Abstract
Inguinal hernia repair is performed more than 20 million times per annum, representing a significant health and economic burden. Over the last three decades, significant technical advances have started to reduce the invasiveness of these surgeries, which translated to better recovery and reduced costs. Here we bring forward an innovative surgical technique using a biodegradable cyanoacrylate glue instead of a traumatic suture to close the peritoneum, which is a highly innervated tissue layer, at the end of endoscopy hernia surgery. To test how this affects the invasiveness of hernia surgery, we conducted a cohort study. A total of 183 patients that underwent minimally invasive hernia repair, and the peritoneum was closed with either a conventional traumatic suture (n = 126, 68.9%) or our innovative approach using glue (n = 57, 31.1%). The proportion of patients experiencing acute pain after surgery was significantly reduced (36.8 vs. 54.0%, p = 0.032) by using glue instead of a suture. In accordance, the mean pain level was higher in the suture group (VAS = 1.5 vs. 1.3, p = 0.029) and more patients were still using painkillers (77.9 vs. 52.4%, p = 0.023). Furthermore, the rate of complications was not increased in the glue group. Using multivariate regressions, we identified that using a traumatic suture was an independent predictor of acute postoperative pain (OR 2.0, 95% CI 1.1–3.9, p = 0.042). In conclusion, suture-less glue closure of the peritoneum is innovative, safe, less painful, and possibly leads to enhanced recovery and decreased health costs.
Subject terms: Outcomes research, Pain
Introduction
Groin hernia is a prevalent disease with a life-time risk to require hernia surgery at least once of 3% for women and 27% for men. This results in over 20 million hernia surgeries performed annually. Over the last three decades1 the minimally-invasive approaches to hernia repair such as laparoscopic and robotic transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP) hernia repair, have gained in importance compared to open repair—such as the Lichtenstein technique—and become the gold standard2. In comparison to open surgery, the minimally invasive techniques reduce acute postoperative pain and thus allow a quicker return to work3,4. Since most hernia patients are of working age5, return to work is an important outcome measure after hernia surgery. The mean absence from work after minimally invasive inguinal hernia repair is of 6.4–7 days4,6. While this is better than in open repair (11 days4), it still cumulates in a significant socioeconomic burden given the high prevalence of the problem.
In addition, about 11% of patients suffer chronic pain after mesh-based inguinal hernia repair7. Non-penetrative mesh fixation had already been shown to be safe by Kukleta et al. in 20128, to decrease postoperative pain9 in randomized controlled trials10,11 and is now generally preferred over penetrative tacker fixation5. During TAPP procedure, in addition to the mesh implantation, the peritoneal flap needs to be closed which is routinely performed using a penetrative (resorbable) suture. Small case series brought forward that gluing may be a safe and fast alternative to suturing12–15. However, It remains unclear whether gluing instead of suturing brings a clinical benefit.
We hypothesize that using glue to close the peritoneal flap reduces the acute postoperative pain. To test this hypothesis, we performed a before-after cohort study after implementation of a glue applicator (Glutack) to close the peritoneal flap during TAPP. We find that atraumatic peritoneal flap closure with glue instead of a suture reduces acute postoperative pain. There was no effect on the safety and secondary outcomes such as complications, chronic postoperative pain or recurrence 1 year after laparoscopic inguinal hernia repair.
Materials and methods
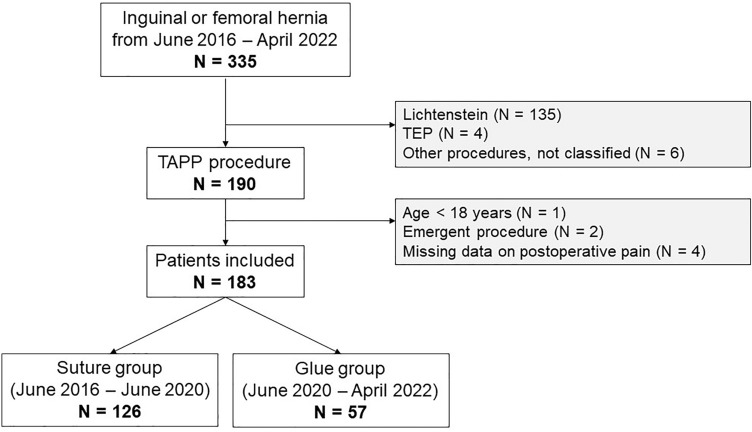
Study design and data collection
To investigate the impact of suture-less peritoneal flap closure on postoperative pain we conducted a retrospective before-after cohort study. The data of this study were prospectively collected using the Herniamed quality control study16. Herniamed is an international, internet-based quality assurance registry in which data on hernia surgery can be registered by hospitals and individual surgeons. All patients signed a consent form before enrollment. The, data collected on the Herniamed registry include patient demographics, health status, details on hernia and surgical procedure as well as follow-up data (up to ten years). From the Herniamed registry, all patients operated by one surgeon (CH) were selected. All adult patients that underwent elective inguinal or femoral hernia repair using the TAPP technique between June 2016 (registration to Herniamed) and April 2022 were included. Exclusion criteria were age under 18 years and if the repair was done as an emergency procedure (Fig. 1). All patients registered for this study gave their informed consent in writing (Fig. S1). The study was approved by the cantonal ethics committee (Ethikkommission Ostschweiz, Project ID 2016–00,123). All methods were performed in accordance with the relevant guidelines and regulations.
