Abstract
Management of urethral sounding related injuries continues to be a challenge due to the wide breath of objects implicated, the rarity of cases, and chance of significant complication. We present a particularly challenging and novel case where a patient inserted a round of live ammunition into his urethra. Non-surgical removal was limited over concern for accidental discharge of the round, and the patient was taken to the operating room where open removal was performed. Psychiatric evaluation should be considered for cases where sounding injury requires surgical intervention, and a patient-centered, prevention-focused approach is best for building physician-patient rapport and adherence.
Keywords: Urethral sounding, Foreign body retention, Reconstruction, Live firearm round
1. Introduction
Non-medical urethral sounding is the act of inserting objects into the urethra and is primarily conducted for sexual gratification.1,2 These objects come in a wide array, including surgical sounds, household items (speaker wire, AAA batteries, open safety pins, a plastic cup, straws, marbles, razors, plastic utensils) plants, and various fluids.3,4 Little is known about the epidemiology of sounding, possibly due to a real or perceived stigma. One study investigating a population of 2122 men who have sex with men (MSM) reported that 10.7 % of participants had engaged in sounding at some point in their lifetime.2 Compared to peers, those who engaged in sounding from this population had an increased risk of STIs and were more likely to engage in high-risk sex behaviors.2 Sounding in women seems to be much less common – a study at a single American institution found that of 27 patients who presented with sounding-related injuries over 15 years, only one was a woman.5
Sounding-related injuries requiring medical intervention are rare, however significant complications can occur, including foreign body retention within the urethra or bladder, urethral injury, infection, and bleeding.3 Additional presenting symptoms can include dysuria, increased urinary frequency, pelvic pain, and urinary obstruction.3,6 The act of object insertion can also cause mucosal tears and false passages of the urethra. Multiple or repetitive urethral insertions are correlated with the formation of strictures, false passages, and mucosal tears.3,5 Because of the associated social stigma, patients may be reluctant to seek prompt medical treatment, and attempts to remove the object themselves may contribute to the injury.3 Patient reluctance can also significantly delay presentation, and calcifications can form on the surface of the object, worsening symptoms and complicating removal.3 Additionally, people who engage in sounding are prone to bacterial infection.6 Bacteria from unsterilized inserted objects can easily cross the urethra's submucosa and enter the vasculature of the corpus spongiosum.4 Long-term sounding may lead to abscesses, calculus formation, urethral diverticula, strictures, or fistula formation.1,6
Given the rare nature of urethral sounding, we seek to add to the known literature with a contemporary review of management strategies as well as present a particularly unique challenge of a patient who required surgical intervention due to sounding with live ammunition. In that context, we also review different ammunition types and specific considerations with regards to their handling.
2. Case report
We present the case of a 21-year-old male with no significant past medical history, who was transferred to our institution from an outside hospital. Twenty-four hours prior to his transfer, patient had inserted a single 0.223 caliber cartridge into his urethra. The patient had attempted to manually retrieve the cartridge following insertion but was unsuccessful despite multiple attempts. He admitted a recent history of urethral sounding but explained that this cartridge constituted the widest object he had attempt to pass. The patient also explained that this was live ammunition, and the primer end (tail) (Fig. 1) was closer to the meatus, advising against clamping on this location.
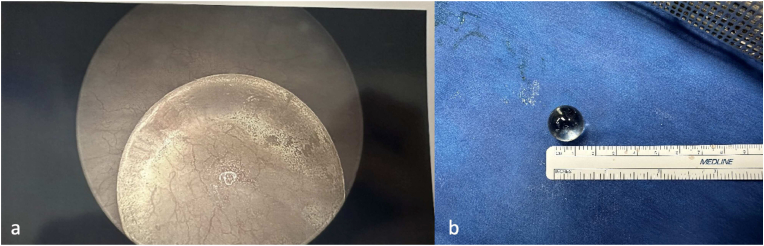
Fig. 1.
A: Visualization of the back of the cartridge through the meatus. B: Exposure of the proximal cartridge via ventral urethrotomy. C: Delivery of the intact cartridge. D: Blank round (cartridge) removed with labeled components.10
The patient had no voiding complaints and minimal post-residual volume. Patient otherwise denied any constitutional symptoms or hematuria. On examination, patient was hemodynamically stable. Physical exam revealed a circumcised penis with a cartridge in the distal urethra, positioned with the primer end closest to the meatus. (Fig. 1a). The cartridge had been completely pushed into the urethra, with no portion remaining externalized to allow simple removal.
