Editorial on the Research Topic Reviews in cardiac rehabilitation
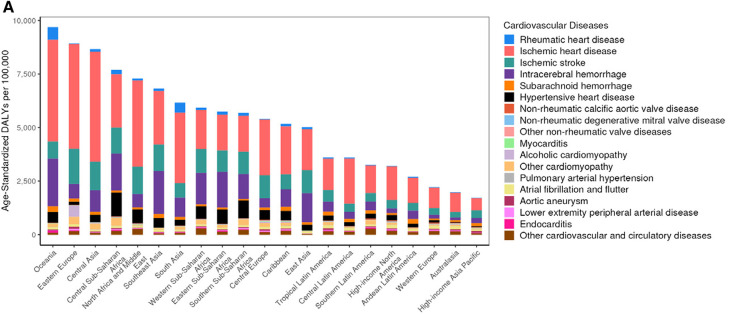
Cardiovascular disease (CVD) is a global issue and global deaths from CVD continue to increase (1) (Figure 1). Cardiac Rehabilitation (CR) is a proven interdisciplinary modality based on counseling and physical training aimed to improve exercise capacity and cardiovascular (CV) morbidity and mortality amongst several CVDs (3–5). International guidelines recommend CR with Class I Level of recommendation A/B (based on the diseases) to support its use (6). Most of the leading causes for CVD (Figure 1) would benefit with the intervention of CR (1). However, despite these findings, CR is globally underutilized. This is due to both system and personal barriers, leading patients to not participate or complete a CR program. In addition, there are some groups of patients (i.e., women, elderly patients, and ethnic minorities) in which CR is less prescribed or less used (7). System level barriers include cost, time availability (of both the CR programs and patients), transportation, and personal preference (8). In addition, in the last years, the COVID-19 pandemic made the situation even worse, adding a further barrier in attending or completing CR; indeed, most programs were temporarily closed during the pandemic and several never reopened after the pandemic (9). However, to overcome these limitations, further alternative options to the in-person CR programs have been suggested, with equivalent benefits, safety, and patient satisfaction (10, 11). Alternative options include: Virtual CR (all CR components done via a virtual and on-demand platform), Hybrid (a blend of in-person and virtual), and a home-based CR (12). Compared to traditional CR programs, hybrid models of CR offer several potential advantages. They facilitate eligible patients who are unable to visit rehabilitation centers for various reasons (eliminating the “CR deserts”), decrease medical costs, and improve patient satisfaction and adherence to CR.
Figure 1.
Reprinted from Mensah et al. (2). Copyright (2023), with permission from Elsevier.
In this context, in the present issue of the Frontiers in Cardiovascular Medicine Journal, several manuscripts have been published, dwelling upon various topics related to CR.
In the Western countries, as well as several other industrialized countries, the importance of disease prevention is resulting in a shift in thought, knowledge, and resources. For instance, The Million Hearts Campaign is a national initiative co-led by the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare & Medicaid Services (CMS) taking-action to have at least 70% of eligible patients participate in CR (13, 14). In parallel, in the context of a call for health policymakers to reset the priorities of healthcare resources and provide adequate preventative care, the Chinese government approved the plan named “Healthy China 2030,” which aims to improve national health and prevent disease in China (Zhang et al.). However, despite efforts to increase the availability of CR programs in China, the growth has been slow. In the present issue, Zhang et al. extracted data on 19,896 patients from the online registry platform of the China Society of Cardiopulmonary Prevention and Rehabilitation from February 2012 to December 2021. In this investigation, as in other countries, men and younger patients were more frequently enrolled in CR (15–18). Notably, despite China also having similar system and personal barriers to getting patients referred and enrolled into CR programs, most patients preferred a hospital-based CR. In addition, this investigation pointed out the “CR deserts”, with CR programs being less prominent in the rural areas of China and being offered at tertiary care centers. These issues have resulted in the majority of the Chinese patients diagnosed with CVD being unable to heed the benefits of CR. These disparities will result in a haves and have-not implementation and participation in CR (Zhang et al.).
There are various components of a CR program, which includes exercise, nutrition, psycho-social issues, CV risk factor modification, and education. However, not all of the exercise regimens fit all patients. Therefore, exercise must meld into the individual patient's lifestyle. Efforts to offer various types of exercises must be made, to increase the sustainability and to individualize the exercise regimen. As an example, High intensity interval training (HIIT) is specifically embraced by more elite athletes and women (19) and strength training to rebuild lost skeletal muscle is key for heart failure (HF) patients (20). Furthermore, exercises must be culturally varied in order to embrace our patient's needs.
