Fig. 1.
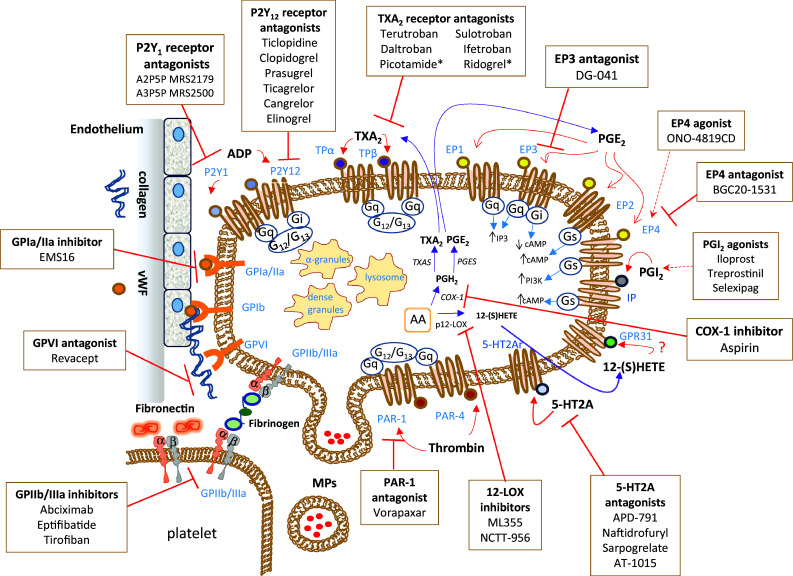
Platelet structure, primary receptors, eicosanoid machinery, and targeted therapeutics. Platelets are involved in the release of many mediators that are stored in different granules in the cytoplasm and microvesicles. A plethora of proteins are contained in α-granules; there are cell adhesion proteins, blood clotting factors, growth and angiogenic factors. The plasma membrane of platelets expresses several transmembrane receptors, involved in the crosstalk with other platelets and different cell types. Platelets adhere to the damaged vascular endothelium through the binding of integrin receptors (GP, glycoproteins) to the extracellular matrix proteins, such as collagen and VWF (von Willebrand factor). Possible strategies to inhibit the adhesion of platelets to a damaged endothelium involve the use of agents that interact with collagen binding sites, such as revacept, thus preventing the activation of the collagen receptors GPIa/IIa and GPVI expressed on the plasma membrane of platelets. Platelet aggregation, mediated by the binding of fibrinogen or fibronectin to GPIIb/IIIa on agonist-stimulated platelets, is inhibited by different antagonists of the GPIIb/IIIa receptor (abciximab, eptifibatide, and tirofiban). The activation of platelets by ADP (adenosine diphosphate) is mainly affected by antagonists of the P2Y12 receptor, among them, there is the pro-drug clopidogrel. An important antiplatelet agent is aspirin, which irreversibly inhibits the activity of cyclooxygenase (COX)-1 involved in the production of prostaglandin (PG) H2 that is then converted to the potent pro-aggregatory agent thromboxane (TX)A2 by the activity of TXA2 synthase (TXAS). A secondary product of COX-1-dependent pathway is PGE2 produced by the activity of different PGE synthases (PGES). TXA2 and PGE2 cause different platelet responses by the interaction with specific receptors. Various receptor antagonists in clinical development are reported. Picotamide and ridrogrel act by a dual mechanism involving the blockage of TP receptors and the inhibition of TXAS. There are four different receptors for PGE2 on the platelet surface: EP1, EP2, EP3 and EP4. The stimulation of EP3 leads to platelet activation, and specific antagonists are under clinical development, including DG-041. EP4 and EP2 signaling may increase intraplatelet cAMP (cyclic adenosine monophosphate) levels and thus possibly counteracting the platelet activation by EP3. Some agonists and antagonists of these receptors have been synthesized. An important receptor present on the platelet plasma membrane is the IP receptor for prostacyclin (PGI2), for which different commercially available agonists have been developed (Iloprost, Treprostinil, Selexipag). Another abundant eicosanoid produced by platelets is 12(S)-HETE [12(S)-hydroxyeicosatetraenoic acid] via the activity of the platelet-type lipoxygenase (p12-LOX). The mechanism of action is 12-(S)HETE has not been entirely understood. Recently, it has been proposed the activation of the orphan receptor GPR31 by 12-(S)HETE. The discovery of selective inhibitors of 12-LOX, such as ML355, will allow enhancing our knowledge of the role played by 12-LOX in health and disease. Protease-activated receptors (PARs) are involved in platelet activation by thrombin. There are two receptors, known as PAR-1 and PAR-4. However, PAR-1 possesses a higher affinity for thrombin. The PAR-1 antagonist vorapaxar was approved for clinical use in 2014. New antiplatelet agents include serotonin receptor antagonists (5-HT2A antagonists)