Figure 1.
Flowchart of patient selection.
The primary outcome of acute postoperative pain was systematically assessed with a simple yes/no question at 7–10 days post-surgery. The investigator (CH) was not blinded. In addition, pain was also quantified on a Visual Analogue Scale (VAS) (0 representing no pain and 10 corresponding to the worst possible pain) at the same time. Additional outcomes were collected in the study according the Herniamed protocol (Supplementary Table S1). Follow-up data (chronic pain and symptomatic recurrence) were collected after one year, using standardised questionnaire sent per Mail with a stamped reply envelope.
Operative technique
All study patients were operated by the same surgeon (CH). This surgeon had 19 years of experience in laparoscopic hernia surgery prior to begin of the study. This is more than necessary to reach a steady state in the learning curve for this procedure17. The surgical indication and procedure were carried out according to current standard of care recommendations5,18,19. In June 2020, the surgical routine of peritoneal flap closure was altered from using a suture to using glue without exception. Therefore, patients that received surgery before June 2020 were exposed to suturing and thus comprise the suture group, and the patients operated after June 2020 to April 2022 were exposed to gluing and therefore comprise the glue group. All patients were operated under general anaesthesia with intravenous disoprivan, remifentanil and fentanyl in supine position. No transversus abdominis plane block was performed.
A camera trocar was placed in midline 2–3 cm over the umbilicus (12 mm). After establishing a pneumoperitoneum of 12 mmHg two additional trocars (5 mm in the left, 12 mm in the right mid-abdomen) were inserted. Then, the peritoneum was incised about 6 cm cranial to the inner inguinal ring from lateral to medial. The preperitoneal space was dissected and the hernia sac reduced. Then, after a control of haemostasis, the mesh (Polypropelene Lightweight Monofilament Mesh of 10 × 15 cm, Parietene™ flat lightweight) was inserted and fixed with 8–10 single applications of Glubran®. In the Suture group, the peritoneal flap was then closed with a running suture using a resorbable barbed monofilament suture (V-Loc™). In the glue group, the peritoneum was closed using a cyanoacrylate glue [Glubran® 2 (N-butyl cyanoacrylate metacryloxysulfolane, NBCA-MS)] applied with 10–15 applications of Glutack® (Supplementary Video 1). Then, the trocars were removed under visual control and the fascia was sutured for the 12 mm trocar using resorbable back stitch. Postoperatively, all patients received Ibuprofen (400 mg p.o. qid) and Paracetamol (1 g p.o. qid). In patients with renal insufficiency, Ibuprofen was replaced by metamizole (1000 mg p.o. qid).
Statistical analysis
The baseline characteristics were described hernia-wise and patient-wise. For patient-wise comparison, the following criteria were applied for all patients with bilateral hernia: (i) hernia size was defined by the size of the larger hernia. (ii) If the patient had more than one hernia, it was considered as a combined hernia irrespective of location. (iii) Recurrent hernia was defined by having at least one recurring hernia.
Dichotomous data were reported as number and proportion, and continuous data as mean and standard deviation (SD). Categorical data were compared with Pearson's chi-squared or Fisher’s Exact Test. Continuous variables were compared by parametic tests (t-test) when normally distributed or by non-parametric tests (Wilcoxon) when non-normally distributed.
To adjust for potential confounding, a multivariate regression model was used. First univariate logistic regression was performed to explore the unadjusted association between each patient- and hernia-related variable and the primary outcome. Next, a multivariate regression model was fit with all variables statistically relevant in the unadjusted model. A two-sided level of significance of 0.05 was used for all analyses. All statistical analyses were performed using R statistical environment20. The underlying raw data and R scripts necessary to reproduce all figures and tables are available in the Supplementary Materials.
Results
Patient demographics and baseline characteristics
A total of 183 patients were enrolled with N = 126 in the suture and N = 57 in the glue group (Fig. 1). Demographic variables age (p = 0.9), BMI (p = 0.3), sex (p = 0.7) and ASA-score (p = 0.2) were not significantly different between groups (Table 1). However, the frequency of patients with preoperative pain was significantly higher in the suture group (56 vs 37%, p = 0.019) when compared with the glue group.
Table 1.
Patient demographics and preoperative pain.
| Variable | N | Suture, N = 1261 | Glue, N = 571 | p-value2 |
|---|---|---|---|---|
| Age | 183 | 55 (15) | 55 (14) | 0.9 |
| BMI | 183 | 24.99 (2.66) | 25.52 (3.10) | 0.3 |
| Sex | 183 | 0.7 | ||
| Female | 11/126 (9%) | 6/57 (11%) | ||
| Male | 115/126 (91%) | 51/57 (89%) | ||
| ASA Score | 183 | 0.2 | ||
| 1 | 99/126 (79%) | 40/57 (70%) | ||
| 2 | 27/126 (21%) | 16/57 (28%) | ||
| 3 | 0/126 (0%) | 1/57 (2%) | ||
| Presence of preoperative pain | 183 | 70/126 (56%) | 21/57 (37%) | 0.019 |
1Mean (SD); n/N (%).
