Abstract
Introduction
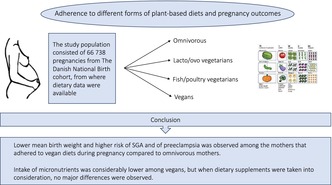
The number of people adhering to plant‐based diets has been increasing dramatically in recent years, fueled by both environmental and animal welfare concerns. Beneficial or possible adverse consequences of such diets, particularly the most restrictive forms during pregnancy, have been minimally explored. The aim of this prospective observational study was to examine associations between different forms of plant‐based diets during pregnancy with birth outcomes and pregnancy complications.
Material and methods
The Danish National Birth Cohort included 100 413 pregnancies to 91 381 women in 1996–2002. The population consisted of 66 738 pregnancies, about which sufficient dietary data were available and included in the study. Dietary and supplemental intake was assessed by Food Frequency Questionnaire in gestational week 25 and women were characterized as fish/poultry‐vegetarians, lacto/ovo‐vegetarians, vegans or omnivorous, based on their self‐report in gestational week 30. Main outcome measures were pregnancy and birth complications, birthweight and small for gestational age.
Results
A total of 98.7% (n = 65 872) of participants were defined as omnivorous, whereas 1.0% (n = 666), 0.3% (n = 183) and 0.03% (n = 18) identified themselves as fish/poultry vegetarians, lacto/ovo‐vegetarians or vegans, respectively. Protein intake was lower among lacto/ovo‐vegetarians (13.3%) and vegans (10.4%) than among omnivorous participants (15.4%). Intake of micronutrients was also considerably lower among vegans, but when dietary supplements were taken into consideration, no major differences were observed. Compared with omnivorous mothers, vegans had a higher prevalence of preeclampsia and their offspring had on average −240 g (95% confidence interval −450 to −30) lower birthweight.
Conclusions
The women reporting that they adhered to vegan diets during pregnancy had offspring with lower mean birthweight and higher risk of preeclampsia compared with omnivorous mothers. Low protein intake might be one plausible explanation for the observed association with birthweight.
Keywords: Danish National Birth Cohort, diet, pregnancy outcomes, vegans, vegetarians
Women adhering to vegan diets during pregnancy had offspring with a lower mean birth weight compared with omnivorous mothers. Further research is needed regarding possible causality between plant‐based diets and pregnancy and birth outcomes to strengthen the basis for dietary recommendations.
Abbreviations
- BMI
body mass index
- CI
confidence intervals
- FFQ
Food Frequency Questionnaire
- GDM
gestational diabetes mellitus
Key message.
Women adhering to vegan diets during pregnancy had offspring with lower mean birthweight compared to omnivorous mothers. Further research is needed regarding possible causality between plant‐based diets and pregnancy and birth outcomes to strengthen the basis for dietary recommendations.
1. INTRODUCTION
Interest in strict adherence to plant‐based diets such as veganism has been surging in many western societies and this trend has been fueled by environmental, ethical and animal welfare concerns (Interest in veganism is surging. The Economist [online]; Available online at: https://www.economist.com/graphic‐detail/2020/01/29/interest‐in‐veganism‐is‐surging [accessed September 10, 2023]). 1 In Denmark, the prevalence of veganism in the general population has gone from being barely measurable in 2010 (<1%) to around 3% in 2022, with higher prevalence (7.4%) reported among young adults aged 18–34 years. The prevalence may be even higher in the pregnant population, as 70% of the vegetarians in Denmark are women (Vegetarisk Forening. Statistik om vegetarisk levevis i Danmark. Available online at: https://vegetarisk.dk/statistik‐om‐danmark/ [accessed September 7, 2023]). Based on limited data, adherence to plant‐based diets has been associated with reduced all‐cause mortality, 2 but at the same time, in a systematic review comprising 48 studies including 12 000 vegans, risk of nutritional deficiency has been documented for the most restricted forms. 3
Several studies have examined associations between adherence to plant‐based diets and birth outcomes. A narrative review of studies published prior to 2015 found limited evidence for any adverse effects on maternal health or birth outcomes, for example noting that vegan diets had been associated with both lower and higher birthweight. 4 However, two recent studies from Israel comparing 60 vegans with 112 omnivorous mothers 5 and the USA comparing 32 vegetarians with 1256 omnivorous mothers 6 reported significantly lower birthweight (~200 g) and a higher prevalence of small for gestational age. It is possible that heterogeneity in diets among those following vegan diets 3 , 7 may explain divergent findings, but a major limitation of most previous studies is that information on nutrient intake of study participants is usually not recorded.
