with the forearm in pronation. This results in axial load in combination with valgus and/or rotating forces across the elbow. This trauma mechanism can lead to a fracture of the radial head as it impacts against the capitellum (4). Radial head fractures can exert a notable influence on upper limb functionality due to the pivotal role of the radial head in stabilizing the elbow joint, secondary to the collateral ligaments and coronoid process. The management of radial head fractures encompasses a spectrum of treatment options, spanning from conservative methods to surgical procedures such as internal fixation, arthroplasty, or radial head excision (RHE).
Radial head fractures may be associated with other injuries of clinical importance, especially when secondary to high-energy traumatic mechanisms. Ligament disruption and associated elbow fractures, especially fractures of the coronoid, must be considered when evaluating fractures of the radial head. The extent of bony involvement, associated fractures, and soft tissue injury helps to determine the appropriate management of these complex injuries.
Despite the common occurrence of radial head fractures, there is a notable lack of consensus regarding their optimal management strategy. A recent British survey highlighted the lack of consensus in the management of displaced, non-comminuted radial head fractures among an experienced cohort of participating orthopedic surgeons (5). The purpose of this paper is to present a review of recent literature and to provide state-of-the-art guidance on which radial head fractures should be treated surgically.
Biomechanics
The radial head is a pivotal component of the elbow joint complex, contributing significantly to its biomechanical stability and functionality. The concave articulating surface of the proximal radius, particularly accentuated by thicker peripheral cartilage, interfaces with the convex surface of the humeral capitellum. Additionally, the lateral aspect and rim of the radial head articulate with the proximal ulna within the lesser sigmoid notch and with the lateral portion of the trochlea (zona conoidea) (6). Approximately 60% of the load on the elbow is transmitted through the radiohumeral joint, depending on the position of the forearm axis. Load transmission by the lateral compartment increases during elbow extension and forearm pronation.
The elbow is stabilized by primary and secondary stabilizers, of which the radial head is an important secondary stabilizer in almost all directions (4). For longitudinal stability, the radial head acts as a buttress to axial load in the elbow joint. In cases where the radial head demonstrates a severely comminuted fracture, there is a risk of proximal migration of the radius bone due to lack of support of the lateral column. This longitudinal migration is particularly facilitated when injuries occur to the interosseous membrane (IOM) and triangular fibrocartilage complex, as seen in longitudinal radio ulnar dissociation (7). The radial head also serves as a secondary stabilizer to valgus stress, with the medial collateral ligament (MCL) functioning as the primary stabilizing structure. Furthermore, the radial head contributes to stabilization against varus stress by tensioning the lateral collateral ligament (LCL) complex. Experimental studies have demonstrated that radial head resection can lead to increased instability in varus–valgus and posterolateral rotatory directions, especially in a ligament-deficient elbow (4, 8, 9, 10). Thus, when the collateral ligaments and the soft tissues of the forearm are intact, the radial head may be removed. If, however, either the IOM or distal radioulnar joint (DRUJ) has been violated or a medial or lateral collateral ligament has been disrupted, then radial head integrity is critical to elbow function.
In conjunction with the radial head, the elbow’s articulations involve the greater sigmoid notch of the ulna, as well as the trochlea and capitellum of the humerus. The interlocking configurations of these components play a significant role in maintaining elbow stability, in addition to the ligaments. The coronoid process serves as a primary stabilizer against axial stress, varus stress, and rotatory instability (4, 11). If the coronoid process is fractured, the radial head becomes a critical stabilizer (12).
Classification
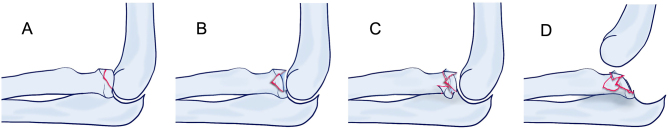
The classification for radial head fractures introduced by Mason in 1954 remains the most referenced classification system (13). In his initial publication, Mason reviewed 100 consecutive cases of radial head fractures and their management strategies. Mason described type I fractures as either fissures (non-displaced) or peripheral rim fractures (Fig. 1A). Type II fractures were characterized by marginal sector fractures with displacement (Fig. 1B). Type III fractures encompassed comminuted, displaced fractures involving the entirety of the radial head (Fig. 1C).
Figure 1.
Mason classification of radial head fractures (13). Fissures (non-displaced) or peripheral rim fractures (A) are classified as Mason type I fractures. Type II fractures are marginal sector fractures with displacement (B). Type III fractures are comminuted, displaced fractures involving the whole radial head (C). Radial head fractures accompanied by dislocation (D) were added as type IV fractures by Johnston (14).
In 1962, Johnston added a fourth type to signify radial head fractures accompanied by dislocation, irrespective of displacement or fragment comminution (Fig. 1D) (14). In 1987, Broberg and Morrey modified the Mason classification with the suggestion that a partial radial head fracture must be of sufficient size (at least 30% of the articular surface) and displacement (at least 2 mm) to be considered a displaced fracture (Mason type II, as opposed to nondisplaced Mason type I) (15). Despite widespread use, the Mason and modified Mason classifications exhibit limitations, notably moderate inter- and intraobserver reliability and inconsistent guidance regarding treatment or prognostic prediction (16, 17).