2Wilcoxon rank sum test; Pearson's chi-squared test; Fisher's exact test.
Hernia characteristics
Next, we asked whether the hernia characteristics between the two groups were different (Table 2). In this study, a total of N = 258 hernias were operated (N = 175 in the suture, N = 83 in the glue group) in N = 183 patients (Fig. 1). There were more medial (31 vs. 18%) but less combined inguinal hernias (17 vs. 33%) in the suture group (p = 0.012) as defined by the Aachen classification (Table 2)21. Looking at size distribution, most hernias showed a maximal diameter between 1.5 and 3 cm in both groups, representing a Grade II inguinal hernia. There were slightly more Grade I hernias in the suture group (15 vs. 8.4%) and fewer Grade III (20 vs. 39%) (Table 2). The proportion of primary (vs. recurrent) hernias was the same in both groups. In terms of size, the suture group showed a significantly lower percentage of larger hernias (20 vs. 39% Hernia Grad III, p = 0.005). No significant difference in the primary hernia rate was found between two groups (93 vs. 95%) (Table 2).
Table 2.
Hernia characteristics (per hernia).
| Variable | N | Suture, N = 1751 | Glue, N = 831 | p-value2 |
|---|---|---|---|---|
| Aachen Classification | 258 | 0.012 | ||
| Combined | 29 / 175 (17%) | 27 / 83 (33%) | ||
| Femoral | 3 / 175 (2%) | 2 / 83 (2%) | ||
| Lateral | 88 / 175 (50%) | 39 / 83 (47%) | ||
| Medial | 55 / 175 (31%) | 15 / 83 (18%) | ||
| Size | 258 | 0.005 | ||
| I (< 1.5 cm) | 26 / 175 (15%) | 7 / 83 (8%) | ||
| II (1.5-3 cm) | 114 / 175 (65%) | 44 / 83 (53%) | ||
| III (> 3 cm) | 35 / 175 (20%) | 32 / 83 (39%) | ||
| Primary Hernia | 258 | 162 / 175 (93%) | 79 / 83 (95%) | 0.43 |
1n / N (%); Mean (SD).
2Fisher's exact test; Pearson's Chi-squared test; Wilcoxon rank sum test.
To compare the hernia characteristics per patient, the data of patients with bilateral hernia repair was processed as described in the methods section. Overall, the two treatment groups are comparable (Table 3). Notably, there was a significant difference in hernia size between the groups with a higher rate of size I (9 vs. 2%) and size II (65 vs. 56%) but less size III hernias (26 vs. 42%) in the suture group (p = 0.043) (Table 3).
Table 3.
Hernia characteristics (per patient).
| Variable | N | Suture, N = 1261 | Glue, N = 571 | p-value2 |
|---|---|---|---|---|
| Aachen Classification | 183 | 0.6 | ||
| Combined | 62 / 126 (48%) | 33 / 57 (58%) | ||
| Femoral | 3 / 126 (2%) | 0 / 57 (0%) | ||
| Lateral | 48 / 126 (38%) | 18 / 57 (32%) | ||
| Medial | 13 / 126 (10%) | 6 / 57 (10%) | ||
| Side | 183 | 0.4 | ||
| Bilateral | 49 / 126 (39%) | 26 / 57 (46%) | ||
| Unilateral | 77 / 126 (61%) | 31 / 57 (54%) | ||
| Size | 183 | 0.043 | ||
| I (< 1.5 cm) | 11 / 126 (9%) | 1 / 57 (2%) | ||
| II (1.5-3 cm) | 82 / 126 (65%) | 32 / 57 (56%) | ||
| III (> 3 cm) | 33 / 126 (26%) | 24 / 57 (42%) | ||
| Primary Hernia | 183 | 117 / 126 (93%) | 54 / 57 (95%) | 0.8 |
1Mean (SD); n / N (%).
2Wilcoxon rank sum test; Pearson's chi-squared test; Fisher's exact test.
Postoperative pain
The rate of patients feeling pain 7–10 days after operation is significantly higher in the suture group when compared with the glue group (respectively 54 vs 37%, p = 0.032) (Table 4, Fig. 2). Congruently, the pain score (VAS = 1.50 vs. 1.31, p = 0.029) and the rate of patients still depending on painkillers (78 vs. 52%, p = 0.023) were significantly increased in the suture group (Table 4).
Table 4.
Postoperative follow-up data.