Public health guidelines aimed at those following strict forms of plant‐based diets during pregnancy are currently based on limited data and often appear conflicting. 8 , 9 To improve such guidelines, better characterization of dietary composition among those adhering to vegetarian and vegan diets is needed. The aim of this study was to compare dietary composition and quantity of consumed energy and macro‐ and micronutrients among women following different forms of plant‐based diets and to examine to what extent these diets might be associated with pregnancy outcomes. For this purpose, we used the large prospective Danish National Birth Cohort including more than 91 000 women.
2. MATERIAL AND METHODS
Between 1996 and 2002, a total of 91 381 pregnant women were recruited into the Danish National Birth Cohort. As women were allowed to enter the study repeatedly, the full cohort included 100 413 pregnancies, corresponding to around 35% of all births in Denmark. 10 Participants were recruited during their first antenatal visit to the general practitioner (gestational week ~6) after which they provided informed written consent. Detailed computer‐assisted telephone interviews on current and past lifestyle and health were conducted around gestational weeks 12 and 30; and in week 25, questions about maternal diet were recorded using a thorough semiquantitative Food Frequency Questionnaire (FFQ). 11
In the computer‐assisted telephone interview conducted in gestational week 30, women were asked the following question: “Are you a vegetarian?”; if they answered “yes” they were asked “What kind of vegetarian?” where the following options for response were “vegetarian + fish and poultry”, “vegetarian + milk, eggs (lacto/ovo‐vegetarian)”, “only diet from plants (vegan)” or “I do not know or I do not wish to answer”.
Prior to the interview in week 30, a paper and pencil food frequency questionnaire had been mailed to all women around gestational week 25. In this 360‐food item questionnaire, women were asked to record their habitual diet during the previous 4 weeks. After completion the women returned the questionnaire by mail. Frequency of intake reported for different food items was scaled to grams per day using assumptions on standard partition sizes. 12 The amount of energy macro‐ and micronutrients consumed was then quantified using the Danish Food Composition Tables 13 by aggregating the contribution from all food items. The FFQ has previously been validated against selected macro and micronutrients and individual food items using both 24‐hour recalls and biomarkers of nutrition status. 14 , 15 The FFQ also recorded information on food supplements and the amount of each nutrient was quantified based on the women's record of which supplements, supplement brand and average daily dosages during the previous 4 weeks. This information was linked to a database of existing dietary supplements sold in Denmark at the time.
Information on maternal birth outcomes and pregnancy complications were extracted from the National Birth Registry. These included information on birthweight, length, mode of delivery and length of gestation as well as pregnancy complications such as gestational diabetes (GDM) and preeclampsia. The registry‐based diagnoses of both GDM and preeclampsia cases in this cohort have been validated by expert panels through review of hospital records. 16 , 17 Information on maternal anemia, which was self‐reported, and other complications occurring during pregnancy was obtained from the computer assisted telephone interview conducted at gestational week 30. For further details regarding the questions included in interview carried out in week 30, see the Danish National Birth Cohort website (www.dnbc.dk/data‐available/interviews‐1–4 [accessed September 7, 2023]).
Of the 100 413 pregnancies recruited into the cohort, dietary information was available for 70 183 pregnancies. Of those, 1079 and 1590 pregnancies were excluded due to unrealistically low (≤4.5 MJ) or high (>25.0 MJ) energy intake and multiple pregnancies, respectively. In addition, 776 women did not participate in the telephone interview in gestational week 30 during which information on adherence to plant‐based diet was recorded. The final sample size therefore consisted of 66 738 women, or 66% of all pregnancies recruited into the study (but 95% of all those who filled out the FFQ).
Concerning influence of missing values and other exclusions, we found no differences (mean [standard deviation]) between those included in this study and those excluded with respect to maternal age (30.4 years [4.2] vs 30.4 years [4.5]) and pre‐pregnancy body mass index (BMI) (23.5 kg/m2 [4.2] vs 23.7 kg/m2 [4.4]). The prevalence of nulliparous women (49% vs 43%) and non‐smokers (76% vs 69%) was, however, slightly higher among those included into our study. Information regarding the possible influence of dropout in the Danish National Birth Cohort was investigated in previous studies and will not be described in detail here. 18
2.1. Statistical analyses
Continuous normally distributed variables were described using the mean and standard deviation, skewed variables were described using the median (10th–90th percentile) and dichotomous variables were described using percentages. To test differences between two groups for continuous variables, we used the t‐test and Mann–Whitney t‐test for normally distributed and skewed variables, respectively. For dichotomous variables, differences between groups were assessed using the Chi‐square test.