In 1997, Hotchkiss aimed to include the indications for surgical intervention. Type II fractures were redefined as reconstructable radial head fractures with a mechanical block during movement. Type III fractures were redefined as non-reconstructable radial head fractures (18).
However, despite their significant impact on treatment outcomes, it is noteworthy that all modified Mason classification systems lack inclusion of associated lesions. Van Riet et al. proposed in 2008 to enhance the Mason classification by incorporating a suffix to describe these associated lesions, based on clinical and intraoperative observations. Clinically relevant injuries were included: articular injury (c: coronoid, o: olecranon), followed by ligamentous injury (l: lateral collateral ligament, m: medial collateral ligament, d: distal radioulnar joint). This simplified system aids in identifying 97% of associated injuries (19).
Associated injury
Radial head fractures are frequently accompanied by associated osseous, chondral, or ligamentous injuries of the ipsilateral upper extremity. In a retrospective evaluation of 333 patients with a radial head fracture, van Riet et al. described an overall incidence of associated injuries in 39% (20). Both comminution of the radial head and complete loss of cortical contact of at least one fracture fragment are associated with a high occurrence of associated injuries (19, 20, 21, 22). Associated fractures of the upper extremity have been described in 10.2% of patients with a radial head fracture, with coronoid fractures being the most common associated fractures (1, 20). These fractures are common with dislocations of the elbow and can be part of a ‘terrible triad’ of the elbow. Studies using MRI show a 76–92% incidence of associated injuries in patients with a radial head fracture, with LCL and capitellar injury the most common (22, 23). However, most injuries detected with MRI in patients with radial head fractures are not symptomatic or of clinical importance in short-term follow-up (mean 13.3 months) (24).
Treatment options
The management of radial head fractures encompasses a spectrum of treatment options, spanning from conservative methods to surgical procedures. Conservative treatment usually consists of a pressure bandage and sling for support and early range of motion exercises with plain radiographic imaging follow-up to detect secondary fracture displacement (25). Surgical procedures consist of open or arthroscopic reduction and internal fixation, radial arthroplasty, or RHE.
Reduction and internal fixation
Open reduction and internal fixation can be performed by the lateral approach through the interval between anconeus and extensor carpi ulnaris muscles (Kocher interval) or the extensor digitorum communis (EDC) split interval. The EDC splitting approach provides greater exposure of the anterior half of the radial head while minimizing the risk of iatrogenic injury to the lateral ulnar collateral ligament (LUCL) compared to the Kocher approach (26). The Kocher interval provides greater exposure of the posteromedial quadrant of the radial head. However, most displaced radial head fractures involve the anterolateral quadrant (98%), whereas parts of the posteromedial quadrant are involved in a minority of the fractures (15%) (27). To protect the posterior interosseous nerve during the lateral approach, the forearm must be pronated, and care must be taken when pulling on the anterior retractors. Arthroscopic reduction and internal fixation offer an excellent view on the articular surfaces and associated chondral or ligamentous injury. However, the technique is challenging and requires expertise (28, 29).
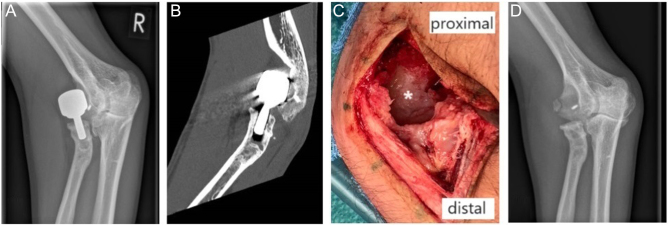
The goal for reduction and internal fixation is to obtain a stable and anatomic reconstruction. Headless screws are typically employed for the fixation of head fragments (Fig. 2A). While plates are commonly utilized for fixation when the whole head is involved and disrupted from the shaft (Fig. 2B), they necessitate removal in the majority of patients. The need for plate removal can be minimized by positioning the implant within the designated ‘safe zone’, an area of the radial head that remains non-contact with the ulna in both pronation and supination (Fig. 2C). However, despite the use of modern anatomical low profile locking plates, plate removal has still been reported up to 32% (30).
Figure 2.
Surgical treatment options for radial head fractures. Headless screw fixation for partial radial head fractures (A). Fixation of radial head fractures by plate and screw fixation (B), the plate should be placed in the safe zone of the proximal radius (C) to limit the risk of impingement of the plate in de proximal radioulnar joint. Fixation of the radial head with crossing headless screws (tripod technique) (D) as alternative for plate fixation. Radial head arthroplasty (E) and radial head excision (F).
An alternative to plate fixation is the low-profile tripod fixation technique, in which crossing headless screws are used to fix the head to the radial shaft (Fig. 2D). This technique is described to achieve a biomechanical stability comparable to plate fixation (31) with the advantage of less complications and less need of implant removal (32, 33).
