Perennial rhinitis may be defined clinically as an inflammatory condition of the nose characterised by nasal obstruction, sneezing, itching, or rhinorrhoea, occurring for an hour or more on most days throughout the year. In one study in London of adults between the ages of 16 and 65 years, the prevalence of rhinitis was 16%; of these, 8% had perennial symptoms, 6% perennial and seasonal symptoms, and 2% seasonal symptoms alone. As with asthma, both seasonal and perennial rhinitis seem to be increasing.
Non-allergic, non-infective rhinitis*
Idiopathic rhinitis refers to a heterogeneous group of patients with nasal hyperresponsiveness to non-specific triggers such as strong smells (eg, perfumes, bleach, and solvents), tobacco smoke, vehicle exhaust fumes, and changes in environmental temperature and humidity in the absence of an identifiable underlying cause
Non-allergic rhinitis with eosinophilia syndrome (NARES) is characterised by nasal eosinophilia (usually in young women) with perennial nasal symptoms with negative results on skin prick testing and normal IgE concentrations. Patients usually respond well to topical corticosteroids
Hormonal rhinitis can occur during pregnancy, puberty, hypothyroidism, and acromegaly. Postmenopausal women may develop atrophic changes, elderly men sometimes watery rhinorrhoea (“old man’s drip”)
Drug induced rhinitis is associated with several drugs. β sympathomimetic receptor antagonists (β blockers) and angiotensin converting enzyme inhibitors have been associated with nasal symptoms, as have topical ophthalmic β blockers, chlorpromazine, oral contraceptives, aspirin, and other non-steroidal anti-inflammatory agents
Food induced rhinitis Gustatory rhinorrhoea may occur during consumption of hot and spicy foods. Non-IgE mediated hypersensitivity may result from food colourings and preservatives. Alcohol, in addition to the mechanisms above, also acts as a vasodilator, which may result in nasal obstruction
Emotional factors including stress and sexual arousal can affect the nose, probably due to autonomic stimulation
*Poorly understood and more difficult to identify specific causes
Classification
Allergic rhinitis—Perennial allergic rhinitis can be more difficult to diagnose than seasonal allergy, particularly if the patient presents with secondary symptoms of sinusitis and a “permanent cold.” The most common allergen to account for perennial allergic symptoms is the house dust mite (Dermatophagoides pteronyssinus). Other frequent causes are animals: particularly cats, dogs, and horses.
Occupational rhinitis may result from allergy to airborne agents in the workplace—for example, laboratory animals and latex.
Infective rhinitis—Infective rhinitis may be acute or chronic. Chronic symptoms may be due to specific infections, such as fungi or tuberculosis. Chronic infection may also be the result of a host defence deficiency; this may be systemic (for example, panhypogammaglobulinaemia, IgA deficiency, or AIDS) or a local problem (for example, primary ciliary dyskinesia).
Other factors—Other non-allergic, non-infective factors may be involved (see box).
Differential diagnosis
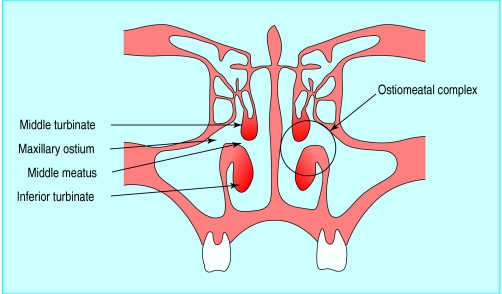
Structural abnormalities of the nose include deviation of the nose or septum, enlarged middle and inferior turbinates, adenoidal hypertrophy (particularly in children; rare in adults), and choanal atresia. The ostiomeatal complex is the area lying between the middle and inferior turbinates and the natural ostium of the maxillary sinus. It is this area which drains and aerates the maxillary sinus, the anterior ethmoidal sinuses, and the frontal sinus. Obstruction in this area, whether structural or secondary to an inflammatory condition, will predispose to sinusitis.
Nasal polyps result from inflammation of the mucosal lining of the sinuses; the lining prolapses down, particularly from the anterior ethmoidal sinuses through the middle meatus to obstruct the nasal airway. Allergy does not seem to be an important factor. Nasal polyps in children are rare and are almost invariably associated with cystic fibrosis. A strong association exists between nasal polyps, asthma, and sensitivity to aspirin (Samter’s triad).
Granulomatous rhinitis may be associated with Wegener’s granulomatosis and sarcoidosis.
Primary atopic rhinitis is characterised by nasal congestion, hyposmia, and an unpleasant smell (ozoena), resulting from a progressive atrophy of the nasal mucosa and underlying bone. Secondary atrophic rhinitis may result from radical surgery, infections, irradiation, and trauma.
Leaking of cerebrospinal fluid will present with watery rhinorrhoea, often unilateral. It is usually associated with trauma (including surgical trauma) or neoplasia, but spontaneous leaking may occur.