Associations between adherence to different plant‐based diets and birth outcomes were examined using multivariate‐logistic‐ and linear regression analyses for dichotomous and continuous outcomes, respectively. In these regression analyses, participants were classified as being omnivorous, fish/poultry vegetarian, lacto/ovo‐vegetarian or vegan. Adjusted mean differences for continuous birth outcomes, with 95% confidence intervals (CI), were estimated for those following the three different plant‐based diets relative to omnivores. Repeated entry into the cohort by the same women, though with different pregnancies (~10% of all pregnancies), were accounted for using PROC MIXED and PROC GENMOD in SAS for continuous and binary outcomes, respectively. In our analyses, the following set of covariates were included: maternal age, pre‐pregnancy BMI, smoking during pregnancy and parity. Further adjustment for offspring sex was made when examining associations with birthweight, length and length of gestation.
3. RESULTS
A total of 98.7% (n = 65 872) of study participants were defined as omnivorous, whereas 1.0% (n = 666), 0.3% (n = 183) and 0.03% (n = 18) identified themselves as fish/poultry vegetarians, lacto/ovo‐vegetarians or vegans, respectively (Table 1). Although formal statistical significance was not always reached, those adhering to plant‐based diets (all types) were slightly older and more likely to be parous and less likely to smoke. The prevalence of overweight and obesity (pre‐pregnancy BMI >25 kg/m2) was also somewhat lower and the prevalence of underweight higher (pre‐pregnancy BMI <18.5 kg/m2) among those adhering to plant‐based diets.
TABLE 1.
Maternal characteristics according to adherence to omnivorous or plant‐based diets (n = 66 739).
| Omnivorous (n = 65 872) | Vegetarian fish/poultry (n = 666) | Vegetarian lacto/ovo‐(n = 182) | Vegan (n = 18) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (standard deviation) or % | ||||||||
| Age, years | 30.4 | (4.2) | 30.81 | (4.5) | 30.7 | 30.7 | 30.81 | (4.5) |
| Height, cm | 168.8 | (6.1) | 169.0 | (6.1) | 169.2 | (6.1) | 169.1 | (7.0) |
| BMI, kg/m2 | 23.6 | (4.2) | 21.92 | (3.3) | 21.8 | 21.8 | 21.92 | (3.3) |
| BMI >25 | 27% | 14% | 18% | 18% | ||||
| BMI <18.5 | 4% | 9%2 | 9% | 6% | ||||
| Nulliparous | 48% | 61%2 | 60% | 61%2 | ||||
| Smoking | 24% | 19%2 | 15% | 19%2 | ||||
| Physically active | ||||||||
| Week 12 | 38% | 48%2 | 50% | 48%2 | ||||
| Week 30 | 32% | 46%2 | 49% | 46%2 | ||||
Note: 1 P < 0.05, 2 P < 0.01: t‐test for all continuous variables except gestational age (Mann–Whitney test), otherwise Chi‐square test for all dichotomous variables.
Total energy intake was modestly lower (mean difference: 0.3–0.7 MJ/day) among those adhering to plant‐based diets compared with omnivorous participants (Table 2). For lacto/ovo‐vegetarians and those following vegan diets, total protein intake was substantially lower, or 13.3% and 10.4% of energy, respectively, compared wth 15.4% among omnivorous participants. As expected, intake of carbohydrates was also higher among those adhering to plant‐based diets. For micronutrients, dietary intake of vitamin B12, vitamin D and calcium were lower among those adhering to plant‐based diets with a decreased level of intake with higher restriction (ie omnivorous > fish/poultry‐vegetarian > lacto/ovo‐vegetarians > vegan). However, when intake from dietary supplements was added to the dietary contribution (Table 3), the median intake of iron, vitamin B12, folic acid, calcium and other nutrients was well above the recommended nutrient intake 19 for most participants, independent of their diet. The only exception was the intake of vitamin D, where intake from food and supplements was below recommendations for vegans; only ~40% of vegans were above the recommendation compared with ~50% to 60% for the other food groups.
TABLE 2.
Dietary nutrient intake as recorded in gestation week 25 according to adherence to omnivorous or plant‐based diets.