In the present issue, Zhang et al. performed a meta-analysis of randomized controlled trials aimed to evaluate the effects of Traditional Chinese Exercises (TCE)—such as Tai Chi, Qi Gong, and Ba Duan Jin in patients with myocardial infarction (MI). TCE has become increasingly popular around the world because of their gentle movements, low-risk, easy training, and long-term adherence (Zhang et al.). As a mild muscle- strengthening sport, TCE combines spiritual meditation with moderate postures, musculoskeletal stretching, and deep breathing (21, 22). TCE has been shown in numerous studies to be an effective exercise for CR and to enhance cardiorespiratory health (23, 24). In this investigation based on 21 studies involving 1,890 patients, Zhang et al. showed that the use of TCE was an effective form of exercise in patients after an MI to prevent subsequent CV events and improve patient's emotions and quality of life (QoL) (Zhang et al.).
Heart failure (HF) incidence is increasing (20, 25). HF with reduced ejection fraction (HFrEF) <35% is a qualifying diagnosis that for many is covered by insurance and Medicare. Unfortunately, Medicaid coverage for CR is quite variable from state to state within the United States (US) with very limited CR coverage. Despite heart failure with preserved ejection fraction (HFpEF) increasing, especially in the elderly and women, it is not covered for CR (20, 25). As a set of Tai Chi exercises designed specifically for elderly patients with chronic heart failure, Fu Yang Tai Chi exercises are ideal. Fu Yang Tai Chi stems from the traditions of Tai Chi and incorporates a holistic approach melding the body, mind, and breath, “emphasizing the importance of spiritual care in moderate exercise, realizing the combination of “exercise prescription” and “psychological prescription.” The whole set of movements is even and slow, combining movement and stillness, and is a unique connotation of aerobic physical and mental exercise” (Jiao et al.). However, there are no clinical trials to confirm the effectiveness and safety of the exercises; therefore, Jiao et al. designed a single-center, open label, randomized controlled trial (RCT) to study the effects of Fu Yang Tai Chi as an adjunctive therapy on the QoL of elderly patients with HF. If the results are positive, this therapy could become a good way for older people with HF to exercise at home that is also affordable (Jiao et al.).
In conclusion, the lack of utilization of CR for patients with CVD as a resource to prevent disease is adding insult to injury, salt to the wound. The knowledge is abundant for the benefits of CR to prevent subsequent events in patients with CVD. The COVID pandemic brought to the surface the great need, benefit, efficacy, and safety of alternative options of traditional CR to expand the benefit to the masses of patients with CVD. This global awareness is occurring now. The effects and outcomes will decrease CV events, reduce the barriers to receive CR, and improve CV morbidity and mortality.
Author contributions
MT: Writing – original draft, Conceptualization, Validation, Writing – review & editing. CM: Validation, Writing – review & editing. AS: Validation, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Roth GA, Mensah GA, Fuster V. The global burden of cardiovascular diseases and risks: a compass for global action. J Am Coll Cardiol. (2020) 76(25):2980–1. 10.1016/j.jacc.2020.11.021 [DOI] [PubMed] [Google Scholar]
- 2.Mensah AG, Fuster V, Murray CJL, Roth GA, Mensah GA, Abate YH. Global burden of cardiovascular diseases and risks, 1990–2022. JACC. (2023) 82(25):2350–473. 10.1016/j.jacc.2023.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. (2009) 54(1):25–33. 10.1016/j.jacc.2009.01.078 [DOI] [PubMed] [Google Scholar]
- 4.O'Connor GT, Buring JE, Yusuf S, Goldhaber SZ, Olmstead EM, Paffenbarger Jr RS, et al. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation (1989) 80(2):234–44. 10.1161/01.cir.80.2.234 [DOI] [PubMed] [Google Scholar]
- 5.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. (2001) (1):CD001800. 10.1002/14651858.CD001800 Update in: Cochrane Database Syst Rev. 2011;(7):CD001800. [DOI] [PubMed] [Google Scholar]
- 6.Drozda J, Messer JV, Spertus J, Abramowitz B, Alexander K, Beam CT, et al. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American college of cardiology foundation/American heart association task force on performance measures and the American medical association-physician consortium for performance improvement. Circulation (2011) 124(2):248–70. 10.1161/CIR.0b013e31821d9ef2 Erratum in: Circulation. 2011 Jul 12;124(2):e39 [DOI] [PubMed] [Google Scholar]
