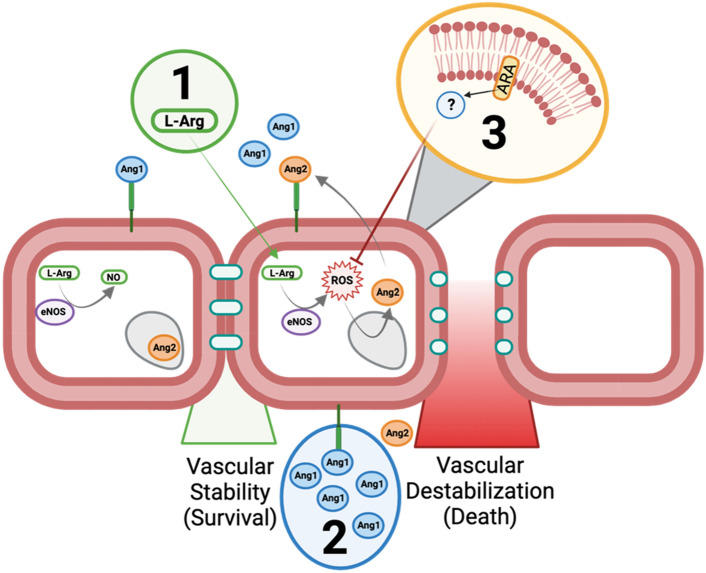
Figure 5.
Proposed model of enhancing vascular resilience in neonatal sepsis via 3 complementary strategies. During the steady state, vascular integrity is maintained by sequestration of Ang2 within intracellular vesicles. eNOS remains coupled to the cellular membrane, and converts L-Arg into NO. During the septic inflammatory response, eNOS is uncoupled from the cellular membrane and converts L-Arg into ROS. ROS releases Ang2 from within the endothelial cell which outcompetes Ang1 from binding to the TIE2 receptor. The Ang2:TIE2 complex triggers the release of tight junctions and causes vascular instability. Vascular resilience was enhanced through three avenues: (1) L-Arg supplementation ensured that eNOS could access sufficient substrate to generate NO instead of ROS, improving survival outcomes. (2) Exogenous Ang1 ensures a more favorable Ang1:Ang2 ratio which led to decreased levels of ROS improving survival. (3) Oral supplementation with ARA prior to challenge resulted in decreased levels of ROS in the liver during sepsis (via a still unknown mechanism), while increasing levels of plasma Ang1 and improving survival outcomes. L-Arg L-arginine, NO nitric oxide, eNOS endothelial nitric oxide synthase, Ang1 angiopoetin-1, Ang2 angiopoetin-2, ROS reactive oxygen species, ARA arachidonic acid. This image was created using Biorender.