| Omnivorous (n = 65 872) | Vegetarian fish/poultry (n = 666) | Vegetarian lacto/ovo (n = 182) | Vegan (n = 18) | |
|---|---|---|---|---|
| Macronutrients | Mean (standard deviation) | |||
| Energy, MJ/day | 10.4 (2.8) | 9.92 (2.7) | 10.1 (3.2) | 9.7 (2.5) |
| Protein, %E | 15.4 (2.4) | 14.72 (2.5) | 13.32 (2.3) | 10.41 (2.6) |
| Fat, %E | 32.3 (6.1) | 29.92 (6.6) | 29.72 (6.7) | 32.7 (5.7) |
| Carbohydrates, %E | 51.8 (5.9) | 55.12 (6.4) | 56.72 (6.5) | 56.7 (6.1) |
| Fiber, g/day | 27 (9) | 292 (11) | 302 (12) | 30 (11) |
| Micronutrients | Median (10th–90th percentile) | |||
| Retinol, μg/day |
645 (323–1219) |
3982 (210–793) |
424 (198–779) |
4192 (224–1146) |
| Beta‐carotene, μg/day |
2.1 (0.9–5.2) |
3.02 (1.3–9.0) |
3.1 (1.2–9.8) |
2.92 (1.1–1.6) |
| Folic acid, μg/day |
350 (237–498) |
3762 (252–541) |
376 (243–588) |
3792 (224–588) |
| Vitamin B12, μg/day |
6.4 (3.5–10.2) |
5.32 (2.7–9.5) |
4.32 (1.7–8.1) |
1.52 (0.4–6.9) |
| Vitamin D, μg/day |
3.3 (1.7–6.3) |
4.22 (1.5–9.0) |
1.72 (0.8–5.3) |
1.12 (0.3–5.5) |
| Calcium, g/day |
1.4 (0.8–2.1) |
1.32 (0.8–2.1) |
1.5 (0.8–2.2) |
0.92 (0.5–2.1) |
| Iron, mg/day |
11.4 (7.8–15.7) |
11.11 (7.7–15.9) |
11.2 (7.9–16.5) |
11.5 (7.8–17.0) |
| Iodine, μg/day |
268 (162–413) |
270 (149–427) |
275 (114–481) |
2221 (117–312) |
Note: 1 P < 0.05, 2 P < 0.01: t‐test for all macronutrients, otherwise Mann–Whitney test.
TABLE 3.
Maternal intake of micronutrients from foods and supplements as recorded in week 25 of gestation relative to recommended intake.
| Omnivorous (n = 65 872) | Vegetarian fish/poultry (n = 666) | Vegetarian lacto/ovo (n = 182) | Vegan (n = 18) | Recommended intake 1 | |
|---|---|---|---|---|---|
| Median (% above lower boundary of recommended intake) | |||||
| Vitamin A, IU | 1414 (90%) | 1274 (85%) | 1295 (85%) | 1326 (72%) | 800 |
| Folic acid, μg/day | 623 (67%) | 667 (72%) | 703 (72%) | 599 (61%) | 500 |
| Vitamin B12, μg/day | 10.4 (>99%) | 10.0 (99%) | 10.5 (93%) | 9.4 (89%) | 2 |
| Vitamin D, μg/day | 10.2 (51%) | 11.3 (59%) | 10.4 (52%) | 6.2 (39%) | 10 |
| Calcium, g/day | 1.5 (91%) | 1.5 (92%) | 1.6 (90% | 1.2 (72%) | 0.9 |
| Iron, mg/day | 63 (92%) | 51 (91%) | 53 (93%) | 35 (89%) | 15 2 |
| Iodine, μg/day | 381 (94%) | 381 (94%) | 393 (93%) | 332 (72%) | 200 |
Nordic Nutrition Recommendation 2023 recommendations for pregnant women. 19
No value set for pregnant women as individual monitoring of iron status applies. Value used here is for lactating women.
Mean birthweight, birth length, length of gestation and prevalence of low birthweight (<2500 g) were similar among omnivorous, fish/poultry‐ and lacto/ovo‐vegetarians (Table 4). The prevalence of GDM, preeclampsia and cesarean section was also similar across these three groups but the prevalence of anemia was higher among fish/poultry‐ and lacto/ovo‐vegetarians than omnivorous participants. The offspring of vegan mothers had lower mean birthweight compared with offspring of omnivorous mothers (3441 vs 3601 g) and the mean length of gestation was around 5 days longer. Vegan mothers had a higher prevalence of having an infant with low birth weight (11.1% vs 2.5%) and of preeclampsia (11.1% vs 2.6%) compared omnivorous mothers, but this comparison needs to be interpreted in the context of low number of vegan participants.
TABLE 4.
Pregnancy outcomes according to adherence to omnivorous or plant‐based diets.