Radial head arthroplasty and radial head excision
Radial head arthroplasty (RHA) or RHE are surgical options for severely comminuted non-reconstructable radial head fractures (Fig. 2E and F). The determination of what represents a non-reconstructable radial head is subjective. Especially in patients with concomitant posterolateral instability due to injury to the lateral ligamentous complex or coronoid, valgus instability due to injury of the MCL, or axial instability due to an injury of the IOM, RHA is a good choice to obtain optimal radiocapitellar contact when the radial head cannot be fixed. Elbow injuries that require RHA are associated with moderate reoperation rates around 20% (34). However, 93% of reoperations are reported to occur within the first year of surgery and are related to persistent instability or stiffness of the elbow, rather than implant failure (35). Functional outcomes following RHA are good to excellent at long-term follow-up (minimum of 8 years), despite radiological signs of degeneration in about 27% and (capitellar) erosions in about 32% of patients (34). The latter being unfavorable outcomes in the young patient where erosion rates are reported to be 62%, rates of ulnohumeral degeneration 15%, and lucency around the stem 100% (Fig. 3) (36). Overlengthening of the radial head prosthesis is thought to be a significant complication and cause of rapid capitellar erosion and degenerative changes (37). In overlengthening, the head of the prosthesis overextends the physiological level of the native radial head and leads to overstuffing of the radiohumeral joint and compression and potential early osteoarthritis of the medial part of the ulnohumeral joint. The incidence of overlengthening is not precisely known, but estimations range to up to 20% of all implanted prostheses (37) and could be limited by using the proximal rim of the lesser sigmoid notch as reference for the correct height of the implant. Overlengthening should be differentiated from insufficiency of the IOM resulting in persisting proximal migration of the radius and derangement of the DRUJ. Oversizing of the head of the implant can result in attenuation of the LCL complex, finally resulting in instability in posterolateral direction.
Figure 3.
Plain radiograph (A) and CT scan (B) showing loosening of a radial head arthroplasty in a 32-year-old male, with extensive erosion of the capitellum and joint space narrowing in the ulnohumeral compartment. After removal of the implant, a large defect marked by * is seen in the capitellum (C). Postoperative plain radiograph (D) shows the destruction of the capitellum and ulnohumeral joint space narrowing.
RHE might have the least postoperative complications (abnormal ossification, fracture hardware removal, nerve palsy, and revision) in the treatment of comminuted radial head fractures, followed by RHA and ORIF (38). Outcomes of RHE for acute fracture are good to excellent (39). However, symptoms as instability of the proximal radius stump, early osteoarthritis of the ulnohumeral joint, and complaints of the DRUJ are frequently seen in our experience and might be under reported as most PROMS used are not validated for these symptoms. Moreover, a RHE should not be performed when concurrent coronoid fractures or ligamentous injuries are present, which is the case in most comminuted radial head fractures (20, 21, 22).
Treatment of nondisplaced or minimally displaced fractures of the radial head (Mason–Hotchkiss type I)
Isolated nondisplaced or minimally displaced (<2 mm) fractures without a mechanical block in forearm rotation can be treated conservatively. Intra-articular hematoma might mimic a mechanical block in rotation due to pressure and pain. Sterile injection of an analgetic might be used to examine a possible mechanical block or the examination should be repeated after a few days. Outcomes of nonoperative treatment of nondisplaced or minimally displaced Mason type I fractures are predominantly favorable, with no significant difference in elbow function when the formerly fractured elbow was compared to the nonfractured elbow at a mean of 21 years follow-up (40). In some studies, persistent complaints have been reported in 20% of cases, with the shortest period of immobilization resulting in the best patient-reported outcome measure scores (PROMs) at follow-up (41, 42). The usefulness of subsequent radiographs during follow-up of nonoperative treatment is debated, as they do not alter treatment of radial head fractures with no associated ligament injuries or fractures (43, 44, 45).
Treatment of displaced (>2 mm) fracture of the radial head or neck (angulated) without severe comminution (Mason–Hotchkiss type II)
Mason–Hotchkiss type II fractures are displaced fractures of the head (usually >2 mm) or angulation at the neck, which are technically possible to repair by open reduction and internal fixation. This also includes comminuted fractures with more than two fragments but without severe comminution. The displacement of the fragments may lead to a mechanical block in motion. There is consensus in the literature and among surgeons that a mechanical block to rotation is a clear indication for surgery (5). A CT scan is necessary in all type II fractures to determine fracture displacement, number and location of fragments, and the presence of associated fractures. ORIF is the preferred surgery, and the limitation for ORIF depends on the possibility to obtain a stable, anatomical reconstruction. The type of ORIF is usually dependent on fracture pattern, the number of fragments, and the discontinuity of the radial head with the neck.
However, there is no clear consensus on whether isolated displaced partial radial head fractures (Mason type II) without a mechanical block should be treated with ORIF or nonoperatively. A systematic review performed by Kaas et al. in 2012 found the success rates of operative treatment to be higher than the success rates of nonoperatively treated patients, but no firm conclusion could be drawn due to the low level of available evidence (46). In 2021, Lanzerath et al. performed an update of this systematic review, concluding that operative treatment is not superior to nonoperative treatment concerning functional outcome parameters (47). Treatment was successful in 90.9% of patients treated with ORIF and 95.1% in patients treated nonoperatively. Subsequent surgery rates were higher for patients treated with ORIF, but 5.2% of the patients treated with ORIF had signs of osteoarthritis compared with 11.9% of the patients treated nonoperatively. To our knowledge, only one randomized controlled trial is available comparing operative treatment to nonoperative treatment for isolated partial (Mason type II) radial head fractures of at least one-third of the articular surface, >2 mm step-off, but less than 2 mm of gap between fragments (48). This study concluded that nonoperatively treated adults with an isolated Mason type II radial head fracture had similar functional results after 1 year compared with operatively treated patients. In addition, complication rates were low for both operative and nonoperative treatment. Although the target sample size of this trial was not reached because of slow recruitment and a high number of crossovers from the operative group to the nonoperative group (because of minor complaints), the study adds evidence that displacement (>2 mm step-off) of isolated partial radial head fractures is not a clear indication for surgery.