| Variable | N | Suture, N = 1261 | Glue, N = 571 | p-value2 |
|---|---|---|---|---|
| Pain after 7–10 days | 183 | 68 / 126 (54%) | 21 / 57 (37%) | 0.032 |
| Degree of pain after 7–10 days | 183 | 1.34 (1.50) | 0.88 (1.31) | 0.029 |
| Need for Analgesia after 7–10 days | 89 | 53 / 68 (78%) | 11 / 21 (52%) | 0.023 |
| Unknown | 58 | 36 | ||
| Duration of surgery [minutes] | 183 | 67 (24) | 71 (27) | 0.4 |
| Complications (without pain) | 183 | 8 / 126 (6.3%) | 0 / 57 (0%) | 0.059 |
| Intraoperative Complications | 3 / 126 (2.4%) | 0 / 57 (0%) | 0.6 | |
| Postoperative Complications | 4 / 126 (3.2%) | 0 / 57 (0%) | 0.3 | |
| Postoperative Hematoma | 3 / 126 (2.4%) | 0 / 57 (0%) | 0.6 | |
| Postoperative Seroma | 1 / 126 (0.8%) | 0 / 57 (0%) | > 0.9 |
| Follow-up 1 year postoperative | ||||
|---|---|---|---|---|
| Pain | 132 | 11 / 101 (11%) | 4 / 31 (13%) | 0.8 |
| Unknown | 25 | 26 | ||
| Pain at rest | 132 | 3 / 101 (3.0%) | 1 / 31 (3.2%) | > 0.9 |
| Unknown | 25 | 26 | ||
| Pain by physical Stress | 132 | 10 / 101 (9.9%) | 4 / 31 (13%) | 0.7 |
| Unknown | 25 | 26 | ||
| Dysesthesia | 132 | 2 / 101 (2.0%) | 0 / 31 (0%) | > 0.9 |
| Unknown | 25 | 26 | ||
| Recurrence of Hernia | 92 | 1 / 71 (1.4%) | 0 / 21 (0%) | > 0.9 |
| Unknown | 55 | 36 | ||
| Reason for Break Off of Follow-up | 163 | 0.4 | ||
| No break off | 101 / 126 (80%) | 31 / 37 (84%) | ||
| Patient moved | 1 / 126 (0.8%) | 1 / 37 (2.7%) | ||
| Other reasons for break off | 24 / 126 (19%) | 5 / 37 (14%) | ||
| Unknown | 0 | 20 | ||
1Mean (SD); n / N (%).
2Wilcoxon rank sum test; Pearson's Chi-squared test; Fisher's exact test.
Statistically significant values are in bold.
Figure 2.
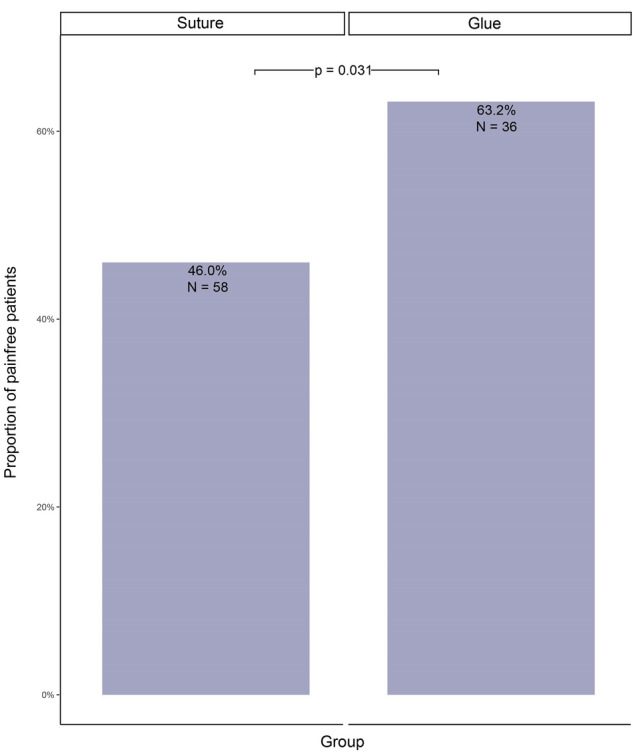
Painfree patients within 10 days of operation.
In our univariate analysis, we identified 5 predictors for acute postoperative pain (7–10 days post-surgery): peritoneal flap suturing (OR 2.01, p = 0.031), younger age (OR 1.03, p = 0.002), presence of preoperative pain (OR 1.81, p = 0.046), female sex (OR 3.85, p = 0.014) and small hernia size (size II OR 2.9, size III OR 4.77, p = 0.049) (Table 5).
Table 5.
Painfree 7–10 days after operation (univariate regression model).
| Variable | N | Event N | OR1 | 95% CI1 | p-value |
|---|---|---|---|---|---|
| Group | 183 | 94 | 0.031 | ||
| Suture | – | – | |||
| Glue | 2.01 | 1.07, 3.86 | |||
| Age | 183 | 94 | 1.03 | 1.01, 1.06 | 0.002 |
| BMI | 183 | 94 | 1.05 | 0.95, 1.17 | 0.34 |
| Sex | 183 | 94 | 0.014 | ||
| Female | – | – | |||
| Male | 3.85 | 1.30, 14.1 | |||
| ASA score | 183 | 94 | 1.38 | 0.72, 2.71 | 0.33 |
| Previous operation | 183 | 94 | 0.52 | ||
| No | – | – | |||
| Yes | 1.29 | 0.59, 2.89 | |||
| Preoperative pain | 183 | 94 | 0.046 | ||
| Yes | – | – | |||
| No | 1.81 | 1.01, 3.27 | |||
| Aachen classification | 183 | 94 | 0.20 | ||
| Combined | – | – | |||
| Femoral | 0.00 | ||||
| Lateral | 1.00 | 0.53, 1.87 | |||
| Medial | 1.29 | 0.48, 3.60 | |||
| Side | 183 | 94 | 0.89 | ||
| Bilateral | – | – | |||
| Unilateral | 0.96 | 0.53, 1.73 | |||
| Size | 183 | 94 | 0.049 | ||
| I (< 1.5 cm) | – | – | |||
| II (1.5-3 cm) | 2.90 | 0.82, 13.6 | |||
| III (> 3 cm) | 4.77 | 1.27, 23.3 | |||
| Primary hernia | 183 | 94 | 0.92 | ||
| No | – | – | |||
| Yes | 1.06 | 0.32, 3.51 | |||
| Duration of surgery [minutes] | 183 | 94 | 0.99 | 0.98, 1.00 | 0.21 |
1OR = Odds Ratio, CI = Confidence Interval.