| Birth outcomes | Omnivorous (n = 65 872) | Vegetarian fish/poultry (n = 666) | Vegetarian lacto/ovo (n = 182) | Vegan (n = 18) |
|---|---|---|---|---|
| Mean (standard deviation) or % | ||||
| Birthweight, g | 3601 (544) | 3571 (527) | 3617 (499) | 3441 (558) |
| z‐score for birthweight | 0.00 (0.00) | −0.11 (1.01) | 0.07 (0.92) | −0.56 (0.87) |
| Birth length, cm | 52.3 (2.6) | 52.4 (2.4) | 52.5 (2.3) | 52.5 (2.6) |
| Gestational age, days | 280.6 (11.9) | 281.4 (10.9) | 280.3 (10.8) | 285.6 (9.9)2 |
| Low birthweight <2500 g, | ||||
| % [no. cases/N] | 2.5% [1623/65549] | 2.3% [15/662] | 2.3% [4/178] | 11% [2/18]1 |
| Small for gestational age,3 | ||||
| % [no. cases/N] | 9.9% [6502/65549] | 11.9% [79/662] | 7.3% [13/178] | 27.8% [5/18] |
| Male infants, | ||||
| %, [no. cases/N] | 51.3% [33 792/65872] | 51.7% [344/666] | 50.6% [92/182] | 38.9% [7/18] |
| Spontaneous delivery, | ||||
| %, [no. cases/N] | 67.9% [44 421/65422] | 68.2% [451/661] | 68.3% [123/180] | 66.7% [12/18] |
| Induced labor, | ||||
| % [no. cases/N] | 32.1% [20 870/65039] | 7.4% [47/632] | 4.2% [7/167] | 16.7% [3/18] |
| Cesarean section, | ||||
| % [no. cases/N] | 15.3% [9917/65039] | 14.6% [92/632] | 14.4% [24/167] | 5.6% [1/18] |
| Iron deficiency before week 30, | ||||
| % [no. cases/N] | 7.7% [4993/65228] | 12.8% [85/665]2 | 13.8% [25/1841]2 | 5.6% [1/18] |
| GDM, | ||||
| % [no. cases/N] | 0.8% [512/65872] | 0.5% [3/666] | 0.6% [1/182] | 0% [0/18] |
| Preeclampsia, | ||||
| % [no. cases/N] | 2.6% [1680/65872] | 3.0% [20/666] | 2.2% [4/182] | 11.1%1 [2/666] |
Note: 1 P < 0.05, 2 P < 0.01: t‐test for all continuous variables except gestational age (Mann–Whitney test), otherwise Chi‐square test for all dichotomous variables. 3Birthweight >10th percentile for gestational age.
After covariate adjustment, offspring of vegan mothers had on average a birthweight 240 g lower (95% CI −450 to −30) and a gestation 5.2 days longer (95% CI −0.2 to 10.7) compared with offspring of omnivorous mothers, leading to a significant lower birthweight z‐score: −0.50 (−0.96 to −0.03) (Table 5).
TABLE 5.
Adjusted associations between adherence to omnivorous or plant‐based diets and selected pregnancy and birth outcomes.
| Omnivorous (n = 65 872) | Vegetarian fish/poultry (n = 666) | Vegetarian lacto/ovo (n = 182) | Vegan (n = 18) | |
|---|---|---|---|---|
| Mean difference (95% confidence interval) a | ||||
| Birthweight, g | Referent | −15 (−50 to 19) | 34 (−35 to 98) | −240 (−450 to −30) |
| z‐score for birthweight | Referent | −0.05 (−0.13 to 0.03) | 0.08 (−0.07 to 0.23) | −0.50 (−0.96 to −0.03) |
| Birth length, cm | Referent | −0.0 (−0.2 to 0.2) | 0.1 (−0.2 to 0.5) | −0.3 (−1.3 to 0.7) |
| Gestational age, days | Referent | 1.0 (0.1 to 1.9) | −0.2 (−1.9 to 1.5) | 5.2 (−0.2 to 10.7) |
Adjusted for offspring sex, maternal age, pre‐pregnancy body mass index, smoking during pregnancy and parity.
4. DISCUSSION
In this large cohort of Danish pregnant women recruited between 1996 and 2002, those who reported to adhere to vegan diets had offspring with a significantly lower mean birthweight, a higher prevalence of being small for gestational age (and of low birthweight [<2500 g]) compared with omnivorous women. The prevalence of preeclampsia was also higher. Overall, no differences in birth and pregnancy complications were observed between fish/poultry vegetarians, lacto/ovo‐vegetarians and omnivorous mothers, with the exception that the prevalence of anemia was higher in the first two groups.
Although our results suggest a higher risk of low birthweight (<2500 g) and preeclampsia among vegans, these findings are subject to some uncertainty given the small number of vegans in our study (n = 18). However, our sample size was still sufficient to detect meaningful differences in continuous birth outcomes such as birthweight. The lower birthweight of around 240 g among vegans compared with omnivorous mothersin our study, strengthens our observation that vegans may be at higher risk of giving birth to low birthweight infants. The observed effect size on birthweight is comparable to what is observed among daily smokers relative to non‐smokers in this cohort. 20 Furthermore, the on‐average ~5‐day longer gestation observed among vegans in our study would be indicative of reduced fetal growth rate rather than lower birthweight due to shorter gestation.