At this moment, there is also no conclusive data on the acceptable amount of angulation of the radial head in relation to the shaft in the literature. Some studies report that the displacement at the neck should not exceed 4 mm (49, 50).
Comminution (>2 fragments) of isolated radial head fractures is generally believed to be an indication for surgery (50). Originally, comminuted radial head fractures were classified as Mason type III fractures and advised to be resected or replaced by RHA (13). The modified Mason classification by Hotchkiss included comminuted radial head fractures that are amendable for reconstruction into the type II group of fractures. A systematic review published in 2021 of 12 comparative studies and one randomized controlled trial concluded that RHA and RHE had lower risks of complications (abnormal ossification, fracture hardware removal, nerve palsy and revision) compared to ORIF for comminuted radial head fracture (38). RHA was reported to be the most effective treatment in terms of elbow performance outcomes (Mayo elbow performance index; MEPI). However, there was a very wide range in follow-up duration (12.7–157 months) between included studies, and outcomes like osteoarthritis, capitellar erosion, or elbow instability were not analyzed. More recent studies indicate that ORIF of radial head fractures with up to three or four fragments can achieve good functional results with good fracture healing and a low complication rate and seems to be a valid alternative to RHA (51). In comminuted radial head fractures, an in-situ reduction and fixation of the fragments can be challenging and sometimes not possible. An on-table (ex-situ) reconstruction of the radial head and subsequent fixation to the shaft with plate osteosynthesis (Fig. 4) is a reliable option with good clinical outcomes and low complication rate. It can restore joint alignment and maintain radial length. The risk for avascular necrosis is low, and the bone healing rate is high (52, 53, 54). Two small retrospective studies reported that preserving the patient’s own radial head with screws in comminuted fractures without subsequent fixation of the head to the radial shaft might be a good alternative to plate fixation (55, 56). Functional outcomes were equal or superior as compared to plate fixation. Nonunions were frequently observed, but asymptomatic, and rates of development of osteoarthritis were seen in the majority of patients in both groups (55). The implant needed to be removed in 54% of the plate fixation group (56).
Figure 4.
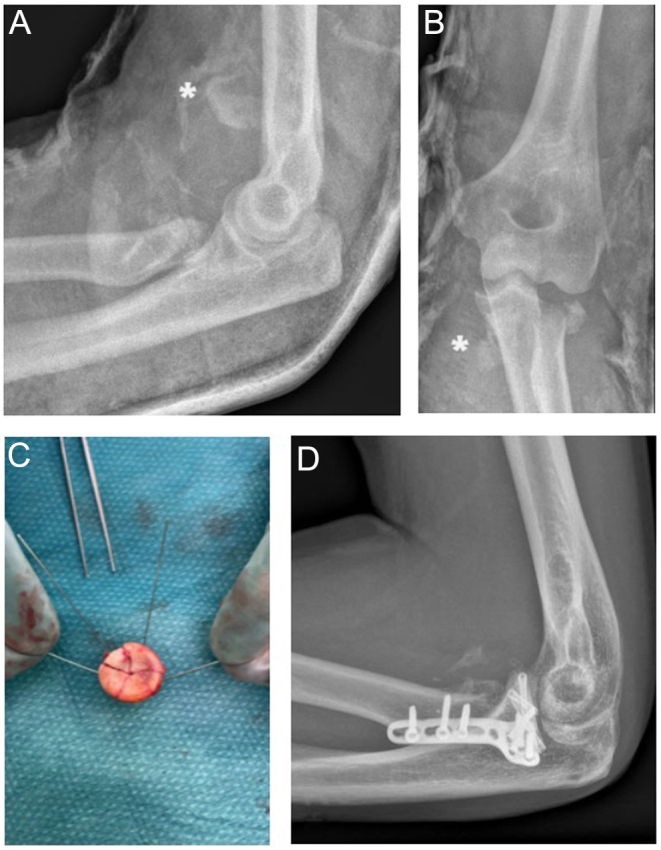
Plain radiographs of a very comminuted radial head fracture showing fragments (marked by *) proximal to the anterior fossa (A) and on the medial side of the proximal ulna (B). All fragments were retrieved and an on-table reconstruction of the five fragments was performed (C). Fixation of the radial head to the shaft was performed with plate osteosynthesis in de safe zone (D).