Statistically significant values are in bold.
When adjusted in a multivariate regression model, the three independent predictors of acute postoperative pain (7–10 days post-surgery) were as follows. Peritoneal flap suturing (OR 2.07, p = 0.042), younger age (OR 1.03, p = 0.004) and female sex (OR 4.57, p = 0.015) (Table 6).
Table 6.
Painfree 7–10 days after operation (multivariate regression model).
| Variable | OR1 | 95% CI1 | p-value |
|---|---|---|---|
| Group | 0.042 | ||
| Suture | – | – | |
| Glue | 2.07 | 1.03, 4.26 | |
| Age | 1.03 | 1.01, 1.06 | 0.004 |
| Sex | 0.015 | ||
| Female | – | – | |
| Male | 4.57 | 1.33, 19.0 | |
| Preoperative Pain | 0.66 | ||
| Yes | – | – | |
| No | 1.16 | 0.60, 2.22 | |
| Size | 0.79 | ||
| I (< 1.5 cm) | – | – | |
| II (1.5-3 cm) | 1.45 | 0.37, 7.20 | |
| III (> 3 cm) | 1.67 | 0.38, 8.89 |
1OR = Odds Ratio, CI = Confidence Interval.
Statistically significant values are in bold.
Unlike previous reports, we did not observe a significant decrease in operation time in the suture group (67 min) when compared with the glue group (71 min, p > 0.05), and the intra- and early postoperative complication rate were comparable in both groups (respectively 6.3 vs 0%, p = 0.059).
Furthermore, the two approaches resulted in comparable outcomes after 1 year follow-up. The rate of patients experiencing chronic pain was comparable found between the suture and glue groups (respectively 11 vs 13%, p > 0.05) whether for pain at rest (3 vs 3.2%, p > 0.05) or pain during physical stress (9.9 vs 13%, p > 0.05). As for the dysesthesias experienced one year postoperatively, no significant difference were found for hernia recurrence rate after 1 year (Table 4).
Discussion
Here we present a comparative cohort study, supporting the introduction of an innovative concept: utilizing a glue applicator instead of a suture to close the peritoneal flap after TAPP. Our findings demonstrate that this less invasive approach significantly reduces acute pain levels experienced 7–10 days post-surgery. Because inguinal hernia repair is so frequently performed22,23 and often in patients of working age24, this small improvement in care amounts to a huge beneficial effect for health care systems.
Laparoscopic suturing has a relatively long learning curve, which ideally should first be practiced outside the operating theatre in a specific box-training before it can be performed on patients25–27. Incremental technological support (e.g. 3D screens, virtual reality training) attempts to make the surgeon's job easier28–30. Here we bring forward yet another approach: the use of a glue applicator, which is fast, intuitive, and safe for the patient31.
The use of glue in the abdominal cavity is still subject to intense debate. The acrylic adhesive utilized in this study (Glubran2®) deviates from the N-butyl-2-cyanoacrylate (NBCA) monomer present in Histoacryl® due to the inclusion of metacryloxysulfolane (MS). This addition, acting as a comonomer, modifies its chemical composition and confers anti-inflammatory properties, along with changing its viscosity among other characteristics32. Glue mesh-fixation has been evaluated in a prospective manner and gluing the mesh in place, results in a significant reduction of chronic pain and haematoma rate, when compared to mechanical fixation (high level of evidence)33,34. Its use has also been described in the context of incisional hernia repair by Laparoscopic intraperitoneal onlay mesh (IPOM)31. However, these studies investigate the effect on mesh fixation. Only small retrospective, non-comparative studies reported its implementation in the context of peritoneal closure12,35. In their 2016 publication, Köckerling et al. report a postoperative bleeding occurrence of about 1.5% after endoscopic hernia repair36. While the current cohort is clearly underpowered to detect a significant difference of such a rare event, we argue on a conceptual level that using glue instead of a suture might reduce the bleeding risk.
Furthermore, glue fixation of the peritoneal flap did not increase hernia recurrence rate. This statement is limited, because the current cohort is neither sufficiently powered nor followed up long enough for this specific question. However, recent experimental studies conducted by Lesch et al. on biomechanical constraints in abdominal reconstruction suggest that stability primarily emerges during the period of plastic deformation. This process appears to occur mainly during the initial mechanical stresses37.
While not insignificant, the closure of the peritoneum appears to have a secondary impact on biomechanical stability following mesh hernia repair38. Overall, we conclude that glue closure of the peritoneal flap after TAPP is safe. The research conducted by Kallinowski et al. assigns it a value as a term rather than a factor within the equation used to calculate the GRIP39 value, assessing resistance of the Mesh-reconstruction (Gained/Critical Resistance to Impacts related to Pressure). Undoubtedly, this is a hot topic, and the principles of biomechanically calculated repair (BCR), which have shown promising outcomes for incisional hernias40 should be carefully considered in patient-tailored inguinal hernia surgery.