Non-surgical intervention was attempted at the bedside via use of a Zero Tip stone retrieval basket. Despite positioning the basket proximal to the head of the attempts at removal were unsuccessful, likely due to the width of the cartridge's tail precluding exit through the meatus and difficulty engaging a cartridge of this caliber with the basket. Given the concern for possible accidental discharge of the ammunition while still in situ, the decision was made to limit further bedside retrieval maneuvers. For the safety of patient and staff the decision was made to take the patient to the operating room for open removal.
The cartridge was estimated to be 5 cm long with the tip palpable in the mid to distal urethra. A vertical incision was made on the ventral aspect over the site of the cartridge (Fig. 1b). The tissue was dissected sharply (avoiding electrocautery) down to the cartridge itself, and the incision was then extended until the tip was visualized, and gentle retrieval was possible (Fig. 1c and d). In total, the ventral urethral opening was 2 cm in length. A multilayered closure of the urethra and surrounding structures was then performed over a 22 French male sound. A 14 French foley catheter placed for drainage. Follow up retrograde urethrogram showed no extravasation.
3. Management of retained sounding objects
Perhaps the most pressing and challenging management of urethral sounding is the removal of retained objects. To avoid further damage by manipulation and catheterization by medical professionals, the object should be accurately sized and localized before removal is attempted.3 This can be achieved at least in part by detailed physical exam, with added information gleaned from ultrasound or plain radiograph for radiopaque objects.7 This imaging may assist the provider in identifying likely complications or hematomas. Endoscopic retrieval of the retained object under general, or local anesthesia by a urologist, is possible the majority of the time.3,4,8 Endoscopic retrieval of small, inert objects such as a marble (Fig. 2) can be retrieved safely. However occasionally urethrotomy or cystotomy may be required particularly for large objects (Fig. 3).3,4 Occasionally extrinsic pressure or voiding may be sufficient to ‘expel’ the foreign body.5 Because of the increased risk of infection, a broad-spectrum antibiotic should be initiated before removal.3,4
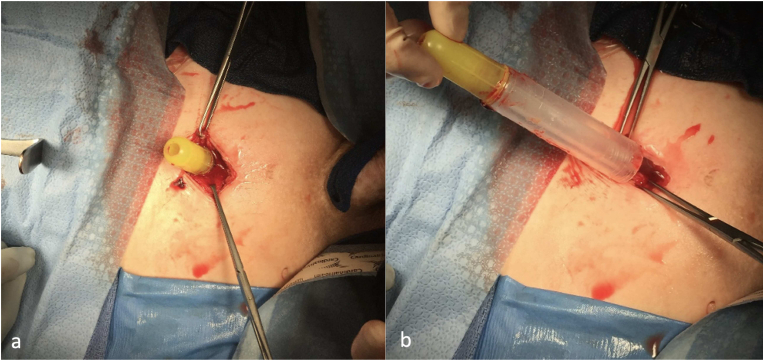
Fig. 2.
A: Marble within otherwise normal bladder on cystoscopy. B: Removed Marble.
Fig. 3.
A: Lidocaine applicator within the bladder identified on open cystotomy. B: Lidocaine applicator removed intact.
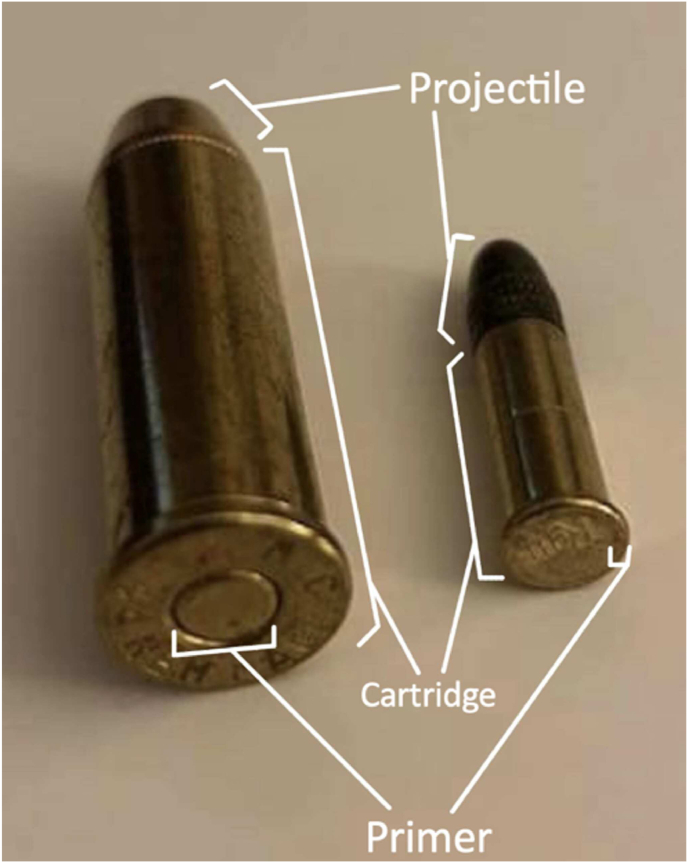
In this case, the potential explosive component provides a particular challenge. Because of the risk of discharge while extracting a live round from the urethra, it is important to understand the relative danger of manipulating the various parts of the cartridge. The components of a cartridge (Fig. 1d) are the projectile (bullet), case, propellant, and ignition (primer).9,10 The primer, or the part of the cartridge that ignites the propellant when struck, is the part of the round that should be approached with the most caution. There are two modern types of primer for a cartridge: rimfire and centerfire.11 (Fig. 4) The cartridge in this case was a centerfire and had the classic bull's eye appearance. A centerfire cartridge is discharged when a firing pin strikes the primer at the center of the cartridge's tail end. As in this case, the primer may be a different color than the rest of the cartridge case as it must be a softer metal to allow for compression from firing pin impact. Thus, the sides are safer to grasp when extracting a centerfire cartridge as it is less likely to discharge from manipulation here. The other type of cartridge is rimfire, where the primer that is struck by the firing pin is located around the edge of the tail of the cartridge. Rimfire cartridges are used in smaller caliber projectiles (0.22s and smaller) since the casing metal must be thin enough to be deformed by the firing pin.9,12 Thus, if a rimfire cartridge needed to be removed from a patient's body, only the front of the cartridge should be grasped with instruments. A blank round—a cartridge without the projectile, while generally safer than loaded ammunition, is still explosive and can be dangerous. Given the patient report that this was a live cartridge, the amount of safe manipulation was uncertain.