Treatment of severely comminuted fracture of the radial head and neck (Mason–Hotchkiss type III)
Severely comminuted radial head fractures that are judged not to be reconstructable, based on radiographs, CT scans, and intraoperative appearance, usually require removal of fragments to improve movement. The determination when a radial head fracture is reconstructable or not is subjective, but having four or more fragments and complete loss of cortical continuity of one of the fragments are negative predictors for a successful outcome after fixation and highly correlated to associated injury (20, 21, 57). The high appearance of associated injuries in severely comminuted radial head fractures should make surgeons cautious to perform a radial head resection, and it should not be performed when a coronoid fracture or ligamentous injury is present (39). In general, RHA is reported to result in satisfactory clinical outcomes and modest complication and revision rates at long-term follow-up (34). Fractures with associated elbow dislocation appear to be at the highest risk for reoperation (35).
Treatment of associated injury
Whether radial head fractures should be treated surgically is also largely dependent on associated fractures or ligamentous injuries. Associated fractures of the coronoid, olecranon, or distal humerus should be treated by open reduction and internal fixation. Osteochondral defects of the capitellum might need debridement when loose bodies are present. Large capitellar fragments should be treated with fixation. Stability of the elbow should be examined, and lesions of the MCL or LCL should be repaired in cases with instability.
Conclusion and recommendations
Despite the common occurrence of radial head fractures, there is still a notable lack of consensus regarding their optimal management strategy. The goal of management of radial head fractures is to achieve a stable, functional, and pain-free elbow joint. The decision to perform surgery if often not dictated by the fracture pattern alone but also by the presence of associated injury. In all radial head fractures, thorough examination of elbow and DRU joint instability and associated fractures should be performed.
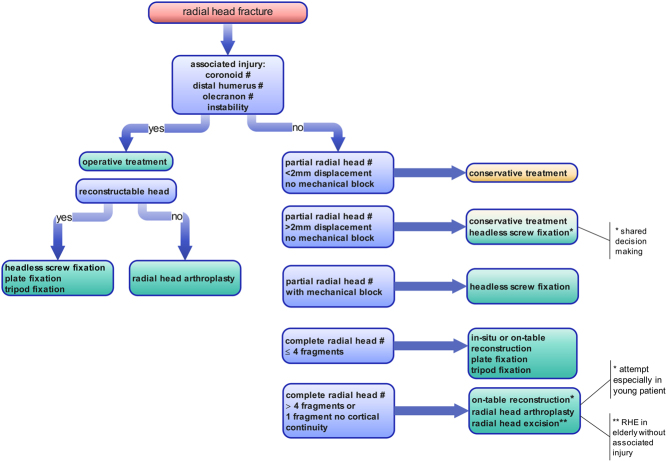
Based on the best available evidence and own preference and experience, we have designed a treatment algorithm for the management of radial head fractures (Fig. 5). The algorithm might be helpful for surgeons in their decision-making which radial head fractures should be treated surgically. There is consensus in literature that non-displaced/minimally displaced partial radial head fractures without a mechanical block can be treated nonoperatively. Optimal treatment for partially displaced fractures without a mechanical block remains uncertain, and both treatment options (conservative or ORIF) as well as their risks for complications should be discussed with the patient. All radial head fractures with a mechanical block in pronation/supination and comminuted fractures should be treated surgically. Our preference is to attempt open reduction and internal fixation for all radial head fractures, regardless of the number of fragments, with RHA available as a backup option if fixation proves unfeasible. Especially in the young patients, we prefer to avoid RHA to limit the risk of capitellar erosion and ulnohumeral osteoarthritis. RHE should not be performed when concurrent coronoid fractures or ligamentous injuries are present, which is the case in most comminuted radial head fractures.
Figure 5.
Treatment algorithm for radial head fractures.
In the literature, almost all studies comparing the effect of different treatment modalities on functional outcome and complications for the various types of radial head fractures have a retrospective design, and randomized controlled trials are scare. To further clarify which radial head fractures should be treated surgically, more randomized controlled trials are needed.
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this instructional lecture
Funding Statement
This instructional lecture did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author contribution statement
Conceptualization: AW, LL, JC, DE; Methodology: AW; Investigation: AW; Resources: AW, LL; Data curation: AW, JC, DE; Writing – Original Draft: AW; Writing – Review and Editing: AW, LL, JC, DE; Visualization: AW, LL; Supervision: JC, DE; Project Administration: AW. All authors read and agreed to the final version of the manuscript.
Acknowledgements
The authors wish to thank Christa Niehot from the Erasmus MC Medical Library for developing and updating the search strategies.
