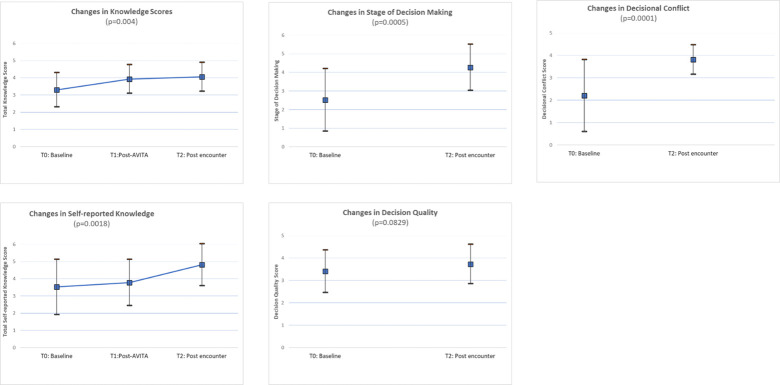
Fig 3. For all included outcomes, higher scores are desirable; higher decisional conflict scores reflect less decisional conflict (desirable).
S2 Table in S1 File reports these longitudinal findings. Self-reported knowledge scores similarly improved from 3.52 [1.60] at T0 to 3.78 [1.34] at T1 and 4.82 (1.22) at T2 (p = 0.0018) [linear mixed-effects model]. Actual and perceived knowledge were uncorrelated at T0 (R = -0.017, p = 0.932) but strongly correlated at T2 (R = 0.507; p = 0.016). Patients’ stage of decision-making significantly improved, with more patients moving closer to deciding (mean 2.52 [1.68] at T0 vs 4.27 [1.24] at T2, p = 0.0005) [paired t-test] (Fig 3). Decisional conflict significantly improved from 2.21 [1.61] at T0 to 3.82 [0.66] at T2 (p = 0.0001) [paired t-test], corresponding to fewer people (2/22 [9.09%]) experiencing decisional conflict at T2 compared to T0 (19/29 [65.52%]. Decisional quality improved from 3.41 [0.95] at T0 to 3.73 [0.88] at T2 (p = 0.083) [paired t-test]. At T0, all patients reported that they wanted to participate at least partially in decision-making; no patient wanted to leave treatment decisions to their clinician. Clinicians accurately judged their patient’s role preference in 11/28 [39.3%] encounters, overestimated their patient’s reliance on clinician’s judgement in 11/28 [39.3%] encounters, and underestimated it in 5/28 [17.9%] (S8 Fig in S2 File). Agreement between patient-reported role preferences and clinician judgement of patients’ preferred role was low (Kappa = 0.217 [95% CI -0.078–0.512]).