- 7.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic variation in cardiac rehabilitation participation in medicare and veterans affairs populations: opportunity for improvement. Circulation. (2018) 137(18):1899–908. 10.1161/CIRCULATIONAHA.117.029471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, Koepsell E, et al. Barriers to participation in cardiac rehabilitation. Am Heart J. (2009) 158(5):852–9. 10.1016/j.ahj.2009.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pecci C, Ajmal M. Cardiac rehab in the COVID-19 pandemic. Am J Med. (2021) 134. 10.1016/j.amjmed.2021.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schopfer DW, Whooley MA, Allsup K, Pabst M, Shen H, Tarasovsky G, et al. Effects of home-based cardiac rehabilitation on time to enrollment and functional Status in patients with ischemic heart disease. J Am Heart Assoc. (2020) 9(19):e016456. 10.1161/JAHA.120.016456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brewer LC, Abraham H, Kaihoi B, Leth S, Egginton J, Slusser J, et al. A community-informed virtual world-based cardiac rehabilitation program as an extension of center-based cardiac rehabilitation: mixed-methods analysis of a multicenter pilot study. J Cardiopulm Rehabil Prev. (2023) 43(1):22–30. 10.1097/HCR.0000000000000705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keteyian SJ, Ades PA, Beatty AL, Gavic-Ott A, Hines S, Lui K, et al. A review of the design and implementation of a hybrid cardiac rehabilitation program: an expanding opportunity for optimizing cardiovascular care. J Cardiopulm Rehabil Prev. (2022) 42(1):1–9. 10.1097/HCR.0000000000000634 [DOI] [PubMed] [Google Scholar]
- 13.Ritchey MD, Loustalot F, Wall HK, Steiner CA, Gillespie C, George MG, et al. Million hearts: description of the national surveillance and modeling methodology used to monitor the number of cardiovascular events prevented during 2012–2016. J Am Heart Assoc. (2017) 6(5):e006021. 10.1161/JAHA.117.006021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright JS, Wall HK, Ritchey MD. Million hearts 2022: small steps are needed for cardiovascular disease prevention. JAMA—J Am Med Assoc. (2018) 320(18):1857–8. 10.1001/jama.2018.13326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li S, Fonarow GC, Mukamal K, Xu H, Matsouaka RA, Devore AD, et al. Sex and racial disparities in cardiac rehabilitation referral at hospital discharge and gaps in long- term mortality. J Am Heart Assoc. (2018) 7:e008088. 10.1161/JAHA.117.008088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grace SL, Oh PI, Marzolini S, Colella T, Tan Y, Alter DA. Observing temporal trends in cardiac rehabilitation from 1996 to 2010 in Ontario: characteristics of referred patients, program participation and mortality rates. BMJ Open. (2015) 5(11):e009523. 10.1136/bmjopen-2015-009523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grace SL, Shanmugasegaram S, Gravely-Witte S, Brual J, Suskin N, Stewart DE. Barriers to cardiac rehabilitation: does age make a difference? J Cardiopulm Rehabil Prev. (2009) 29(3):183–7. 10.1097/HCR.0b013e3181a3333c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. (2002) 16(5):541–52. 10.1191/0269215502cr524oa [DOI] [PubMed] [Google Scholar]
- 19.Way KL, Reed JL. Meeting the needs of women in cardiac rehabilitation: is high-intensity interval training the answer? Circulation. (2019) 139(10):1247–8. 10.1161/CIRCULATIONAHA.118.037754 [DOI] [PubMed] [Google Scholar]
- 20.Pandey A, et al. Exercise intolerance in older adults with heart failure with preserved ejection fraction. JACC. (2021) 78(11):1166–87. 10.1016/j.jacc.2021.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeng ZP, Liu YB, Fang JJ, Liu Y, Luo J, Yang M. Effects of baduanjin exercise for knee osteoarthritis: a systematic review and meta-analysis. Complement Ther Med. (2020) 48:102279. 10.1016/j.ctim.2019.102279 [DOI] [PubMed] [Google Scholar]
- 22.Zhou ZL, Zhou RZ, Li KP, Zhu Y, Zhang ZQ, Luo Y, et al. Effects of tai chi on physiology, balance and quality of life in patients with type 2 diabetes: a systematic review and meta-analysis. J Rehabil Med. (2019) 51(6):405–17. 10.2340/16501977-2555 [DOI] [PubMed] [Google Scholar]
- 23.Yang YL, Wang YH, Wang SR, Shi PS, Wang C. The effect of tai chi on cardiorespiratory fitness for coronary disease rehabilitation: a systematic review and meta-analysis. Front Physiol. (2018) 8:1091. 10.3389/fphys.2017.01091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gu Q, Wu SJ, Zheng Y, Zhang Y, Liu C, Hou JC, et al. Tai chi exercise for patients with chronic heart failure: a meta-analysis of randomized controlled trials. Am J Phy Med Rehabil. (2017) 96(10):706–16. 10.1097/PHM.0000000000000723 [DOI] [PubMed] [Google Scholar]
- 25.Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. (2018) 391(10120):572–80. 10.1016/S0140-6736(17)32520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]