References
- 1.Kaas L van Riet RP Vroemen JP & Eygendaal D. The incidence of associated fractures of the upper limb in fractures of the radial head. Strategies in Trauma and Limb Reconstruction 2008371–74. ( 10.1007/s11751-008-0038-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaas L van Riet RP Vroemen JP & Eygendaal D. The epidemiology of radial head fractures. Journal of Shoulder and Elbow Surgery 201019520–523. ( 10.1016/j.jse.2009.10.015) [DOI] [PubMed] [Google Scholar]
- 3.Kaas L Sierevelt IN Vroemen JP van Dijk CN & Eygendaal D. Osteoporosis and radial head fractures in female patients: a case-control study. Journal of Shoulder and Elbow Surgery 2012211555–1558. ( 10.1016/j.jse.2012.03.007) [DOI] [PubMed] [Google Scholar]
- 4.Morrey BF & An KN. Stability of the elbow: osseous constraints. Journal of Shoulder and Elbow Surgery 200514174S–178S. ( 10.1016/j.jse.2004.09.031) [DOI] [PubMed] [Google Scholar]
- 5.Barakat A McDonald C & Singh H. Current concepts in the management of radial head fractures: a national survey and review of the literature. Annals of the Royal College of Surgeons of England 2023105469–475. ( 10.1308/rcsann.2022.0109) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeon IH Chun JM Lee CS Yoon JO Kim PT An KN Morrey BF & Shin HD. Zona Conoidea of the elbow: another articulation between the radial head and lateral trochlear of the elbow. Journal of Bone and Joint Surgery 201294517–522. ( 10.1302/0301-620X.94B4.27842) [DOI] [PubMed] [Google Scholar]
- 7.Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. Journal of Bone and Joint Surgery 195133B244–247. [PubMed] [Google Scholar]
- 8.Johnson JA Beingessner DM Gordon KD Dunning CE Stacpoole RA & King GJ. Kinematics and stability of the fractured and implant-reconstructed radial head. Journal of Shoulder and Elbow Surgery 200514195S–201S. ( 10.1016/j.jse.2004.09.034) [DOI] [PubMed] [Google Scholar]
- 9.Jensen SL Olsen BS & Sojbjerg JO. Elbow joint kinematics after excision of the radial head. Journal of Shoulder and Elbow Surgery 19998238–241. ( 10.1016/s1058-2746(9990135-0) [DOI] [PubMed] [Google Scholar]
- 10.Beingessner DM Dunning CE Gordon KD Johnson JA & King GJ. The effect of radial head excision and arthroplasty on elbow kinematics and stability. Journal of Bone and Joint Surgery 2004861730–1739. ( 10.2106/00004623-200408000-00018) [DOI] [PubMed] [Google Scholar]
- 11.Schneeberger AG Sadowski MM & Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. Journal of Bone and Joint Surgery 200486975–982. ( 10.2106/00004623-200405000-00013) [DOI] [PubMed] [Google Scholar]
- 12.O'Driscoll SW Jupiter JB King GJ Hotchkiss RN & Morrey BF. The unstable elbow. Instructional Course Lectures 20015089–102. ( 10.2106/00004623-200005000-00013) [DOI] [PubMed] [Google Scholar]
- 13.Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. British Journal of Surgery 195442123–132. ( 10.1002/bjs.18004217203) [DOI] [PubMed] [Google Scholar]
- 14.Johnston GW. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Medical Journal 19623151–56. [PMC free article] [PubMed] [Google Scholar]
- 15.Broberg MA & Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clinical Orthopaedics and Related Research 1987216109–119. ( 10.1097/00003086-198703000-00017) [DOI] [PubMed] [Google Scholar]
- 16.Doornberg J Elsner A Kloen P Marti RK van Dijk CN & Ring D. Apparently isolated partial articular fractures of the radial head: prevalence and reliability of radiographically diagnosed displacement. Journal of Shoulder and Elbow Surgery 200716603–608. ( 10.1016/j.jse.2006.10.015) [DOI] [PubMed] [Google Scholar]
- 17.Guitton TG & Ring D. Science of variation G. Interobserver reliability of radial head fracture classification: two-dimensional compared with three-dimensional CT. Journal of Bone and Joint Surgery 2011932015–2021. ( 10.2106/JBJS.J.00711) [DOI] [PubMed] [Google Scholar]
- 18.Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? Journal of the American Academy of Orthopaedic Surgeons 199751–10. ( 10.5435/00124635-199701000-00001) [DOI] [PubMed] [Google Scholar]
- 19.van Riet RP & Morrey BF. Documentation of associated injuries occurring with radial head fracture. Clinical Orthopaedics and Related Research 2008466130–134. ( 10.1007/s11999-007-0064-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Riet RP Morrey BF O'Driscoll SW & Van Glabbeek F. Associated injuries complicating radial head fractures: a demographic study. Clinical Orthopaedics and Related Research 2005441351–355. ( 10.1097/01.blo.0000180606.30981.78) [DOI] [PubMed] [Google Scholar]
- 21.Rineer CA Guitton TG & Ring D. Radial head fractures: loss of cortical contact is associated with concomitant fracture or dislocation. Journal of Shoulder and Elbow Surgery 20101921–25. ( 10.1016/j.jse.2009.05.015) [DOI] [PubMed] [Google Scholar]
