Figure 1.
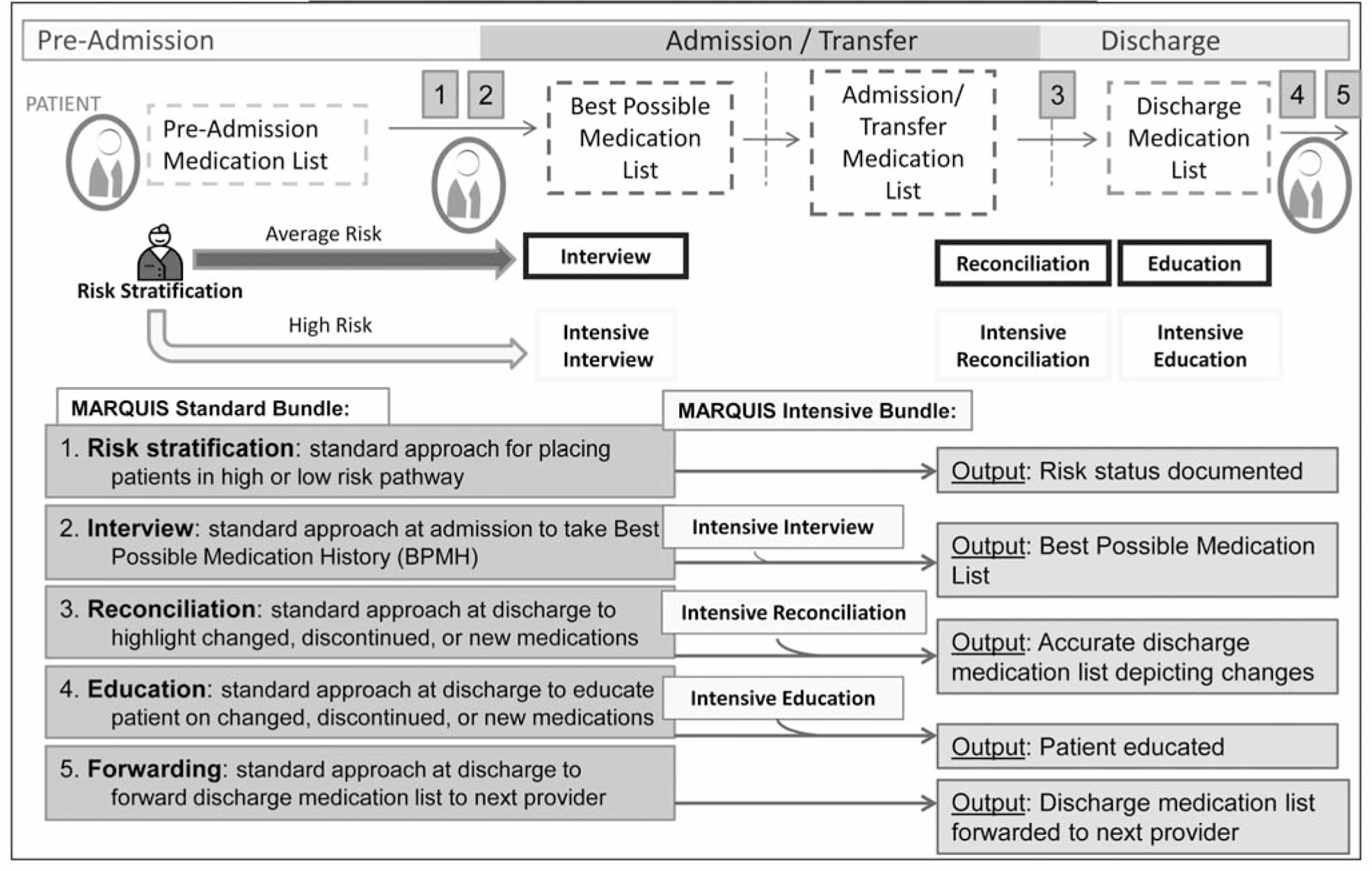
The ideal medication reconciliation process begins at time of patient admission, where patients are stratified into average- versus high-risk pathways, based on particular baseline patient characteristics. Both average- and high-risk patients then proceed through the same subsequent four steps in the medication reconciliation process that differ only in the additional dedicated time and expertise that is required for the intensive medication reconciliation bundle. These subsequent four steps are (2) Admission interview to obtain the best possible medication history (BPMH); (3) Standard approach toward discharge reconciliation of medications, where medication changes, discontinuations, and new medications are highlighted; (4) Standard approach to education of patient at time of discharge on any changed, discontinued, or new medications; and (5) Standard approach of forwarding discharge medication list to the follow-up provider(s). Notably, in the ideal medication reconciliation process, reconciliation occurs at time of admission, any transfer of service during patient hospitalization, and discharge. (Available in color in online article).