Similar findings reporting ~200 g mean lower birthweight among vegans compared with omnivorous participants have been reported in two recent studies, one from Israel where 60 vegans were compared with 112 omnivorous womwn, 5 and one from the USA including 32 full‐vegetarians. 6 In those two studies the number of vegans was higher; however, “full‐vegetarians” can include both vegans and lacto/ovo‐vegetarians. Both studies also reported a significantly increased risk of small for gestational age, which has also been reported in a retrospective web‐based study from 2017 including 234 vegans. 21 These results along with ours provide quite consistent evidence suggesting that adherence to vegan diets during pregnancy may adversely affect fetal growth. Previous studies have explored the relationship between adherence to plant‐based diets and weight control. Adopting a vegetarian diet is a possibility to legitimate restrictive eating and the studies concluded that adherence to plant‐based diets could be an expression of weight control or even indication of eating disorders such as anorexia. 22 , 23 However, when asked specifically about eating disorders, none of the women following vegan diets in our study answered yes to that question.
Leaving the findings on vegans aside, it is reassuring that there was no indication in our study of any adverse birth outcomes or pregnancy complications for the less restrictive lacto/ovo‐vegetarians, which shared some of the same dietary characteristics of vegans, particularly low protein and vitamin D. Similarly, no sign of any adverse associations was observed for the fish/poultry vegetarians, who had largely similar nutrient profile as omnivorous participants. For both lacto/ovo‐ and fish/poultry vegetarians, our sample size was relatively large compared with other studies and would have allowed us to detect modest associations with, for example, birthweight.
Concerning what dietary or behavioral characteristics of vegans might explain lower birthweight, previous studies have noted lower gestational weight gain among vegan compared with omnivore mothers. 5 , 6 , 21 Although gestational weight gain is a strong predictor of birthweight, 24 it is only an indirect marker reflecting dietary, lifestyle and general health of the mother. Previous studies 5 , 6 , 21 as well as our study found no indications of unhealthier lifestyles such as smoking, alcohol consumption or sedentary behavior among vegan mothers, making differences in dietary habits a more plausible explanation. Nutritional deficiencies including inadequate vitamin B12, iron, zinc calcium and iodine status have been noted among vegans, 3 , 6 , 7 which may potentially affect fetal growth. However, although dietary intake of some vitamins and minerals such as vitamin B12, iodine and calcium was indeed lower among vegans compared with omnivorous participants in our study, once intake from supplements was taken into consideration, total micronutrient intake was largely in line with recommended intakes. 19
A more plausible explanation for lower birthweight among vegan mothers might be low protein intake. The mean protein intake as percentage of energy in our study was 10.4% (or 56 g/day) and 15.4% (or 89 g/day) among vegan and omnivorous mothers, respectively. Similar differences (~50 vs 90 g protein per day) was reported among full‐vegetarians and omnivorous in the USA. 6 The current recommended intake of protein for adults, including pregnant women, in Denmark is 10%–20% of energy, which corresponds to about 0.8–1.5 g protein/kg bodyweight/day. 19 With mean protein intake being only 10.4% of energy in our study, around half of our vegan participants were below current recommendations. Furthermore, in a large combined and prospective analyses of 126 443 mothers from the Danish National Birth Cohort and the Norwegian Mother and Child Cohort Study, we have previously reported a higher relative risk of low birthweight (1.6 [95% CI 1.3–2.0]) among 1368 mothers who had a protein intake >60 g/day compared with 42 536 mothers who had protein intake between 80 and 90 g/day. 25 Similarly, lower birthweight has been observed among women following diets that were low in protein such as macrobiotic diets. 26 Evidence from interventions providing balanced protein supplementation have also been suggestive of a protective effect on intrauterine growth retardation. 27
Our findings on higher prevalence of preeclampsia among vegan than omnivorous mothers require careful interpretation given the number of vegan participants in our study and the fact that two previous studies, with a larger sample size of vegans, have not found any indication of hypertensive disorders during pregnancy among vegans. 5 , 6 Although some studies have suggested a link between low protein intake, calcium or vitamin D and preeclampsia, the overall evidence for such a relationship is at best inconsistent 28 and our findings would need replication before stronger conclusions can be drawn.