- 22.Kaas L Turkenburg JL van Riet RP Vroemen JP & Eygendaal D. Magnetic resonance imaging findings in 46 elbows with a radial head fracture. Acta Orthopaedica 201081373–376. ( 10.3109/17453674.2010.483988) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Itamura J Roidis N Mirzayan R Vaishnav S Learch T & Shean C. Radial head fractures: MRI evaluation of associated injuries. Journal of Shoulder and Elbow Surgery 200514421–424. ( 10.1016/j.jse.2004.11.003) [DOI] [PubMed] [Google Scholar]
- 24.Kaas L van Riet RP Turkenburg JL Vroemen JP van Dijk CN & Eygendaal D. Magnetic resonance imaging in radial head fractures: most associated injuries are not clinically relevant. Journal of Shoulder and Elbow Surgery 2011201282–1288. ( 10.1016/j.jse.2011.06.011) [DOI] [PubMed] [Google Scholar]
- 25.Mahmoud SS Moideen AN Kotwal R & Mohanty K. Management of Mason type 1 radial head fractures: a regional survey and a review of literature. European Journal of Orthopaedic Surgery and Traumatology 2014241133–1137. ( 10.1007/s00590-013-1386-8) [DOI] [PubMed] [Google Scholar]
- 26.Desloges W Louati H Papp SR & Pollock JW. Objective analysis of lateral elbow exposure with the extensor digitorum communis split compared with the Kocher interval. Journal of Bone and Joint Surgery 201496387–393. ( 10.2106/JBJS.M.00001) [DOI] [PubMed] [Google Scholar]
- 27.Mellema JJ Eygendaal D van Dijk CN Ring D & Doornberg JN. Fracture mapping of displaced partial articular fractures of the radial head. Journal of Shoulder and Elbow Surgery 2016251509–1516. ( 10.1016/j.jse.2016.01.030) [DOI] [PubMed] [Google Scholar]
- 28.Guerra E Marinelli A Tortorella F Floter MDS Ritali A Sessa A Carbone G & Cavallo M. Elbow arthroscopy for the treatment of radial head fractures: surgical technique and 10 years of follow up results compared to open surgery. Journal of Clinical Medicine 202312. ( 10.3390/jcm12041558) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rolla PR Surace MF Bini A & Pilato G. Arthroscopic treatment of fractures of the radial head. Arthroscopy 200622233.e1–233.e6. ( 10.1016/j.arthro.2005.10.003) [DOI] [PubMed] [Google Scholar]
- 30.Gruszka D Nowak TE Tkacz T Wagner D & Rommens PM. Complex radial head and neck fractures treated with modern locking plate fixation. Journal of Shoulder and Elbow Surgery 2019281130–1138. ( 10.1016/j.jse.2018.11.056) [DOI] [PubMed] [Google Scholar]
- 31.Rebgetz PR Daniele L Underhill ID Ochsner A & Taylor FJ. A biomechanical study of headless compression screws versus a locking plate in radial head fracture fixation. Journal of Shoulder and Elbow Surgery 201928e111–e116. ( 10.1016/j.jse.2018.10.008) [DOI] [PubMed] [Google Scholar]
- 32.Adiguzel İF Orman O Unkar EA Baydar M Eren M & Ozturk K. Comparing the outcomes of tripod technique and locked plate fixation for the treatment of Mason type 3 radial head fractures. Joint Diseases and Related Surgery 202334716–723. ( 10.52312/jdrs.2023.1161) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Model Z Merchan N Rozental TD & Harper CM. Outcomes of radial head fractures treated with the "tripod technique". Journal of Hand Surgery 202247582.e1–e5. ( 10.1016/j.jhsa.2021.06.014) [DOI] [PubMed] [Google Scholar]
- 34.Davey MS Davey MG Hurley ET Galbraith JG Molony D Mullett H & Pauzenberger L. Long-term outcomes of radial head arthroplasty for radial head fractures-a systematic review at minimum 8-year follow-up. Journal of Shoulder and Elbow Surgery 2021302438–2444. ( 10.1016/j.jse.2021.03.142) [DOI] [PubMed] [Google Scholar]
- 35.Campbell BR Rengifo S Wickes CB Amer KM & Ilyas AM. Radial head arthroplasty for fracture: implant survivorship and outcomes at mean follow-up of 8 years. Journal of Hand Surgery 2023. ( 10.1016/j.jhsa.2023.04.020) [DOI] [PubMed] [Google Scholar]
- 36.Sims LA Aibinder WR King GJW & Faber KJ. The unsalvageable radial head in patients aged 30 years and younger. Journal of Hand Surgery 202146989–997. ( 10.1016/j.jhsa.2021.06.011) [DOI] [PubMed] [Google Scholar]
- 37.Wegmann K Hackl M Leschinger T Burkhart KJ & Muller LP. Overlengthening of the radial column in radial head replacement: a review of the literature and presentation of a classification system. Archives of Orthopaedic and Trauma Surgery 20211411525–1539. ( 10.1007/s00402-020-03619-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chaijenkij K Arirachakaran A & Kongtharvonskul J. Clinical outcomes after internal fixation, arthroplasty and resection for treatment of comminuted radial head fractures: a systematic review and network meta-analysis. Musculoskeletal Surgery 202110517–29. ( 10.1007/s12306-020-00679-3) [DOI] [PubMed] [Google Scholar]
- 39.Hildebrand AH Zhang B Horner NS King G Khan M & Alolabi B. Indications and outcomes of radial head excision: a systematic review. Shoulder and Elbow 202012193–202. ( 10.1177/1758573219864305) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Herbertsson P Josefsson PO Hasserius R Karlsson C Besjakov J & Karlsson MK. Displaced Mason type I fractures of the radial head and neck in adults: a fifteen- to thirty-three-year follow-up study. Journal of Shoulder and Elbow Surgery 20051473–77. ( 10.1016/j.jse.2004.07.001) [DOI] [PubMed] [Google Scholar]