Our data do not allow us to infer on the exact pathophysiological reasons why post-surgical pain is decreased after gluing. However, some studies seem to suggest that sutures in the abdominal wall may create ischemic areas in the muscle, triggering inflammation and therefore pain41. Importantly, the beneficial effect of gluing was lost after one year. The overall percentage of patients with chronic pain (defined as lasting more than 3 months after the operation) in this study was 11% und therefore well comparable with the numbers reported in the literature5. As the suture used is absorbable and has been resorbed after this time (V-Loc™ resorption after 180 days42), we assume that it contributes to the difference of initial acute postoperative pain but not the chronic pain. Interestingly, the beneficial effect of gluing might be lost in the elderly as we observed that older ager is an independent protective factor against acute postoperative pain. This difference is in line with the current literature, in the context of decreased function of the nociceptive sensation and an increased pain perception threshold in the elderly43,44 and possibly also generational differences in pain experience41. Conversely—although the study is clearly underpowered to back this up—the positive effect of peritoneal gluing may be even more pronounced in women because women have an independent propensity to experience more pain after inguinal hernia surgery. This effect, of unknown pathophysiology and probably multivariate etiology has already been observed and discussed in several studies whose results tended to demonstrate the same effect45–47. Taken together, we bring forward that gluing is less painful than suturing most likely because it is less traumatic, an effect that may be particularly desirable in young and female patients with pre-operative pain.
The novelty of our study is that we use glue for the closure of the peritoneum, and not only to fixate the mesh and that we compare this technique with an established approach. This shows a remarkable beneficial effect of gluing over suturing. But because this study is limited by the cohort size and its retrospective non-blinded nature, the current data alone may not warrant a recommendation of gluing over suturing just yet. In addition, the study suffers from missing data regarding the analgesic use and follow-up data and some, presumably asymptomatic, patients were lost to follow-up after one year. A further limitation of this study is that the change in surgical technique (suture vs glue) coincides in time with a change of the policy makers in Switzerland that decreed that outpatient surgery should be prioritized over inpatient surgery for unilateral inguinal hernia repair48. This may be a systematic bias in this study that cannot be addressed by study design, and it was also the reason why neither the length of hospital stay, nor the treatment costs were compared in this cohort. Despite these limitations, the current study is the first to systematically compare suturing versus gluing the peritoneal flap after TAPP procedure and clearly provides evidence that the technique is safe and might be superior in terms of acute pain. Clearly, further register based studies or even a randomized controlled trial is necessary to infer on the true potential of this surgical technique.
Conclusion
This study provides solid evidence that the closure of the peritoneal flap after TAPP with cyanoacrylate glue instead of a suture is less painful and at least equally safe. This innovative surgical technique, which has not yet been comparatively studied in the current literature, may be preferable over suturing, especially in women, in the young, and in patients with pre-operative pain.
Supplementary Information
Acknowledgements
We would like to thank Dr. med. Tobias Gehrig, senior physician at the Linth Hospital in Uznach, for the excellent collaboration during this work between the two establishments.
Author contributions
M.H. J.Z and C.H. designed the study. C.H. collected the data and performed all surgeries. M.H. and J.Z. wrote the main manuscript. S. P. did the statistical analysis. G.B. and D.C. supervised the writing and the statistical analysis. E.G. contributed to data collection and to edit the supplemental video. All authors critically reviewed the manuscript and gave their consent.
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files). Further inquiries can be directed to the corresponding author/s.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Christian Helbling and Joel Zindel.
Contributor Information
Michaël Huguenin-Dezot, Email: michael.huguenin-dezot@insel.ch.
Joel Zindel, Email: joel.zindel@unibe.ch.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-62364-w.