Fig. 4.
Comparison of fired rimfire and centerfire cartridges.10
The primer end of the cartridge is particularly dangerous as manipulation may lead to accidental discharge. Furthermore, instruments with rubber ends may be used out of an abundance of caution, for better grip preventing slippage and accidental discharge. Of great concern is that since the cartridge is not contained within the barrel of a firearm, the metal casing will get blown out circumferentially and may send shrapnel into the surrounding tissue. In the case of a bulleted round, the projectile would still be launched forward, but with less force than when fired from inside a barrel, where all the force of the explosion would be channeled in a single direction. This, as well as cartridge shrapnel, poses significant risk to the patient as well as nearby staff and requires substantial caution. While many types of gunshot wounds to the urinary tract have been previously described, an injury of this nature would be unique and have no established treatment plan.13
4. Discussion
While the most common cause for sounding seems to simply be sexual gratification, there has been debate in the literature as to whether a patient presenting with a sounding injury should undergo a psychiatric evaluation.1,3 Breyer et al. found no difference in depression rates between MSM who sound and those who do not.2 However, a multitude of case reports suggest that patients requiring medical intervention for sounding-related injuries typically have an underlying psychiatric condition such as schizophrenia (most frequently), traumatic brain injury, bipolar disorder, or obsessive-compulsive disorder.4,8,14,15 A case series by Angulo-Lozano et al. examined patients presenting to the emergency department for sounding related encounters and evaluation by psychiatrists. In that series, 50 % of patients experienced psychiatric conditions.16 Furthermore, according to Gooren et al. patients performing urethral sounding often are driven by compulsion rather than sexual conduct.17 The relationship between psychiatric conditions and urethral sounding remains unclear. There is likely substantial heterogeneity among individuals who sound – with those requiring resultant medical attention potentially at higher risk of concomitant mental illness. While routine psychiatric follow up for sounding may be unnecessary it should be considered, particularly among individuals with repeat injury significant enough to necessitate medical treatment.
Some investigators have discouraged the practice of sounding, suggesting limiting patient access to insertable foreign objects.4,8 Breyer et al. takes a more realistic approach and provides suggestions for safe practice.2 These include promoting education on object characteristics that may facilitate easy expulsion or retrieval, such as using a smooth and flared, non-explosive device, and encouraging appropriate sterilization of the object.2 We agree with the interpretation that this approach is patient-centered, focuses on prevention, and is likely to contribute to physician-patient rapport and adherence.
5. Conclusion
Much remains to be learned regarding the epidemiology and practicing population of urethral sounding. Foreign body retention is an uncommon but difficult challenge resulting from the sexual practice. Understanding the components of ammunition and projectiles is an important consideration in the rare occasion that one must be manipulated/removed. In cases where these have been inserted, it is always safer to consider them live ammunition. Approach to removal depends on the object size shape and location and should be attempted with much care. Psychologic evaluation is not mandatory but should be considered.