Nasal neoplasms are rare; consider patients with unilateral symptoms of nasal obstruction, pain, or bleeding
History and examination
Taking a history need not be time consuming. A glance at the classification and differential diagnosis will suggest the most important questions.
Taking a history
Patient’s account of symptoms
How long has the condition been present?
Impact on lifestyle: how frequent and severe is it? Does it affect work, school, leisure time, sleep?
Seasonal or perennial?
Trigger factors: allergic or non-allergic?
Exposure to allergens through occupation or hobbies?
Allergens in the home
Does patient have history of asthma, eczema, rhinitis?
Drug or food induced?
Family history
Treatment: compliance, efficacy, side effects
What is the main symptom?
Rare, sinister causes for rhinitis need to be excluded. Unilateral symptoms should always be regarded with suspicion, particularly if associated with symptoms of increasing nasal obstruction, blood stained nasal discharge, or facial pain.
Ear, nose, and throat surgeons examine the nose with a head mirror or headlight and a nasal speculum, but increasingly this is supplemented by rigid or flexible nasendoscopy. In general practice, the nose can be examined with an auriscope fitted with the largest speculum. It is easy to confuse a large, swollen, oedematous inferior or middle turbinate with a polyp; polyps, however, unlike turbinates, are usually pale grey, translucent, and mobile and lack any sensation on gentle probing.
Investigation
Perennial allergic and non-allergic rhinitis may require no specific investigations other than skin prick testing, which has been fully discussed in an earlier article in this series. If the history or examination suggests that other factors need to be excluded, the patient may require a variety of investigations, depending on the history and clinical findings.
Special tests
In addition to routine full blood count and eosinophil count, immunoglobulin concentrations should be checked. Blood tests for antineutrophil cytoplasmic antibody and angiotensin converting enzyme may be indicated if, respectively, Wegener’s granuloma or nasal sarcoidosis is suspected. It is also important to consider whether the patient may have AIDS or be compromised by treatment with immunosupressant drugs. When skin prick tests are not available or not possible for other reasons, blood allergen specific IgE concentrations may be determined (with the radioallergosorbent test).
Imaging
Plain x ray films of the sinuses can be misleading. Computed tomography of the sinuses in the coronal plane has become the standard international imaging method.
Nasal mucociliary clearance
Nasal mucociliary clearance is assessed simply, by measuring the time taken for the patient to detect a sweet taste after a 0.5 mm particle of saccharin is placed on the mucosa of the inferior turbinate. If the test result is abnormal, further assessment of ciliary function involves taking a brushing of the nasal mucosa overlying the inferior turbinate and measuring the frequency of the beating cilia detected with a microscope attached to a photometric cell (normal range 12-15 Hz).
Nasal airway assessment
Peak nasal inspiratory flow can be measured with a modified peak flow meter. This test is easy and inexpensive to perform, but forced inspiration may be associated with significant vestibular collapse. Despite this, the results compare favourably with rhinomanometry.
Rhinomanometry records resistance in the nasal airway by measuring nasal airflow with a face mask, pneumotachograph, and pressure gradient from the front to the back of the nose via a manometer.
Acoustic rhinometry measures neither flow nor pressure, but cross sectional areas of the nasal airway. A sound pulse is passed into the nose, the reflected signal of which is recorded by a microphone and analysed in such a way that it is possible to determine the area in the nasal cavity as a function of distance.
Olfactory tests
Olfactory thresholds can be assessed by testing the patient with serial dilutions of odours such as PM-carbinol (phenylethyl methyl ethyl carbinol) (Olfacto-Labs, USA). Alternatively, “scratch and sniff” tests use cards impregnated with microencapsulated odorants. The Pocket Smell Test (Sensonics, USA), for example, presents three different odours that can be released by scratching with the tip of a pencil and choosing from a list of four possible answers. One or more incorrect reponses suggests olfactory dysfunction, and the 40 item Smell Identification Test (Sensonics) should then be administered.
Swabs, smears, and biopsies
With infective symptoms, swabs for culture and sensitivity may be useful, though a swab taken from the nose will not necessarily correlate with samples taken directly from the sinuses. Nasal smears for cytology may show high concentrations of eosinophils, and biopsies for histology may be indicated when investigating granulomatous conditions—for example, Wegener’s granulomatosis and sarcoidosis—or excluding neoplastic disease.
Treatment
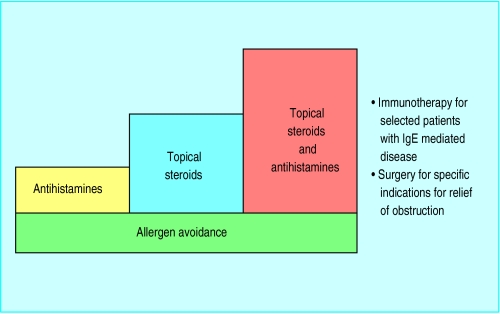
Allergen avoidance
Perennial allergic rhinitis due to house dust mite allergy may be effectively controlled by avoidance measures. Patients who are found to be allergic to animals should, if possible, avoid them completely.