- 41.Paschos NK Mitsionis GI Vasiliadis HS & Georgoulis AD. Comparison of early mobilization protocols in radial head fractures. Journal of Orthopaedic Trauma 201327134–139. ( 10.1097/BOT.0b013e31825cf765) [DOI] [PubMed] [Google Scholar]
- 42.Smits AJ Giannakopoulos GF & Zuidema WP. Long-term results and treatment modalities of conservatively treated Broberg-Morrey type 1 radial head fractures. Injury 2014451564–1568. ( 10.1016/j.injury.2014.05.034) [DOI] [PubMed] [Google Scholar]
- 43.Burton KR Mellema JJ Menendez ME Ring D & Chen NC. The yield of subsequent radiographs during nonoperative treatment of radial head and neck fractures. Journal of Shoulder and Elbow Surgery 2016251216–1222. ( 10.1016/j.jse.2016.03.007) [DOI] [PubMed] [Google Scholar]
- 44.Fenoglio AK Stephens AR Zhang C Presson AP Tyser AR & Kazmers NH. Evaluating the utility of follow-up radiographs for isolated radial head fractures undergoing initial nonoperative treatment. Journal of Orthopaedic Trauma 201933e291–e295. ( 10.1097/BOT.0000000000001489) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shulman BS Lee JH Liporace FA & Egol KA. Minimally displaced radial head/neck fractures (Mason type-I, OTA types 21A2.2 and 21B2.1): are we "over treating" our patients? Journal of Orthopaedic Trauma 201529e31–e35. ( 10.1097/BOT.0000000000000173) [DOI] [PubMed] [Google Scholar]
- 46.Kaas L Struijs PA Ring D van Dijk CN & Eygendaal D. Treatment of Mason type II radial head fractures without associated fractures or elbow dislocation: a systematic review. Journal of Hand Surgery 2012371416–1421. ( 10.1016/j.jhsa.2012.03.042) [DOI] [PubMed] [Google Scholar]
- 47.Lanzerath F Hackl M Wegmann K Muller LP & Leschinger T. The treatment of isolated Mason type II radial head fractures: a systematic review. Journal of Shoulder and Elbow Surgery 202130487–494. ( 10.1016/j.jse.2020.10.011) [DOI] [PubMed] [Google Scholar]
- 48.Mulders MAM Schep NWL de Muinck Keizer RO Kodde IF Hoogendoorn JM Goslings JC & Eygendaal D. Operative vs. nonoperative treatment for Mason type 2 radial head fractures: a randomized controlled trial. Journal of Shoulder and Elbow Surgery 2021301670–1678. ( 10.1016/j.jse.2021.02.025) [DOI] [PubMed] [Google Scholar]
- 49.Akesson T Herbertsson P Josefsson PO Hasserius R Besjakov J & Karlsson MK. Displaced fractures of the neck of the radius in adults. An excellent long-term outcome. Journal of Bone and Joint Surgery 200688642–644. ( 10.1302/0301-620X.88B5.17226) [DOI] [PubMed] [Google Scholar]
- 50.van Riet RP van den Bekerom M Van Tongel A Spross C Barco R & Watts AC. Radial head fractures. Shoulder and Elbow 202012212–223. ( 10.1177/1758573219876921) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Helmstetter T Maniglio M Fornaciari P Tannast M & Vial P. Open reduction and internal fixation of modified Mason type III/IV radial head fractures with more than three fragments: an analysis of the clinical outcome and reoperation rate. European Journal of Orthopaedic Surgery and Traumatology 2024341121–1130. ( 10.1007/s00590-023-03772-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Everding J Raschke MJ Polgart P Gruneweller N Wahnert D & Schliemann B. Ex situ reconstruction of comminuted radial head fractures: is it truly worth a try? Archives of Orthopaedic and Trauma Surgery 20191391723–1729. ( 10.1007/s00402-019-03250-3) [DOI] [PubMed] [Google Scholar]
- 53.Kastenberger T Kaiser P Spicher A Stock K Benedikt S Schmidle G & Arora R. Clinical and radiological outcome of Mason-Johnston types III and IV radial head fractures treated by an on-table reconstruction. Journal of Orthopaedic Surgery and Research 202217503. ( 10.1186/s13018-022-03394-w) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kiran Kumar GN Sharma G Farooque K Sharma V Jain V Singh R & Morey V. On-table reconstruction and fixation of Mason type III radial head fractures. Chinese Journal of Traumatology 201518288–292. ( 10.1016/j.cjtee.2015.11.005) [DOI] [PubMed] [Google Scholar]
- 55.Gregori M Zott S Hajdu S & Braunsteiner T. Preserving the radial head in comminuted Mason type III fractures without fixation to the radial shaft: a mid-term clinical and radiographic follow-up study. Journal of Shoulder and Elbow Surgery 2019282215–2224. ( 10.1016/j.jse.2019.07.036) [DOI] [PubMed] [Google Scholar]
- 56.Neumann M Nyffeler R & Beck M. Comminuted fractures of the radial head and neck: is fixation to the shaft necessary? Journal of Bone and Joint Surgery 201193223–228. ( 10.1302/0301-620X.93B2.24760) [DOI] [PubMed] [Google Scholar]
- 57.Ring D Quintero J & Jupiter JB. Open reduction and internal fixation of fractures of the radial head. Journal of Bone and Joint Surgery 2002841811–1815. ( 10.2106/00004623-200210000-00011) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a