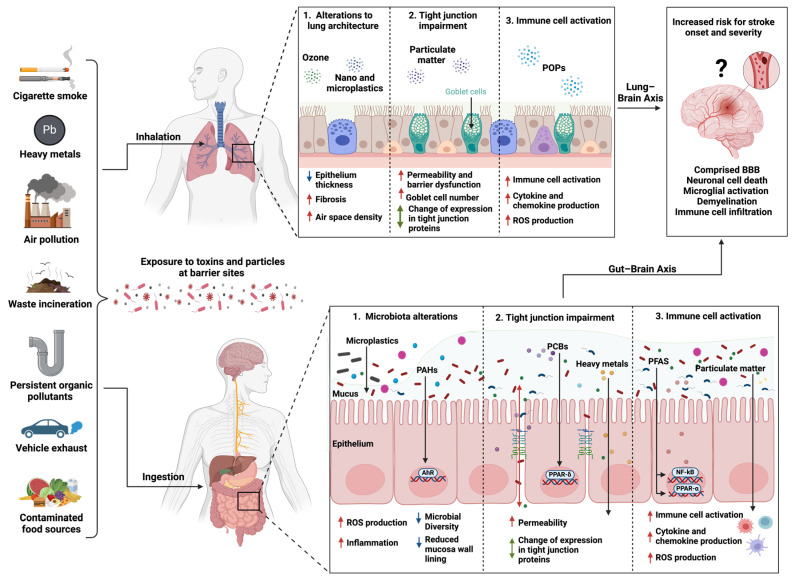
Figure 1.
Mechanisms of environmental toxins inhaled or ingested potentially leading to increased susceptibility to stroke and severity. Environmental toxins originate from several sources, including industrial processes and as byproducts from incomplete combustion. These toxins can enter the environment and contaminate sources such as food, water, and soil and can also be abundant in the air, increasing human exposure via inhalation and ingestion as two primary routes. Once exposed, these toxins can target the primary organs, gut and lungs, and induce perturbation of the microbiota composition (dysbiosis), a pro-inflammatory response leading to disruption of tissue architecture, immune cell activation, and increased permeability at epithelial barrier sites, which may increase the exposure risk to harmful bacteria and pathogens. Inhaled or ingested xenobiotics are metabolized and bind to their respective receptors, upregulating ligand-activated transcription factors and inflammatory signaling pathways (AhR, PPAR, and NF-κB). Alterations at the gut and lung barriers can indirectly affect brain function. Metabolites generated from the metabolism of xenobiotics can traffic to the brain and may directly increase the risk for stroke by compromising the blood–brain barrier, activating brain resident immune cells and immune cells trafficking from the periphery, and causing cell death. AhR, aryl hydrocarbon receptor; BBB, blood–brain barrier; NF-κB, nuclear factor-κB; PAHs, polycyclic aromatic hydrocarbons; PCBs, polychlorinated biphenyls; PET, polyethylene terephthalate; PFASs, per- and polyfluoroalkyl substances; POPs, persistent organic pollutants; PPAR-α and -δ, peroxisome proliferator-activated receptor-alpha and -delta; ROS, reactive oxygen species; TNF-α, tumor necrosis factor-alpha; Tregs, regulatory T cells, created with Biorender.com.