References
- 1.Ger R. Laparoscopic hernia operation. Chirurg. 1991;62:266–270. [PubMed] [Google Scholar]
- 2.Aiolfi A, et al. Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia. 2019;23:473–484. doi: 10.1007/s10029-019-01964-2. [DOI] [PubMed] [Google Scholar]
- 3.Wellwood J, et al. Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ. 1998;317:103–110. doi: 10.1136/bmj.317.7151.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savarise MT, Simpson JP, Moore JM, Leis VM. Improved functional outcome and more rapid return to normal activity following laparoscopic hernia repair. Surgical Endoscopy. 2001;15:574–578. doi: 10.1007/s004640080039. [DOI] [PubMed] [Google Scholar]
- 5.HerniaSurge G. International guidelines for groin hernia management. Hernia. 2018;22:1–165. doi: 10.1007/s10029-017-1668-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jenkins JT, O'Dwyer PJ. Inguinal hernias. BMJ. 2008;336:269–272. doi: 10.1136/bmj.39450.428275.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nienhuijs S, et al. Chronic pain after mesh repair of inguinal hernia: a systematic review. Am. J. Surg. 2007;194:394–400. doi: 10.1016/j.amjsurg.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Kukleta JF, Freytag C, Weber M. Efficiency and safety of mesh fixation in laparoscopic inguinal hernia repair using n-butyl cyanoacrylate: long-term biocompatibility in over 1300 mesh fixations. Hernia. 2012;16:153–162. doi: 10.1007/s10029-011-0887-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bittner R, et al. Lightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP) Surgical Endoscopy. 2010;24:2958–2964. doi: 10.1007/s00464-010-1140-9. [DOI] [PubMed] [Google Scholar]
- 10.Brugger L, et al. Objective hypoesthesia and pain after transabdominal preperitoneal hernioplasty: a prospective, randomized study comparing tissue adhesive versus spiral tacks. Surgical Endoscopy. 2012;26:1079–1085. doi: 10.1007/s00464-011-2003-8. [DOI] [PubMed] [Google Scholar]
- 11.Subwongcharoen S, Ruksakul K. A randomized controlled trial of staple fixation versus N-butyl-2-cyanoacrylate fixation in laparoscopic inguinal hernia repair. J. Med. Assoc. Thai. 2013;96(Suppl 3):S8–13. [PubMed] [Google Scholar]
- 12.Phillips AW, Viswanath YK, Burns JK, Hall CE, Horgan AF. Use of fibrin glue for fixation of mesh and approximation of Peritoneum in Transabdominal Preperitoneal (TAPP) inguinal hernia repair: technical feasibility and early surgical outcomes. Surg. Laparosc. Endosc. Percutan. Tech. 2014;24:e43–45. doi: 10.1097/SLE.0b013e31828f85d5. [DOI] [PubMed] [Google Scholar]
- 13.Ielpo B, et al. Laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair using fibrin glue for fixation of the mesh and peritoneum closure. Surg. Laparosc. Endosc. Percutan. Tech. 2020;30:e24–e27. doi: 10.1097/SLE.0000000000000797. [DOI] [PubMed] [Google Scholar]
- 14.Raab S, Huber L, Fortelny R, Shamiyeh A. Laparoscopic transabdominal preperitoneal (TAPP) groin hernia repair using n-butyl-2-cyanoacrylate (LiquiBandFIX8) for mesh fixation and peritoneal closure: case report about extraperitoneal hematoma. Ann. Med. Surg. (Lond) 2024;86:481–484. doi: 10.1097/ms9.0000000000001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson P, Hickey L. Laparoscopic transabdominal preperitoneal (TAPP) groin hernia repair using n-butyl-2-cyanoacrylate (Liquiband®Fix8™) for mesh fixation and peritoneal closure: learning experience during introduction into clinical practice. Hernia. 2019;23:601–613. doi: 10.1007/s10029-018-1861-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stechemesser B, Jacob DA, Schug-Pass C, Kockerling F. Herniamed: an internet-based registry for outcome research in hernia surgery. Hernia. 2012;16:269–276. doi: 10.1007/s10029-012-0908-3. [DOI] [PubMed] [Google Scholar]
- 17.Sivakumar J, et al. Learning curve of laparoscopic inguinal hernia repair: systematic review, meta-analysis, and meta-regression. Surgical Endoscopy. 2022 doi: 10.1007/s00464-022-09760-3. [DOI] [PubMed] [Google Scholar]
- 18.Simons MP, et al. European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miserez M, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014;18:151–163. doi: 10.1007/s10029-014-1236-6. [DOI] [PubMed] [Google Scholar]
- 20.R Core Team. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (2019). URL https://www.R-project.org/.
- 21.Schumpelick V, Treutner KH, Arlt G. Classification of inguinal hernias. Chirurg. 1994;65:877–879. [PubMed] [Google Scholar]
- 22.Bansal VK, et al. A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surgical endoscopy. 2013;27:2373–2382. doi: 10.1007/s00464-013-2797-7. [DOI] [PubMed] [Google Scholar]
- 23.Fitzgibbons RJ, Jr, et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA. 2006;295:285–292. doi: 10.1001/jama.295.3.285. [DOI] [PubMed] [Google Scholar]
- 24.Savarise MT, Simpson JP, Moore JM, Leis VM. Improved functional outcome and more rapid return to normal activity following laparoscopic hernia repair. Surgical Endoscopy. 2001;15:574–578. doi: 10.1007/s004640080039. [DOI] [PubMed] [Google Scholar]
- 25.Rodrigues SP, et al. Laparoscopic suturing learning curve in an open versus closed box trainer. Surgical Endoscopy. 2016;30:315–322. doi: 10.1007/s00464-015-4211-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aggarwal R, Moorthy K, Darzi A. Laparoscopic skills training and assessment. Br. J. Surg. 2004;91:1549–1558. doi: 10.1002/bjs.4816. [DOI] [PubMed] [Google Scholar]