CRediT authorship contribution statement
Paul C. Emerson: Writing – review & editing, Writing – original draft, Methodology, Investigation. Jeevan Nijhar: Writing – review & editing, Writing – original draft, Methodology, Investigation. Erin Hays: Writing – review & editing, Methodology, Investigation, Conceptualization. Nathan M. Shaw: Writing – review & editing, Investigation, Conceptualization. Krishnan Venkatesan: Writing – review & editing, Investigation, Conceptualization.
Declaration of competing interest
None.
References
- 1.van Ophoven A., deKernion J.B. Clinical management of foreign bodies of the genitourinary tract. J Urol. 2000;164(2):274–287. doi: 10.1097/00005392-200008000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Breyer B.N., Shindel A.W. Recreational urethral sounding is associated with high risk sexual behaviour and sexually transmitted infections. BJU Int. 2012;110(5):720–725. doi: 10.1111/j.1464-410X.2011.10810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rahman N.U., Elliott S.P., McAninch J.W. Self-inflicted male urethral foreign body insertion: endoscopic management and complications. BJU Int. 2004;94(7):1051–1053. doi: 10.1111/j.1464-410X.2004.05103.x. [DOI] [PubMed] [Google Scholar]
- 4.Crawford S.B., Lowry D., Watts S.H. Evaluation and management of urethral foreign bodies and description of a novel ultrasound-guided catheter-based extraction technique. J Am Coll Emerg Physicians Open. 2021;2(2) doi: 10.1002/emp2.12398. Published 2021 Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palmer C.J., Houlihan M., Psutka S.P., Ellis K.A., Vidal P., Hollowell C.M. Urethral foreign bodies: Clinical presentation and management. Urology. 2016;97:257–260. doi: 10.1016/j.urology.2016.05.045. [DOI] [PubMed] [Google Scholar]
- 6.Guerrero D.M., Sharma A. Chronic infectious complications of recreational urethral sounding with retained foreign body. Cureus. 2020;12(8) doi: 10.7759/cureus.9750. Published 2020 Aug 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shokoohi H., Kendrick Z., Sikka N., Boniface K.S. Sonographic localization of a retained urethral foreign body in an elderly patient. J Clin Ultrasound. 2018;46(4):296–298. doi: 10.1002/jcu.22515. [DOI] [PubMed] [Google Scholar]
- 8.Song J.B., Tanagho Y.S., Haseebuddin M., et al. Endoscopic management of genitourinary foreign bodies. Rev Urol. 2013;15(2):84–91. [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Department of the Interior. Glossary of Weapons Terminology. National Parks Service. Accessed 29 November. 2023. www.nps.gov/fosm/learn/historyculture/glossary-of-weapons-terminology.htm.
- 10.Powers D.B., Delo R.I. Characteristics of ballistic and blast injuries. Atlas Oral Maxillofac Surg Clin North Am. 2013;21(1):15–24. doi: 10.1016/j.cxom.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Jandial R., Reichwage B., Levy M., Duenas V., Sturdivan L. Ballistics for the neurosurgeon. Neurosurgery. 2008;62(2):472–480. doi: 10.1227/01.neu.0000316015.05550.7a. [DOI] [PubMed] [Google Scholar]
- 12.Heard B. second ed. Wiley-Blackwell; 2008. Handbook of Firearms and Ballistics: Examining and Interpreting Forensic Evidence. [Google Scholar]
- 13.Cinman N.M., McAninch J.W., Porten S.P., et al. Gunshot wounds to the lower urinary tract: a single-institution experience. J Trauma Acute Care Surg. 2013;74(3):725–731. doi: 10.1097/TA.0b013e31827e1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arai M., Takeshita H., Hirata W., et al. Female intravesical foreign body penetrating the bladder wall: a rare case of traditional Asian hair stick kanzashi. Clin Case Rep. 2023;11(10) doi: 10.1002/ccr3.8008. Published 2023 Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyle A., Martinez D.R., Mennie P.A., Rafiei A., Carrion R. The time-less urologic question, “Now why would you do that?” A case series and literature review of self-inserted urethral foreign bodies. J Clin Urol. 2014;7(3):165–169. doi: 10.1177/2051415813496562. [DOI] [Google Scholar]
- 16.Angulo-Lozano J.C., Gonzaga-Carlos N., Virgen-Rivera M.F., et al. Should psychiatry Be consulted when facing a self-inflicted foreign body in the urinary tract? Cureus. 2022 Mar 22;14(3) doi: 10.7759/cureus.23400. PMID: 35371889; PMCID: PMC8939880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gooren L.J. In: Jameson J.L., De Groot L.J., de Kretser D.M., et al., editors. Vol. 2. Elsevier; New York, NY: 2016. The endocrinology of sexual behavior and gender identity. (Endocrinology: Adult and Pediatric). 2163-76.e4. [DOI] [Google Scholar]