In all the vegetarian and vegans there was a low prevalence of GDM. As for the prevalence of preeclampsia, the results are limited because of a small sample size. The low prevalence of GDM could also be partly explained by the definition of GDM used in the Danish National Birth Cohort, as the diagnostic criteria for GDM that are still used today were introduced in 2003. Furthermore, there was a self‐selection of healthier women to the cohort. 17
The main strength of our study is the prospective design collecting detailed information on both diet and supplemental use in mid‐pregnancy by a comprehensive questionnaire, combined with an additional, separate recorded interview of the woman's own explicit statement of the type of diet she adhered to during pregnancy. As a result, we could with some level of detail characterize the diets of women reporting following different plant‐based diets and compare them with omnivorous mothers. The main limitation of our study, however, is that the number of vegan pregnancies was extremely low (0.03%; 18 women) relative to the total sample size. Also, being vegan when recruited into the cohort in 1996–2002 may reflect different habits compared with those following vegan diets today. On the other hand, our findings on lower birthweight are consistent with more recent studies 5 , 6 , 21 and the low intake of proteins and other micronutrients is in line with what has been reported in other more recent studies. 3 , 6 , 7
5. CONCLUSION
In a large prospective study of Danish pregnant women recruited between 1996 and 2002, we observed a lower mean birthweight among the few mothers who adhered to vegan diets during pregnancy compared with omnivorous mothers. We acknowledge that finding an association in an observational study cannot lead to conclusions on causality. But future studies should put more emphasis on characterizing the diet among those adhering to vegan diets and other forms of plant‐based diets during pregnancy. This would allow for stronger assumptions on possible causality between any association observed with birth or pregnancy outcomes in such studies and strengthen the basis for dietary recommendations.
AUTHOR CONTRIBUTIONS
Signe Hedegaard, Ellen Aagaard Nohr, Sjurdur Frodi Olsen, Thorhallur Ingvi Halldorsson and Kristina Martha Renault conceived and designed the study. Thorhallur Ingvi Halldorsson extracted and analyzed the data and drafted the tables. Signe Hedegaard, Thorhallur Ingvi Halldorsson and Kristina Martha Renault interpreted the data and wrote the orginal draft. Ellen Aagaard Nohr and Sjurdur Frodi Olsen undertook critical revision. All authors approved the final paper.
FUNDING INFORMATION
Danish Council for Independent Research, Grant/Award Number: DFF – 4183‐00152 and DFF – 4183‐00594. The Danish National Birth Cohort Study and its dietary component has been supported by the March of Dimes Birth Defects Foundation (6‐FY‐96‐0240, 6‐FY97‐0553, 6‐FY97‐0521, 6‐FY00‐407), the Danish Heart Association, Danish Medical Research Council, Sygekassernes Helsefond, Innovation Fund Denmark (Grant No. 09‐067124) and the Danish National Research Foundation.
CONFLICT OF INTEREST STATEMENT
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ETHICS STATEMENT
All participants provided written informed consent. The Danish National Birth Cohort was approved by the Scientific Ethic Committee in Denmark on August 8, 1995 (case no. [KF] 01–471/94) and the Danish Data Protection Agency (ref. no 2008‐54‐0431), which also approved the present study.
Hedegaard S, Nohr EA, Olsen SF, Halldorsson TI, Renault KM. Adherence to different forms of plant‐based diets and pregnancy outcomes in the Danish National Birth Cohort: A prospective observational study. Acta Obstet Gynecol Scand. 2024;103:1046‐1053. doi: 10.1111/aogs.14778
REFERENCES
- 1. Leitzmann C. Vegetarian nutrition: past, present, future. Am J Clin Nutr. 2014;100:496‐502. [DOI] [PubMed] [Google Scholar]
- 2. Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393:447‐492. [DOI] [PubMed] [Google Scholar]
- 3. Bakaloudi DR, Halloran A, Rippin HL, et al. Intake and adequacy of the vegan diet. A systematic review of the evidence. Clin Nutr. 2021;40:3503‐3521. [DOI] [PubMed] [Google Scholar]
- 4. Piccoli GB, Clari R, Vigotti FN, et al. Vegan—vegetarian diets in pregnancy: danger or panacea? A systematic narrative review. BJOG. 2015;122:623‐633. [DOI] [PubMed] [Google Scholar]
- 5. Avnon T, Paz Dubinsky E, Lavie I, Ben‐Mayor Bashi T, Anbar R, Yogev Y. The impact of a vegan diet on pregnancy outcomes. J Perinatol. 2021;41:1129‐1133. [DOI] [PubMed] [Google Scholar]
- 6. Yisahak SF, Hinkle SN, Mumford SL, et al. Vegetarian diets during pregnancy, and maternal and neonatal outcomes. Int J Epidemiol. 2021;50:165‐178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Waldmann A, Koschizke JW, Leitzmann C, Hahn A. Dietary intakes and lifestyle factors of a vegan population in Germany: results from the German vegan study. Eur J Clin Nutr. 2003;57:947‐955. [DOI] [PubMed] [Google Scholar]
- 8. Melina V, Craig W, Levin S. Position of the academy of nutrition and dietetics: vegetarian diets. J Acad Nutr Diet. 2016;116:1970‐1980. [DOI] [PubMed] [Google Scholar]
- 9. Richter M, Boeing H, Grünewald‐funk D, et al. Vegan diet. Ernahrungs Umschau. 2016;63:92‐102. [Google Scholar]
- 10. Olsen J, Melbye M, Olsen SF, et al. The Danish National Birth Cohort—its background, structure and aim. Scand J Public Health. 2001;29:300‐307. [DOI] [PubMed] [Google Scholar]
- 11. Olsen SF, Mikkelsen TB, Knudsen VK, et al. Data collected on maternal dietary exposures in the Danish National Birth Cohort. Paediatr Perinat Epidemiol. 2007;21:76‐86. [DOI] [PubMed] [Google Scholar]
- 12. Andersen LT, Jensen H, Haraldsdóttir J. Typiske vægte for madvarer. Scand J Nutr. 1996;40:29‐51. [Google Scholar]
- 13. Food data (frida.fooddata.dk), version 4.2, 2022. National Food Institute, Technical University of Denmark.