- 27.Scott DJ, et al. Laparoscopic training on bench models: better and more cost effective than operating room experience? J. Am. Coll. Surg. 2000;191:272–283. doi: 10.1016/s1072-7515(00)00339-2. [DOI] [PubMed] [Google Scholar]
- 28.Hanani M, et al. Comparison of a 3D head-mounted display (HMS-3000MT) and 3D passive polarizing display with 2D technique for first laparoscopic inguinal hernia repair by novice surgeons. Hernia. 2020;24:661–668. doi: 10.1007/s10029-019-02065-w. [DOI] [PubMed] [Google Scholar]
- 29.Seymour NE, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann. Surg. 2002;236:458–463. doi: 10.1097/00000658-200210000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grantcharov TP, et al. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br. J. Surg. 2004;91:146–150. doi: 10.1002/bjs.4407. [DOI] [PubMed] [Google Scholar]
- 31.Wilson P. Laparoscopic intraperitoneal onlay mesh (IPOM) repair using n-butyl-2-cyanoacrylate (Liquiband Fix8) for mesh fixation: learning experience and short-medium term results. Hernia. 2020;24:1387–1396. doi: 10.1007/s10029-020-02144-3. [DOI] [PubMed] [Google Scholar]
- 32.Leonardi M, et al. Glubran 2: a new acrylic glue for neuroradiological endovascular use Experimental study on animals. Interv. Neuroradiol. 2002;8:245–250. doi: 10.1177/159101990200800304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Habib Bedwani NAR, et al. Glue versus mechanical mesh fixation in laparoscopic inguinal hernia repair: meta-analysis and trial sequential analysis of randomized clinical trials. Br. J. Surg. 2021;108:14–23. doi: 10.1093/bjs/znaa002. [DOI] [PubMed] [Google Scholar]
- 34.Hu N, et al. Efficacy and safety of glue mesh fixation for laparoscopic inguinal hernia: A meta-analysis of randomized controlled trials. Asian J. Surg. 2023 doi: 10.1016/j.asjsur.2023.03.146. [DOI] [PubMed] [Google Scholar]
- 35.Wilson P, Hickey L. Laparoscopic transabdominal preperitoneal (TAPP) groin hernia repair using n-butyl-2-cyanoacrylate (Liquiband(R)Fix8) for mesh fixation and peritoneal closure: learning experience during introduction into clinical practice. Hernia. 2019;23:601–613. doi: 10.1007/s10029-018-1861-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kockerling F, Roessing C, Adolf D, Schug-Pass C, Jacob D. Has endoscopic (TEP, TAPP) or open inguinal hernia repair a higher risk of bleeding in patients with coagulopathy or antithrombotic therapy? Data from the Herniamed Registry. Surgical endoscopy. 2016;30:2073–2081. doi: 10.1007/s00464-015-4456-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carolin L, et al. Cyclic pulse loads pave the road to the GRIP concept in abdominal wall reconstruction. Mini-Invasive Surg. 2023;7:25. [Google Scholar]
- 38.Ross SW, et al. Does peritoneal flap closure technique following transabdominal preperitoneal (TAPP) inguinal hernia repair make a difference in postoperative pain? A long-term quality of life comparison. Surg. Endosc. 2017;31:2548–2559. doi: 10.1007/s00464-016-5258-2. [DOI] [PubMed] [Google Scholar]
- 39.Kallinowski F, et al. Assessing the GRIP of ventral hernia repair: How to securely fasten DIS classified meshes. Front. Surg. 2017;4:78. doi: 10.3389/fsurg.2017.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lesch C, et al. STRONGHOLD first-year results of biomechanically calculated abdominal wall repair: A propensity score matching. Hernia. 2023 doi: 10.1007/s10029-023-02897-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nienhuijs SW, Rosman C, Strobbe LJ, Wolff A, Bleichrodt RP. An overview of the features influencing pain after inguinal hernia repair. Int. J. Surg. 2008;6:351–356. doi: 10.1016/j.ijsu.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 42.https://www.medtronic.com/content/dam/covidien/library/emea/de/product/wound-closure/weu-v-loc-180-tech-sheet-de.pdf
- 43.Chakour MC, Gibson SJ, Bradbeer M, Helme RD. The effect of age on A delta- and C-fibre thermal pain perception. Pain. 1996;64:143–152. doi: 10.1016/0304-3959(95)00102-6. [DOI] [PubMed] [Google Scholar]
- 44.Gibson SJ, Farrell M. A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. Clin. J. Pain. 2004;20:227–239. doi: 10.1097/00002508-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Tolver MA, Strandfelt P, Rosenberg J, Bisgaard T. Female gender is a risk factor for pain, discomfort, and fatigue after laparoscopic groin hernia repair. Hernia. 2013;17:321–327. doi: 10.1007/s10029-012-0956-8. [DOI] [PubMed] [Google Scholar]
- 46.Lau H, Patil NG. Acute pain after endoscopic totally extraperitoneal (TEP) inguinal hernioplasty: multivariate analysis of predictive factors. Surg. Endosc. 2004;18:92–96. doi: 10.1007/s00464-003-9068-y. [DOI] [PubMed] [Google Scholar]
- 47.Reinpold W. Risk factors of chronic pain after inguinal hernia repair: a systematic review. Innov. Surg. Sci. 2017;2:61–68. doi: 10.1515/iss-2017-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Krankenpflege-Leistungsverordnung (KLV). Verordnung des Eidgenössischen Departements des Innern über Leistungen in der obligatorischen Krankenpflegeversicherung, Änderung vom 7. Juni 2018. (SR 832.112.31). Retrieved from https://www.admin.ch/opc/de/classified-compilation/19950069/index.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its Supplementary Information files). Further inquiries can be directed to the corresponding author/s.