Desensitisation
Desensitisation to pollen and to bee and wasp venom is highly effective
Desensitisation to house dust mite and pets, however, is less helpful and therefore seldom used in Britain
Medical treatment
Antihistamines
Antihistamines are highly effective in controlling itching, sneezing, and watery rhinorrhoea but less effective for nasal obstruction. However, they do have the advantage of controlling eye symptoms as well as nasal symptoms. The modern generation of non-sedating antihistamines are both effective and safe, although terfenadine should not be taken in conjunction with macrolide antibiotics (for example, erythromycin and clarithromycin) or antifungal agents (ketaconazole and related drugs) as serious cardiac toxicity has very rarely been reported. Topical antihistamines (for example, azelastine and levocobastine) are also effective.
Topical steroids
Topical steroids are highly effective for all symptoms of allergic and non-allergic perennial rhinitis and will usually control nasal obstruction, itching, sneezing, and watery rhinorrhoea. The modern topical steroids are safe for long term use and have no significant side effects. Treatment can be continued for several years if necessary, and alternative medical or surgical treatment need be considered only if symptoms fail to respond. Occasionally, topical steroids may be associated with dryness, crusting, and bleeding from the nose, in which case treatment should be discontinued for a few days and then restarted.
Sodium cromoglycate
Sodium cromoglycate is more effective in atopic than non-atopic patients. It has no known side effects but is less effective than antihistamines and corticosteroids and does require frequent use (up to five times daily), which may compromise compliance. Topical sodium cromoglycate eye drops are highly effective for allergic conjunctivitis. Topical nedocromil eye drops are also effective and have a longer duration of effect (up to 12 hours).
Surgical treatment
The first line of treatment for allergic or non-allergic perennial rhinitis is usually medical
When drugs fail, surgery may be indicated
Surgical reduction of the inferior turbinates or correction of a deviated nasal septum or nose may be required to improve the airway or at least to improve access for topical medical treatment
Surgery continues to have a major role in the management of nasal polyps and sinusitis when these conditions fail to respond to medical treatment
The management of nasal polyps and sinusitis has improved with the introduction of minimally invasive endoscopic sinus surgery
Topical anticholinergics
Ipratropium bromide is effective in controlling watery rhinorrhoea, particularly if this is the only symptom. The dose may need to be titrated against symptoms.
BMJ 1998;316;917-20
Nasal decongestants
Topical nasal decongestants may be useful at the start of treatment to “open up” the nose and improve penetration of topical corticosteroids, when flying, or for upper respiratory tract infections. They should only be used for short courses (preferably no more than 2 weeks), however, to avoid the risk of developing “rhinitis medicamentosa” (rebound congestion).
Further reading
Lund V, Aaronson D, Bousquet J, Dahl R, Davies RJ, Durham SR, et al. International consensus report on the diagnosis and management of rhinitis. Allergy 1994;49(suppl 19)
Sibbald B, Rink E. Epidemiology of seasonal and perennial rhinitis. Clinical presentation and medical history. Thorax 1991;46:859-901
Fleming DM, Crombie DL. Prevalence of asthma and hayfever in England and Wales. BMJ 1987;294:279-83
Durham SR, Mackay IS. The nose. In: Brewis RAL, Corrin B, Geddes DM, eds. Respiratory medicine. 2nd ed. Vol 2. London: Saunders, 1995:1006-14
Figure.
Nasal cavity showing ostiomeatal complex. It is the final common pathway draining the maxillary sinus, the anterior ethmoidal sinus, and the frontal sinus
Figure.

Nasal polyp
Figure.
Computed tomogram of normal paranasal sinuses
Figure.
Computed tomogram of paranasal sinuses with increased opacity of maxillary and ethmoidal sinuses and obstruction of ostiomeatal complex
Figure.

Modified peak flow meter for measuring peak nasal inspiratory flow
Figure.
Rhinomanometry: flow is recorded via a face mask and pneumotachograph, and pressure change is measured with a manometer via a tube either to one nostril (unilateral) or through the mouth to the back of the nose (bilateral)
Figure.
Acoustic rhinometry measures cross sectional areas of the nasal airway
Figure.
Stepwise approach to treatment of perennial rhinitis
Footnotes
I S Mackay is a consultant ear, nose, and throat surgeon at the Royal Brompton Hospital and Charing Cross Hospital, London.
The ABC of allergies is edited by Stephen Durham, honorary consultant physician in respiratory medicine at the Royal Brompton Hospital, London. It will be published as a book later in the year.