- 14. Mikkelsen TB, Osler M, Olsen SF. Validity of protein, retinol, folic acid and n–3 fatty acid intakes estimated from the food‐frequency questionnaire used in the Danish National Birth Cohort. Public Health Nutr. 2006;9:771‐778. [DOI] [PubMed] [Google Scholar]
- 15. Mikkelsen TB, Olsen SF, Rasmussen SE, Osler M. Relative validity of fruit and vegetable intake estimated by the food frequency questionnaire used in the Danish National Birth Cohort. Scand J Public Health. 2007;35:172‐179. [DOI] [PubMed] [Google Scholar]
- 16. Klemmensen ÅK, Olsen SF, Østerdal ML, Tabor A. Validity of preeclampsia‐related diagnoses recorded in a national hospital registry and in a postpartum interview of the women. Am J Epidemiol. 2007;166:117‐124. [DOI] [PubMed] [Google Scholar]
- 17. Olsen SF, Houshmand‐Oeregaard A, Granström C, et al. Diagnosing gestational diabetes mellitus in the Danish National Birth Cohort. Acta Obstet Gynecol Scand. 2017;96:563‐569. [DOI] [PubMed] [Google Scholar]
- 18. Nohr EA, Frydenberg M, Henriksen TB, Olsen J. Does low participation in cohort studies induce bias? Epidemiology. 2006;17:413‐418. [DOI] [PubMed] [Google Scholar]
- 19. Fogelholm M, Sc D. Nordic Nutrition Recommendations 2012. Norden; 2012. [Google Scholar]
- 20. Brix N, Ernst A, Lauridsen LLB, et al. Maternal smoking during pregnancy and timing of puberty in sons and daughters: a population‐based cohort study. Am J Epidemiol. 2019;188:47‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kesary Y, Avital K, Hiersch L. Maternal plant‐based diet during gestation and pregnancy outcomes. Arch Gynecol Obstet. 2020;302:887‐898. [DOI] [PubMed] [Google Scholar]
- 22. O'Connor MA, Touyz SW, Dunn SM, Beumont PJ. Vegetarianism in anorexia nervosa? A review of 116 consecutive cases. Med J Austral. 1987;147:540‐542. [DOI] [PubMed] [Google Scholar]
- 23. Gilbody SM, Kirk SFL, Hill AJ. Vegetarianism in young women: another means of weight control? Int J Eating Disord. 1999;26:87‐90. [DOI] [PubMed] [Google Scholar]
- 24. Frederick IO, Williams MA, Sales AE, Martin DP, Killien M. Pre‐pregnancy body mass index, gestational weight gain, and other maternal characteristics in relation to infant birth weight. Matern Child Health J. 2008;12:557‐567. [DOI] [PubMed] [Google Scholar]
- 25. Halldorsson TI, Birgisdottir BE, Brantsæter AL, et al. Old question revisited: are high‐protein diets safe in pregnancy? Nutrients. 2021;13:1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dagnelie PC, van Staveren WA, van Klaveren JD, Burema J. Do children on macrobiotic diets show catch‐up growth? A population‐based cross‐sectional study in children aged 0–8 years. Eur J Clin Nutr. 1988;42:1007‐1016. [PubMed] [Google Scholar]
- 27. de Onis M, Villar J, Gülmezoglu M. Nutritional interventions to prevent intrauterine growth retardation: evidence from randomized controlled trials. Eur J Clin Nutr. 1998;52:83‐93. [PubMed] [Google Scholar]
- 28. Xu H, Shatenstein B, Luo ZC, Wei S, Fraser W. Role of nutrition in the risk of preeclampsia. Nutr Rev. 2009;67:639‐657. [DOI] [PubMed] [Google Scholar]